Published online Jul 18, 2015. doi: 10.5312/wjo.v6.i6.469
Peer-review started: March 28, 2015
First decision: April 10, 2015
Revised: April 23, 2015
Accepted: May 16, 2015
Article in press: May 18, 2015
Published online: July 18, 2015
The majority of orthopaedic surgeons even currently agree that primary total arthroplasty in valgus knees with a deformity of more than ten degrees may prove challenging. The unique sets of bone and soft tissue abnormalities that must be addressed at the time of the operation make accurate axis restoration, component orientation and joint stability attainment a difficult task. Understanding the specific pathologic anatomic changes associated with the valgus knee is a prerequisite so as to select the proper surgical method, to optimize component position and restore soft-tissue balance. The purpose of this article is to review the valgus knee anatomical variations, to assess the best pre-operative planning and to evaluate how to choose the grade of constraint of the implant. It will also be underlying the up-to-date main approaches and surgical techniques be proposed in the English literature both for bone cuts and soft tissue management of valgus knees.
Core tip: Knee arthroplasty in valgus deformity more than 10° is an orthopaedic challenge. During the operation, due to the deformities of the bone and soft tissue, there are many difficulties for the surgeon, such as the restoration of the mechanical axis, the orientation of the component and the stability of the knee joint. Our aim is to review the valgus knee anatomical variations, to assess the best approach and surgical technique for bone cuts and soft tissue management of valgus knees so as to succeed the best result.
- Citation: Nikolopoulos D, Michos I, Safos G, Safos P. Current surgical strategies for total arthroplasty in valgus knee. World J Orthop 2015; 6(6): 469-482
- URL: https://www.wjgnet.com/2218-5836/full/v6/i6/469.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i6.469
Of the patients requiring a primary total knee arthroplasty (TKA), 10% to 15% present with valgus deformity (VD), the inaccurate correction of which continues to be a challenge for the orthopedics even currently[1]. Excessive pre-operative malalignment predisposes to a greater risk of failure compared to well-aligned knees[2]. It is observed that the restoration of the correct lower limb mechanical axis postoperatively; as also the normal balance of the soft tissues are important for the final outcome of these joint replacement operations[2-5]. Thus, the severely valgus deformed knees are related with a worse outcome vs their varus counterparts[5].
There are different and multifactorial etiologic parameters of knee VD, from congenital to secondary such as primary osteoarthritis. To be more specific, in adults VD is commonly associated with inflammatory arthritis (rheumatic diseases) as well as with primary osteoarthritis, posttraumatic arthritis (as a result of a tibial malunion, physeal arrest, or tibial plateau fracture), or even overcorrection from a proximal tibial osteotomy performed to correct a preexisting varus deformity[2,6]. Nevertheless, a significant percentage of adults with lateral compartment osteoarthritis and associated VD represent unresolved physiologic valgus deformity. Occasionally, persistence of genu valgum from childhood may exist secondary to metabolic disorders, such as rickets and renal osteodystrophy[7]. Overwhelmingly, the most common etiology of VD is primary osteoarthritis with a smaller number of patients having rheumatoid arthritis and posttraumatic arthritis; whereas other inflammatory disorders and osteonecrosis are scarce etiologies based on the main clinical series that utilized TKA in patients with knee VD the last two decades[1-5,8-16].
The valgus knee may have any combination of primary or secondary abnormalities even osseous (acquired or preexisting bony anatomic deficiencies) or soft-tissue (lateral and medial). These include on the one hand contraction of the lateral capsule and lateral soft tissues and ligaments; and on the other hand lax medial structures. This constellation of pathology makes attaining soft-tissue balance when the knee is returned to physiologic alignment extremely difficult[2,4,6]. More specifically, the contracted structures are the lateral collateral ligament (LCL), the posterolateral capsule (PLC), the iliotibial band (ITB) and lastly the popliteus tendon. Rarely, there are also affected the long head of the biceps femoralis in addition to the lateral head of the gastrocnemius muscle. Some authors also further described a posterior cruciate ligament (PCL) alteration in valgus knees, but in the literature its influence in maintaining the deformity is not universally accepted[2]. Thus, the knee medial side of the stabilising structures is attenuated. Unlike its varus counterpart, most of the bone defects are found on the lateral femoral condyle, consisting of cartilage erosion, or hypoplasia of the lateral condyle and remodeling of the femur metaphysis, while the plateau of the tibia is generally less affected[2,3,8-10]. The described deformities can lead to a tibial external rotation and to patellar lateral subluxation tendency[11].
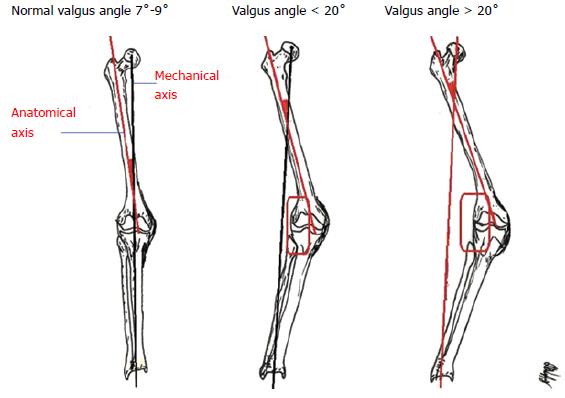
In 2005, Ranawat et al[1] described three grades of VD. More specifically, Grade-I occurs in 80% of the patients, whereas the mechanical axis deviation is less than 10° and it is passively correctable. In Grade-I the medial collateral ligament (MCL) is intact. Grade-II accounts for 15%; is characterized by a range of axis deviation 10° to 20°, whereas the MCL is functional thought elongated. Grade-III is seen in the remaining 5% of the patients having axis deviation more than 20°. The medial stabilising elements are typically not functional so a constrained implant is often required[1,10] (Figure 1).
To understand the important anatomic changes in valgus deformed knees is absolutely helpful so as to choose the best surgical method, to optimize correct component position and restore gap and soft-tissue balancing. Over the last 25 years, different approaches and soft-tissue procedures have been proposed for TKA with VD, having the purpose to restore the limb’s mechanical axis. The objective of this article is to give an overview of the most common approaches, to analyze the different techniques of succeeding anatomical or mechanical axis restoration, soft tissue and gap balance and lastly to present the literature up-to-date long term results.
During standard physical examination for end-stage degenerative knee disease the orthopaedic physician should observe the patient’s gait, in order to identify other dynamic instabilities and assess the lower limb alignment both in the supine and weight-bearing positions. Any sagittal deformity, such as fixed flexion contracture or recurvatum, as well as any rotational deformity, should be attended. It should also be measured the range of motion; and further evaluated the status of the extensor mechanism and the patellofemoral articulation[2,6,11,17].
Furthermore, clinical examination plays a major role for the surgeon so as to determine even if the deformity is correctable or fixed, and whether the knee is stable or unstable. The knee should be further evaluated for anteroposterior laxity, coronal and sagittal deformity, and mediolateral instability[3]. It is very crucial to assess if VD is fixed (Ranawat Grade III) or still reducible (Ranawat Grade II or I). In a fixed deformity, the lateral structures are tight and require release. In cases with non-functional MCL and when the release of the lateral structures has fulfilled, the use of a constrained prosthesis may be necessary. If the deformity is reducible, soft tissue release will be less invasive, and a standard unconstrained prosthesis could be sufficient. The orthopaedic surgeon would lastly perform a neurovascular examination to differentiate a possible lumbosacral or vascular disease[2,9-11].
After the clinical assessment, the mandatory pre-operative planning radiographs that should be included are: (1) a weight-bearing knee anteroposterior view; (2) a lateral; and (3) a patella merchant view. Furthermore, the limb axis deviation measurement with long standing film views or CT-scan with anterior orientation of the patella is also often needed[3]. It has been shown that rotation up to 20˚ has little effect on the measurement of the femorotibial axis deviation[18].
Based to our experience, in cases of serious bone stock deficiency a knee computer tomography will be helpful. Attention should be focused on the hypoplastic lateral femoral condyle, the eroded posterior femoral condyle and the remodeled femoris or tibial metaphysis that can lead to malaligned or malrotated positioned component on the femur. The patellofemoral joint may also be partially dislocated. A precise profile X-ray of the knee will help to assess the tibial slope, and the patellar height (alta or baja) according to the Insall-Salvati ratio. Besides, the patellofemoral view at 30° will add to the evaluation of patellar centering by classifying three states (centered, subluxation, luxation)[2,11,19].
A weight-bearing long leg view is fundamental for the evaluation of lower limb alignment (mechanical and anatomical axis), measure the VD level and plan the amount of correction (templating). In order to determine the amount of VD knee medial instability stress radiographs could be also used[2]. A electromyogram should be made in any case of lower limb dysesthesias that may be attributed to lumbosacral disease [2,11] (Figure 2).
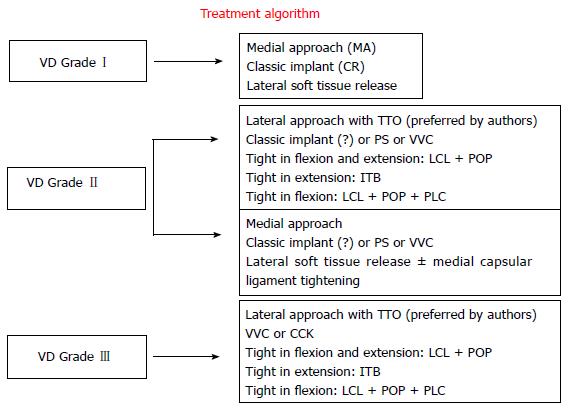
The implant selection should be carried out pre-operatively, based on the radiological and clinical evaluation, but the final decision should be taken after the bone cuts and knee soft-tissue balancing. There will always be plane A and plane B in the selected prosthesis with regard to the degree of component constraint, especially in severe VD total knee arthroplasties.
Ideally, if proper soft-tissue balance is restored, a minimally constrained component can be implanted. Although most surgeons agree that a posteriorly stabilized (PS) component should be used if significant deformity necessitates PCL sacrifice for soft-tissue balancing, it is not universally accepted[6]. PS-TKA prosthesis provides some degree of posterior stabilization as well as protection against posteromedial and posterolateral translation, but it will not protect against residual medial laxity, which is one of the major considerations in achieving proper balance in VD knees[9,10,17].
The debate in VD, PS vs cruciate-retaining (CR) implants has to do with the PCL, which is not rarely contracted and it possibly will limit the VD correction[10,20]. In some cases it may be more difficult to obtain the deformity correction with an intact PCL, since the PCL presence contributes to the deformity on frontal level[21,22]. Besides, on the one hand the PS design is more stable than a CR one, due to the post-cam mechanism; and on the other hand the PS allows greater lateralization of the knee arthroplasty components, which improves patellar tracking[1,2]. For these reasons some surgeons suggest in VD knees to substitute a contracted PCL with a PS design as simplest as to stabilize it by using a CR implant[6].
Besides McAuley et al[23] presented that CR implants may possibly be used in different variations of VD arthritic knees in which the implant survival is improved when the LCL and/or the popliteus tendon (POP) are preserved. The likelihood of revision is POP increased by 19.9 times, when release of both the LCL and POP is performed, because of more mediolateral laxity.
Another debated issue is the amount of constraint needed to balance a valgus knee. Favorito et al[6] proposed that the surgeon should resist the temptation, when possible, to move to a more highly constrained prosthesis, such as a totally stabilized prosthesis, to compensate for shortcomings in achievable soft-tissue balancing. Although highly constrained components may be necessary in difficult revision cases, they are infrequently necessary for primary TKA. The problem is that in severe VD knees the PCL may be stretched or elongated, which means nonfunctional and these knees require either an ultra-congruent (VVC or hinged) or PC component.
Furthermore, in valgus knees with extreme deficiencies of the lateral femoral condyle, the usage of component augmentation blocks may be required. In cases that the lateral femoral condyle has very little or no distal femoral bone resection or, likewise, from the chamfer and posterior cuts; then these cuts might require component augmentation[4,6]. Though, if the femoral component is being press-fit, then as long as native bone is resting on one of the chamfer cuts (as is usually the case for the posterior bevel or chamfer cut), then the remaining defect can be filled with autograft bone taken from the other cut bone in the procedure[1,6].
To understand the ‘‘typical’’ operative procedure in valgus knee, it should be considered that the lateral stabilizers, which may hinder reduction, are of two types. On the one hand, those inserting near the flexion-extension axis (LCL and popliteal tendon), acting in both extension and flexion of the knee; and on the other hand those inserting remotely with respect to the axis (fascia lata, posterolateral articular capsule, biceps and external gastrocnemius muscles), acting only in extension[24].
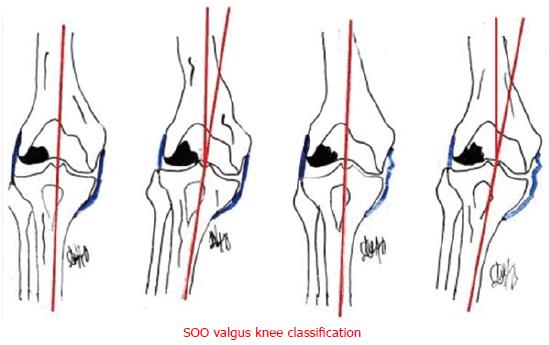
The sequencing of lateral release is controversial, with many and various protocols of progressive step-wise release. Based on the SOO classification presented in 2003 (Societe d’Orthopedie de l’Ouest - Western France Orthopedics Society), four types of valgus knee of increasing surgical difficulty has been distinguished. Type I, can be completely reduced, without medial laxity, posing no particular problem and a medial approach is possible; but in case of patellar dislocation, it is recommended a lateral approach. Type II is totally or partially irreducible, but without medial laxity, and is the most frequent; lateral release is required, whereas Type III is reducible, but with medial distension laxity, and may require management of the medial laxity. Lastly, Type IV is irreducible, with medial distension laxity, combining the problems of types II and III[24] (Figure 3).
Keblish[11] was the first, in 1991, to recommend a lateral capsular approach for valgus knee arthroplasty, in addition to Buechel[25] who refined the technique. It has been proved unpopular due to the technical difficulties and demands of the elevation of the tibial tubercle. Nevertheless, Whiteside[26], in 1993, and Burki et al[27] in 1999, showed their outcome in valgus deformed knees after lateral approach and tibial tubercle osteotomy (TTO). A disadvantage of this approach is the osteotomy of the tibial tuberosity which is necessary for patellar eversion. Fiddian et al[28] presented in 1998 a modified lateral capsular approach with repositioning of vastus lateralis in valgus knee arthroplasties with very good results.
Keblish[11] described a lateral incision along the lateral quadriceps border, taking care to leave 1 cm of the lateral retinaculum, from the junction between the vastus lateralis and the quadriceps tendon to the patella, through 50% of the tendon. During lateral closure, if there were difficulties, he proposed two different tricks to facilitate it: (1) approximation of the infrapatellar fat pad to the patella ligament; and (2) separation of the vastus lateralis from the rectus femoris, followed by suturing together the two tendons in a staggered position[11].
In the anterolateral approach, as detailed described by Nikolopoulos et al[4], a straight 8-10 cm midline skin incision is performed and a lateral parapatellar capsulotomy follows. The ITB is elevated carefully from Gerdy’s tubercle. In order to medially displace the patella, TTO is performed laterally, leaving the soft tissues intact medially. The osteotomy length measures 5 to 6 cm; whereas proximally, at the upper part of the patellar tendon insertion, the oblique proximal part of the osteotomy prevents proximal migration. The tibial tubercle is medially hinged hence the knee joint surface is widely exposed (Figure 4).
Tibial cut is done - directing the level of the resection perpendicular to its longitudinal axis. The resection should be from 6 to 8 mm in the medial compartment and always has to be performed after having removed all the osteophytes, especially in the lateral side of the tibial plateau. In cases that the bone in the tibial plateau is severely deformed, then almost no bone is resected on the lateral side to avoid medial over-resection or malaligned cuts[2].
The distal femoral cut is performed in 3° of valgus in relation to the femoral axis. The distal femoral cut at 3° only, instead of 5° to 7° that applies in varus knees, protects against under-correction. During TKA for VD, it is proposed to put the prosthesis a slightly more varus so as to counteract any tendency for valgus recurrence[11]. Caution is taken not to over-resect the lateral femoral condyle to avoid marked elevation of the joint line[4]. Rossi et al[2] proposed minimal (1-2 mm) or absent of lateral condyle distal femoral resection in severe valgus deformity of the distal femur. Femoral resection should be no more than 10 mm in the medial condyle (usually 7-8 mm). The surgeon has to pay also attention to the lateral condylar hypoplasia that can determine a great intra-rotation of the components if a posterior reference is used[2]. In order to perform the femoral cut in a correct orientation the Whiteside AP axis and the epicondyle axis are used[3,4]. Considering this aspect, Arima et al[29] support the utility of using the anteroposterior axis in order to give the proper femoral rotation in valgus anatomy. In cases of severe trochlear dysplasia, where the Whiteside line can be extremely difficult to identify, then the epicondylar axis or parallel to the tibial cut technique should be used to assess a correct femoral rotation[2].
At this stage, sub-periosteal elevation of the POP and LCL from the epicondyle is performed in stages, namely for knees be tight in flexion. The PLC release can be performed in cases of tightness both in flexion and extension. During closure, the tibial tuberosity as a rule is fixed to its original position; or slightly more medially in cases that the patella tends to track laterally and dislocate, so tibial tubercle transfer is necessary for satisfactory alignment. Tibial tubercle fixation can be performed with three wire loops (preferred) or with 2 cortical screws (4.5 mm). Oblique direction of the wire loops offers better resistance to proximal directed forces[4]. Patellar tracking was finally checked with the “no-thumb” test.
According to the surgeons[1-4] preferring the anterolateral procedure, the main reasons and advantages are: (1) the lateral release, most usually necessary in valgus knees, is part of the approach. In the alternative case of medial arthrotomy, the vascular supply of the extensor mechanism is seriously impaired; (2) the lateral approach facilitates the release of the lateral contracted elements, offering better surgical view; and (3) the possibility to medicalize the tubercle, if required, improving this way the patellar tracking[2,4].
The standard approach performed by the majority of orthopaedic surgeons even in the valgus knee and without contraindications is the anteromedial[1,4,25,30]. A straight midline incision with a medial parapatellar arthrotomy is made. The tibial and femoral bone cuts followed the same technique as the one described in the anterolateral approach. In order to achieve optimal soft tissue balancing, in knee extension the contracted ITB is released even by elevating it form Gerdy’s tubercle or by ITB lengthening with multiple stab wounds. If additional release is needed, then the LCL and popliteus is slightly released or lengthened from the distal part of the femur[4]. In most cases with mild to severe VD, the PLC is further released. If the PLC is released, that is done either in flexed knee from the distal part of the femur, by using a curved osteotome; or in fully extended knee by fractionally lengthening with multiple stabs punctures (“pie crust” technique)[1,30]. Finally, the patellofemoral tracking is improved with lateral retinacular release. Tracking of the extensor mechanism is again evaluated with use of the appropriate lift-off test[3,4].
The medialis approach main disadvantage is the difficulty to reach the PLC during the lateral soft tissue release. In addition, patellar vascular damage has been described when a medial parapatellar approach is combined with a lateral release[25].
Lateral soft tissue: Despite the agreement in the literature that lateral structure release is necessary in VD, there is an open debate on which are the best sequence and the best technique to perform those releases. In the abovementioned part it was presented our experience - based on our publications on the subject of valgus knee arthroplasty[3,4] - in accordance with the main ideas of other researchers[11,25-28,31-33]. In that part it would be analyzed more detailed the literature different proposals for soft tissue balancing of the retracted lateral structures of valgus deformed knees.
The releases should be performed in fully extended knee by using lamina spreaders to check the tension of the medial and lateral compartments. After each release the surgeon should evaluate the alignment and the stability of the knee, in order to achieve a symmetrical rectangular extension and flexion gaps with the spacer block in situ[2,34].
Krackow et al[10] presented firstly the release of the ITB and the LCL in the type I valgus knee, followed by the PLC, POP and the gastrocnemius muscle lateral head, when necessary, while in type II valgus deformities a medial ligamentous reconstruction was also proposed, which consisted of either proximal or distal advancement of the medial ligament mechanism according to the surgeon’s preference. The same period Buechel[25] presented a sequential three-step lateral release during TKA, for correcting fixed valgus deformed knee which included elevation: (1) the ITT from Gerdy’s tubercle; (2) the LCL and PT; and (3) the entire periosteum of the fibular head.
Ranawat et al[1] described a stepwise technique in which the first structure to be released is the PCL; and thereafter a PLC intra-articular release by using an electrocautery at the level of the tibial cut surface. When necessary the ITB is released with multiple “inside-out” stab incisions, as well as the LCL. These multiple transverse stab incisions a few centimeters proximal to the joint line of the ITB with a no. 15 surgical blade, lengthens as necessary the lateral side from the inside with the so-called “pie-crusting” technique. On the contrary the POP is normally preserved[1]. Pie-crust technique has also been performed by Clarke et al[35] and Aglietti et al[36] with excellent results. It is believed that the pie-crust is a reliable technique to correct moderate to severe fixed valgus deformed knees with excellent results and limited complications. The multiple punctures have the following advantages: (1) allow gradual stretching of the lateral soft tissues; (2) reduce the risk of PLC instability; and (3) Maintain the POP tendon[36]. Lastly, one of the disadvantages of this technique is the potential risk of peroneal nerve lesion[1,35,36].
Bruzzone et al[37], in a cadaveric study, concluded that the nerve is at risk during the PLC release, in the triangle defined by the POP, the surface of the tibial cut and the ITB posterior fibres (“danger zone”), but not during the ITB pie-crust technique (“safe zone”).
Favorito et al[6] proposed that due to the fact that the LCL is the tightest structure more commonly, then it is the first structure to be released. The next sequential release follows is the POP (an important structure for rotational and valgus stability in flexion), the PLC, the femoral insertion of the LHG and, finally, the ITB.
Whiteside LA described a soft tissue release sequence based on the anatomic function of ligaments in flexion and extension consistently. A ligament attached to the femur near the epicondyles, so near the axis through which the tibia rotates and the knee flexes and extends, has an important role in flexion stability. On the other hand, a ligament attached far away from the epicondyle is more important for the extension knee stability. Thus, more specifically, for tight knees both in flexion and extension, the LCL and POP tendon are released. For those knees that tightness remains in extension ITB release is needed. Posterior capsular release is performed only when necessary for persistent lateral ligament tightness[38].
Krackow et al[39] published a cadaveric study, in 1999, in which it was studied the correction amount achieved in each step of release of two different sequences, comparing it in flexion and extension. The sequences were on the one hand ITB, POP, LCL and LHG; and on the other hand LCL, POP, ITB and LHG. They evaluated the amount of correction at 0°, 45° and 90° of flexion. The results showed that the greatest varus rotation occurred once all structures were released, with the LHG origin last in both groups. Moreover, the largest increase occurred after the release of the LCL. It was concluded that in severe VD, the LCL should be released first; whereas POP and ITB should be released step-by-step according to the soft tissue balancing needs[39].
Boyer et al[40] give emphasis to the fact that the lateral approach in valgus TKA allows the ITB elevation from the Gerdy’s tubercle in continuity with the anterior compartment fascia, and the release of the lateral part of the femur attachments. Was the knee tight in extension after ITB release, then additional releases was performed? If PLC was tight, it was detached from the posterior condyles or transected at the tibial cut level from PCL insertion to the PLC. If this was insufficient, gastrocnemius and biceps tendon release could be considered[40].
An alternative technique for lateral structure release has been described by Brilhault et al[41] associated with a lateral parapatellar approach. A sliding osteotomy of the femoral LCL and POP insertions is done and the resulting bone block is mobilized and placed more distally. This procedure produces a rectangular space and had great results in Bremer et al[42]’s study, as there was no need for semi-constrained or constrained prosthesis. Mullaji et al[43] described a similar technique in which, after the release of the PLC and the ITB, they performed a computer navigated lateral epicondylar osteotomy, with a more accurate repositioning of the epicondyle. With the computer navigated lateral femoral epicondylar osteotomy is fulfilled precise, absolutely controlled, quantitative lengthening of lateral structures and restoration of optimum soft tissue balance and alignment[43].
Medial soft tissue: As described by Krackow et al[44] in grade II valgus deformities the MCL may not be completely functional and a residual medial laxity is poorly tolerated if VD still exists post-operatively. In these conditions the authors suggested tightening of the medial structures, particularly if the PCL is retained. The advancement of the MCL from the epicondyle or a division and imbrication in order to tighten it can be performed along with the use of constrained condylar implant prosthesis[6] (Figure 5).
In the last three decades, a number of different surgical techniques have been described for TKA, in severe valgus deformed knees[1-6,9-11,17,31-33]. As already mentioned, with the aim of correcting the mechanical axis in valgus knees and achieving soft tissue stability, proper bony alignment and ligament balancing are critical. The distal femoral cut at 3° only, instead of 5° to 7° that applies in varus knees, protects against under-correction. In order the mechanical axis after operation not to shift back into valgus, a slightly more varus result has been proposed during TKA for VD[30]. Miyasaka et al[30] in their 10 to 20-year follow-up study presented 75% successful bony alignment by having a postoperative valgus alignment 2° to 7°.
Above and beyond, on the subject of ligament balancing in valgus knee there is no consensus on the subject of the correct sequence in which the lateral elements should be released. Starting with Insall et al[45], in 1979, who described soft-tissue balancing by transverse division of the ITB above the joint line, and hereafter the lateral aspect of the capsule, the LCL and the POP were detached from the lateral femoral condyle[9,45]. Insall referred 93% of excellent or good results with almost 3% posterior subluxation and 3.6% reoperation rate in 5 years[45] and 6.7% in 12 years[46].
Later on, Keblish[11], Buechel[25] and Fiddian et al[28] suggested a lateral capsular approach with or without TTO. More specifically, Keblish[11] presented lateral approach in valgus knees as a “direct, anatomical, more physiologic surgical technique that maintained soft-tissue integrity”. By performing “lateral release” as part of the main approach in these 79 cases, Keblish[11] presented on the one hand improvement on the limb alignment, and patellofemoral stability and tracking; whereas on the other hand preserved the medial blood supply. Clinical experience also showed a more aesthetic approach and with results objectively superior. Due to that the lateral approach was recommended as the “approach of choice” for fixed VD in TKA. Scores was good to excellent in 94.3% of cases; whereas knee stability was enhanced with the use of non-constrained prostheses in that difficult group of patients[11].
Buechel[25] suggested that lateral release with TTO allows the surgeon firstly to regain neutral alignment in valgus deformities of up to 90˚ and secondly to correct the fixed external tibial rotation deformity. Furthermore, Fiddian et al[28] used a lateral capsular approach with repositioning of vastus lateralis at closure. It was presented good to excellent results in all the 25 cases on the knee ROM and the VD restoration; apart from 2 cases which developed 10˚ and 15˚ of fixed flexion deformity. Repositioning of vastus lateralis offered also consistent restoration of the normal patellofemoral tracking[28].
Meanwhile, Whiteside recommended sequential releases of the ITB, POP, LCL and lateral head of gastrocnemius[26]. It was also performed TTO and transfer when the Q angle was > 20°. Whiteside presented mean valgus angle after surgery at 7°; but without alignment or varus-valgus stability deterioration during the 6-year follow-up period. Nevertheless, the deformed knees over 25° had a tendency to increase posterior laxity. Lastly, patellar subluxation and dislocation occurred in less than 1% of the cases[26].
On the other hand, Krackow et al[10,39,44] and Healy et al[47] mentioned medial soft-tissue advancement or reconstruction in combination with lateral release. To be more specific Krackow et al[39] studied in cadavers the flexion-extension joint gap change after lateral structure release for VD correction in TKA, and concluded that in severe VD, it should be considered firstly the LCL release and afterwards gradually release of the POP and ITB to be performed. In the 99 knees reported Grade I VD knees (according to Ranawat scale) were treated with lateral soft-tissue release, and Grade II patients were treated with medial capsular ligament tightening (ligament reconstruction procedures on the medial side). The results were 72% excellent, 17.5% good, 8.25% fair, and 2.25% poor. Ligament stability was satisfactorily established by lateral release in Grade I and with the combined medial plication in the Grade II patients[44]. Healy et al[47] presented on the one hand the lateral ITB release at the level of the tibial osteotomy, and on the other hand proximal MCL advancement with bone plug recession in Grade II VD knees. The researchers concluded that all the knees were stable with a functional ROM at the time of the last follow-up in 4 to 9 years.
Apart from Krackow cadaveric study, extremely interesting results published in 2001 by Peters et al[48] who studied the flexion-extension gap symmetry in the valgus knee TKA during sequenced release of lateral structures. They concluded that the ITB complete release at the joint line had a more profound effect on the extension than the flexion gap. On the contrary, complete release from the femur of the LCL/POP affected more profoundly the flexion vs the extension gap; both of these release steps produced gap increases that were significant (7-12 mm). Consequently, selective release even of the ITB (fractional lengthening), PLC, and POP tendons alone produced smaller magnitudes of correction, and then more symmetrically affected flexion-extension gaps[48].
Besides, Politi et al[49] presented in 2004, good-to-excellent results by achieving soft tissue balancing in TKAs with VD > 15°, by using a lateral cruciform retinacular (LCR) release, while the LCL and POP are not released. In 3 only cases out of 35, extension gap balancing could not be achieved by using only the LCR release; and so the LCL and POP were partially released to balance the knee. No further constraint prosthesis was necessary after these releases, whereas the stability of these knees remained stable at the latest mean 3.4-year follow-up[49].
Stern et al[31] achieved good-to-excellent results in 91% of his patients in knees with VD > 10°, by accomplishing ligamentous balancing in TKA with sequential releases from the lateral side of the femur and without MCL reconstruction. The postoperative axis alignment was 5° to 9° valgus. Likewise, Laurencin et al[50] succeeded excellent results and achieved postoperative anatomic alignment between 0° and 10° valgus in 96% of TKAs with 25° VD, by releasing lateral retinacular with sequential lateral release.
Chalidis et al[51] in 2014 presented the outcome of 57 valgus knees Grade II according to the Ranawat classification that underwent a primary TKA via lateral parapatellar approach with a global step-cut “coffin” type TTO over a 10-year period. Post-operatively, the knee extension, flexion, Knee Society Pain and Function Scores and WOMAC Osteoarthritis Index were significantly improved. In all cases the patellar tracking observed to be congruent. The researchers concluded that “lateral parapatellar approach along with TTO is an effective technique for addressing non-correctable valgus knee deformity during TKA”[51].
Another interesting way to balance the VD knee is the one proposed in 2002 by Brilhault et al[41]. The surgeons’ treated 13 patients with fixed knee VD by implanting a semi-constrained TKA along with advancement of the LCL by performing a lateral femoral condylar sliding osteotomy. At follow-up of mean 4.6 years, it was improvement of the mean Knee Society score from 32 to 88 and of the functional score from 45 to 73. The mean anatomical axis was corrected from 191 degrees to 180 degrees. There were no postoperative complications as tibiofemoral or patellar instability or distal transposition of the lateral femoral condyle osteotomy[41].
Likewise, Hadjicostas et al[52] presented excellent mid-term results of 15 TKAs with VD over 20˚ by using an osteotomy of the lateral femoral condyle and computer navigation. Before the final fixation of the lateral femoral condyle, the correct mediolateral balancing of the extension gap was confirmed by the navigation system. All the knees were corrected between 0° to 2° valgus. There were also post-operative statistical significant improvement of the knee flexion to a mean of 105° (90° to 130°) and to the mean Knee Society score from 37 (30 to 44) to 90 points (86 to 94)[53].
Consequently, the “inside-out” or the “outside-in” technique has been proposed by different many surgeons, as Keblish[11], Murray et al[8], Stern et al[31], Buechel[25] and with similar results. Likewise, the “pie crust” technique by Clarke et al35] and Bruzzone et al[37] through the taut PLC or ITB with the knee fully extended has also be proposed as an alternative, having the orthopaedic surgeon always the same expectation, the knee balance[53]. If the lateral release does not sufficiently stabilize flexion and extension gaps, then the medial side of the joint should be addressed, in an effort to limit the degree of lateral soft-tissue release[4,6]. Several techniques have been also described for successfully and safely “tightening” the incompetent MCL[10,39,47] (Table 1).
| Ref. | No knees | Valgus deformity | Technique | Implant Selection | Results | Follow-up |
| Ranawat et al[1] | 85 | > 10˚ | Inside-out soft-tissue release of PLC with pie-crusting of the ITB Resection of proximal part of tibia and distal part of femur to provide a balanced, rectangular space | PS | Knee Society Score improved from 30 to 93 points; mean functional score improved from 34 to 81 points; mean ROM 110° 3 patients underwent revision No cases of delayed instability | 10 yr |
| Apostolopoulos et al[3] | 33 | > 10˚ | Lateral parapatellar arthrotomy, in combination with TTO ITB is elevated from Gerdy’s tubercle Pie-crust technique in LCL and PLC if needed | CR, PS, VVC or CCK (> 20 ˚) | Mean IKS score improved from 44 points preoperatively, to 91 points postoperatively, at the last follow-up In terms of alignment parameter, only 2 knees had a residual valgus deviation greater than 7° | 11.5 yr |
| Karachalios et al[5] | 51 | > 20˚ | Medial or lateral parapatellar arthrotomy; balancing non referred | CR or PS | Bristol knee score 84.3% excellent to good results; 15.7% fair to poor Some deformity persisted in 14/51 patients. These patients had a significantly poorer mean clinical outcome Lateral dislocation or subluxation of the patella was found in 4 knees, with VD > 30˚ | 5.5 yr |
| Elkus et al[9] | 85 | > 10˚ | Inside-out soft-tissue release of PCL with pie-crusting of the ITB and resection of the proximal part of the tibia and distal part of the femur to provide a balanced, rectangular space | PS | The mean modified Knee Society clinical score improved from 30 points preoperatively to 93 points postoperatively and the mean functional score improved from 34 to 81 points. The mean post- ROM was 110˚ No cases of delayed instability | 5 yr |
| Krackow et al[10] | 99 | Type I and II Ranawat | Type I: Lateral soft tissue release Type II: Medial capsular ligament tightening | CR | Knee Society post-operative knee score was 87.6 (± 10.6) and mean post-operative functional score was 52.3 | 2 yr |
| Keblish[11] | 79 | Type 2 and 3 Ranawat | Lateral approach ITB, PLC release | Non-constrained | Scores have been good/excellent in 94.3% of cases | > 2 yr |
| Whiteside[26] | 135 | 91: 8˚-15˚ 25: 16˚-25˚ 19: > 25˚ | Lateral approach < 15˚: LCL release < 25˚: + ITB > 25 ˚: + POP + Lat. Head gastrocnemius | CR | Neither alignment nor varus-valgus stability deteriorated during the six-year follow-up period, but the knees with greater than 25 degrees deformity had a tendency to increase posterior laxity Patellar subluxation and dislocation occurred in less than 1% of the cases | 6 yr |
| Burki et al[27] | 61 | > 10˚ | Lateral approach with TTO LCL release | CR | Good or excellent in 45 (88%) patients, fair in four (8%), and poor in two (4%) No postoperative tibial fractures, no delayed unions, and no nonunions at the site of the osteotomy were seen | 1 yr |
| Stern et al[31] | 134 | > 10˚ | Medial approach and lateral release | 118 PS, 8 VVC, 4 KSS, 4 CR | 95 knees (71%) rated as excellent, 27 knees (20%) as good, eight knees (6%) as fair, and four knees (3%) as poor Postoperatively, 76% of the knees had a tibiofemoral alignment between 5 degrees and 9 degrees valgus with an overall average of 7 degrees valgus | 2-10 yr (mean 4.5 yr) |
| Miyasaka et al[30] | 108 | > 10˚ | Medial approach Releasing the lateral retinaculum and ITB, followed when necessary by detaching the PCL and POP tendon from the femur | PS | Mean Knee Society knee score was 88.7 and the mean functional score was 69.2. Postoperative knee alignment averaged 4.5 degrees with 75% of the knees corrected to between 2 degrees and 7 degrees valgus. Postoperative flexion averaged 101 degrees | 10-20 yr |
| Sekiya et al[32] | 47 | 6°-24° | All cases required ITB release at Gerdy's tubercle, 83% ITB at joint level, 21% LCL, 17% POP in medial approach group, and 88% ITB at Gerdy's tubercle, 46% ITB at joint level, 13% LCL, 4% POP in lateral approach group | PS | Pre/postoperative alignment, surgical time, lateral laxity, and preoperative ROM had no significant in two groups; however, postoperative flexion was superior in lateral approach group 123.8°, 109° in medial approach group | 43 mo |
| Chalidis et al[51] | 57 | Type II Ranawat | Lateral approach and TTO | PS | Significant improvement in knee extension (P = 0.002), flexion (P = 0.006), Knee Society Pain and Function Scores (P < 0.001) and WOMAC Osteoarthritis Index (P < 0.001) The tibiofemoral angle changed from a preoperative median value of 11° (10 to 17) to a postoperative value of 3.75° (0 to 9) | 20-98 mo |
| Hadjicostas et al[52] | 15 | 17°-24° | Osteotomy of the lateral femoral condyle and computer navigation | CR | All the knees were corrected to a mean of 0.5° of valgus (0 to 2) Flexion of the knee had been limited to a mean of 85° (75 to 110) pre-operatively and improved to a mean of 105° (90 to 130) after operation The mean Knee Society score improved from 37 (30 to 44) to 90 points (86 to 94) | 24-60 mo |
The medial parapatellar arthrotomy although recommended as a standard procedure in a varus knee, does not represent the optimal approach in a severe and technically demanding VD knee[4]. More specifically, release of lateral patellar retinaculae is necessitated in most cases, in order to prevent patellar instability. The latter in combination with medial capsulotomy results in significant impairment of the extensor (quadriceps-patellar tendon) mechanism’s blood supply[54]. However if the knee joint is approached via a lateral parapatellar arthrotomy, release of the lateral retinaculae is integrated in the approach. Patella vascularity is also preserved, as the medial side stays undisturbed[4,10,54]. Laurencin et al[50] reported 12% rate of the patella avascular necrosis in TKA by performing medial approach with an extensive lateral release. Miyasaka et al[30] reported only one case out of 108, in which a patella fracture occurred 3 years after surgery that was thought to be secondary due to avascular necrosis. In Apostolopoulos et al[3] and Nikolopoulos et al[4] series, no patella fracture or avascular necrosis was observed.
Moreover, in the medial approach, the lateral displacement of the extensor mechanism increases the external tibial rotation, pushing the contracted PLC away from the operative field[11]. In the lateral capsulotomy the surgeon succeeds better viewing of the contracted lateral structures, as the extensor mechanism is displaced medially, and the tibia rotates internally. As a consequence the hazard of unnecessary steps that may create instability is limited[4,11].
Moreover, in cases that patella’s eversion may be compromised by scar tissue - for instance previous tibial osteotomy - the patellar ligament may be particularly prone to avulsion by forceful intraoperative retraction. Therefore, in order to protect the knee extensor mechanism, additional surgical steps are needed either proximally (V-Y quadricepsplasty or “quadriceps snip”)[55,56], or distally to the patella (with TTO)[4,6,27,33,57-60].
Analyzing the literature on the subject of TTO, it is considered as a highly advantageous and safe procedure in achieving gentle eversion of the patella without avulsion[1,4,6,27,33,57-60]. Besides, it prevents tibia internal rotation during patellar eversion, which may simplify the correct positioning of the tibial component in severe valgus knees[4,10,60]. It is true that when a TTO is added to the lateral approach in primary TKA in severe deformed valgus knees, the eversion of the patella is easily performed, offering excellent view[4].
Additionally, with a medial capsulotomy, patella tracking is less than optimum and postoperative patellar problems are more common[10,11,26]. Conversely, with a lateral approach patellar tracking is assured with the self-centering movement of the quadriceps-patellar tendon mechanism[1,11,26]. In cases where lateral capsulotomy is combined with TTO, alignment of the extensor mechanism can be improved or adjusted when required, as osteotomy allows transfer of the patellar tendon insertion medially, eliminating the postoperative hazard for patellar maltracking[4,11]. In our series, no patellar instability was observed post-operatively in the Group of lateral parapatellar arthrotomy combined with TTO, as we had the chance to release the soft tissues easily and to transfer the tuberosity medially in two cases; succeeding the optimal quadriceps-patella tendon balance[4].
Burki et al[27] applied TTO as a part of their lateral approach in revision valgus TKAs, observing good results in 88%. No complications from the osteotomy side were reported; apart from one case complicated with anterior tibial compartment syndrome. Apostolopoulos et al[3] also presented one case in their series. Burki et al[27] believed that the TTO may traumatize the anterior tibial compartment; that’s why it was recommended release of the anterior tibial fascia with several longitudinal incisions. The length of the osteotomized tubercle in Burki approach was 7 cm, while Apostolopoulos et al[3] and Nikolopoulos et al[4] shorten it to 5 cm, in order to avoid tibial fractures. Piedade had TTO fractures and tibial plateau fissures in 8.7%[58]. Consequently, consideration needs to be given to the size of the osteotomized bone fragment and the quality of the internal fixation so as to be stable[4].
The results of TKA in valgus knees with conventional medial parapatellar capsulotomy have been inferior to those of varus knees with significant deformity[5]. Karachalios et al[5] mentioned the residual VD in these total knee arthroplasties did not result in early component failure, but was associated with a worse clinical outcome, due to patellofemoral malalignment. The literature refers full restoration of the anatomical axis in 70%-78% of valgus knees[2,5,6,9]. Incomplete axis restoration has been linked with impaired clinical outcome[4,5]. Conversely, authors using lateral parapatellar capsulotomy have reported better results in terms of anatomical axis correction and also in terms of clinical performance[11,25]. Besides, Krackow et al[10] by using a PCL-sparing prosthesis presented in 90% of cases good results; as the PCL is not usually contracted in VD knees. However, in severe VD the mechanical axis correction is performed with PCL release. A PCL release or a PCL-substituting prosthesis should be selected in severe valgus deformed knees[25,61].
Lastly, it is important to be mentioned the results of the open debate about which approach leads to better outcome. The recent studies of comparison of a standard medial parapatellar approach in contrast to lateral parapatellar with TTO showed the following. Nikolopoulos et al[4] presented no statistically significant differences in terms of clinical results, on the groups of lateral approach with TTO and in the second one of a standard medial approach (Figure 6). Nevertheless in the lateral approach group a valgus deviation occurred in 9% of the patients, compared to 32% in the medial approach one[4]. A similar study has been published by Hirschmann et al[33] concluding that the lateral approach combined with TTO leads to comparable functional results and reduced pain at 2 years follow-up. The question that easily arises for the researchers however remained if these results can outweigh the higher risk of early complications and revisions. Moreover, by studying the results in two randomized groups of valgus TKAs, Sekiya et al[32] found no significant differences in range of movement (ROM), but better post-operative flexion in the group of lateral approach without TTO vs the group of medial parapatellar approach.
Hay et al[62] randomly divided 32 patients in two groups, the one in which lateral subvastus approach combined with a TTO was performed and the other with classic medial approach. Between the two groups no significant differences were found in the parameters of clinical outcome (ROM, VAS score, Western Ontario McMasters University Osteoarthritis index, and KSS) at 2 years follow-up. Better patellar tracking was observed in the group of lateral subvastus approach combined with TTO. Nevertheless the researchers did not support its routine use, because of the complications related with TTO and the longer surgical time (10-15 min). It is not indicated in patients in whom problems with patellar tracking is anticipated[62].
Favorito et al[6] presented in his review article the several complications that have been reported more frequently in this subset of patients. The most commonly reported complications in patients with VD who undergo TKA are tibiofemoral instability (2% to 70%), recurrent valgus deformity (4% to 38%), postoperative motion deficits which requires manipulation under anesthesia (1% to 20%), wound problems (superficial or deep infection) (4% to 13%), patellar stress fracture or osteonecrosis (1% to 12%), patellar tracking problems (2% to 10%), and peroneal nerve palsy (1% to 4%)[1,2,4,8,10,13,37]. In cases with arthrofibrosis and limited flexion < 90° an arthroscopic arthrolysis can be successfully performed[13,33].
Other complications often referred in the English literature are proximal migration of the osteotomized fragment in TTO. In our cases a 5 mm proximal migration was occurred due to breakage of one of the two screws being used to stabilize the osteotomized fragment in one patient[3]. In other cases there is breakage of the wire loops or local infection of the material even early postoperatively, or after the osteotomy fusion[2,27,32,51].
Deep venous thrombosis has also been detected, or superficial or deep infections. Often hematomas, bruises and skin blisters are seen, as in Apostolopoulos et al[3] and Nikolopoulos et al[4] patients that was treated conservatively. Other researchers referred skin necrosis. Chalidis et al[51] published a case of TKA in a patient suffering from rheumatoid arthritis that had as a complication poor wound healing and breakdown, and which was addressed with a gastrocnemius flap. Non-union of the tibial osteotomy was also displayed with migration of the bone fragment.
Very often, especially in cases of TTO, there are operative or post-operative proximal tibial stress fractures. These fractures can be treated surgically or conservative including application of functional knee brace and toe-touch weight bearing of the affected leg till the fracture heals[27,31-33,51].
Peroneal nerve palsy has been cited as an important complication after TKA for VD. The elongation of the lateral side stretches the nerve and places it at risk for indirect injury, via traction or induced ischemia[4,6,22]. Other indirect mechanisms of injury may include compression or crushing from tight dressings[63]. When using the “pie crust” technique as part of the lateral release, there is greater deal of concern regarding peroneal nerve safety[27,35,37]. Idusuyi et al[64] reported 32 postoperative peroneal nerve palsies in more than ten thousand consecutive TKAs. Of the 32 palsies, 10 knees had 12 degrees of preoperative VD or more. This problem presumably is caused by lengthening the lateral aspect of the knee during lateral stabilizer release and subsequent traction to the peroneal nerve. It is generally recommended that patients be evaluated carefully for symptoms postoperatively. If peroneal nerve palsy type symptoms are discovered, the knee should be flexed to relax the tension that is effectively being placed on the nerve. There are no objective guidelines or data to support the efficacy of any immediate surgical intervention[64].
TKA is the gold standard procedure with excellent results for the treatment of advanced knee arthritis. Nevertheless, the long-term results in valgus deformed knee were relatively inferior to those of varus deformation. One of the main reasons of poor prognosis may be the difficulty to acquire good soft-tissue balance during the surgery. That’s the reason the valgus knee presents a challenge to the joint replacement surgeon. By taking into account the pre-existing anatomic deformities and by using the AP axis for femoral component placement may help prevent postoperative patellofemoral maltracking and instability. This article is an up-to-date review of the valgus knee philosophy, the approaches and surgical techniques proposed so as to fulfill the lower limb mechanical axis correction; analyzing in detail the pros and cons of each proposed technique. The surgeon in valgus knee should more confidently achieve soft tissue balancing, resulting in better load distribution and enhancing component stability and longevity.
P- Reviewer: Canavese F, Colak T, Kovar MF S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005;87 Suppl 1:271-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 85] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 2. | Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop. 2014;38:273-283. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Apostolopoulos AP, Nikolopoulos DD, Polyzois I, Nakos A, Liarokapis S, Stefanakis G, Michos IV. Total knee arthroplasty in severe valgus deformity: interest of combining a lateral approach with a tibial tubercle osteotomy. Orthop Traumatol Surg Res. 2010;96:777-784. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Nikolopoulos DD, Polyzois I, Apostolopoulos AP, Rossas C, Moutsios-Rentzos A, Michos IV. Total knee arthroplasty in severe valgus knee deformity: comparison of a standard medial parapatellar approach combined with tibial tubercle osteotomy. Knee Surg Sports Traumatol Arthrosc. 2011;19:1834-1842. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Karachalios T, Sarangi PP, Newman JH. Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg Br. 1994;76:938-942. [PubMed] [Cited in This Article: ] |
| 6. | Favorito PJ, Mihalko WM, Krackow KA. Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg. 2002;10:16-24. [PubMed] [Cited in This Article: ] |
| 7. | White GR, Mencio GA. Genu Valgum in Children: Diagnostic and Therapeutic Alternatives. J Am Acad Orthop Surg. 1995;3:275-283. [PubMed] [Cited in This Article: ] |
| 8. | Murray PB, Rand JA. Symptomatic Valgus Knee: The Surgical Options. J Am Acad Orthop Surg. 1993;1:1-9. [PubMed] [Cited in This Article: ] |
| 9. | Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J Bone Joint Surg Am. 2004;86-A:2671-2676. [PubMed] [Cited in This Article: ] |
| 10. | Krackow KA, Jones MM, Teeny SM, Hungerford DS. Primary total knee arthroplasty in patients with fixed valgus deformity. Clin Orthop Relat Res. 1991;9-18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Keblish PA. The lateral approach to the valgus knee. Surgical technique and analysis of 53 cases with over two-year follow-up evaluation. Clin Orthop Relat Res. 1991;52-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 97] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Satish BR, Ganesan JC, Chandran P, Basanagoudar PL, Balachandar D. Efficacy and mid term results of lateral parapatellar approach without tibial tubercle osteotomy for primary total knee arthroplasty in fixed valgus knees. J Arthroplasty. 2013;28:1751-1756. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Rajgopal A, Dahiya V, Vasdev A, Kochhar H, Tyagi V. Long-term results of total knee arthroplasty for valgus knees: soft-tissue release technique and implant selection. J Orthop Surg (Hong Kong). 2011;19:60-63. [PubMed] [Cited in This Article: ] |
| 14. | Radulescu R, Badila A, Japie I, Ciobanu T, Manolescu R. Primary total knee arthroplasty in severe valgus knee. J Med Life. 2013;6:395-398. [PubMed] [Cited in This Article: ] |
| 15. | Girard J, Amzallag M, Pasquier G, Mulliez A, Brosset T, Gougeon F, Duhamel A, Migaud H. Total knee arthroplasty in valgus knees: predictive preoperative parameters influencing a constrained design selection. Orthop Traumatol Surg Res. 2009;95:260-266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Ang CL, Fook S, Chia SL, Chin PL, Lo NN, Yeo SJ. Unconstrained arthroplasty in type II valgus knees: posterior stabilized or cruciate retaining? Knee Surg Sports Traumatol Arthrosc. 2014;22:666-673. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Lombardi AV, Dodds KL, Berend KR, Mallory TH, Adams JB. An algorithmic approach to total knee arthroplasty in the valgus knee. J Bone Joint Surg Am. 2004;86-A Suppl 2:62-71. [PubMed] [Cited in This Article: ] |
| 18. | Swanson KE, Stocks GW, Warren PD, Hazel MR, Janssen HF. Does axial limb rotation affect the alignment measurements in deformed limbs? Clin Orthop Relat Res. 2000;246-252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 99] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Robbins GM, Masri BA, Garbuz DS, Duncan CP. Preoperative planning to prevent instability in total knee arthroplasty. Orthop Clin North Am. 2001;32:611-626, viii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Mihalko WM, Miller C, Krackow KA. Total knee arthroplasty ligament balancing and gap kinematics with posterior cruciate ligament retention and sacrifice. Am J Orthop (Belle Mead NJ). 2000;29:610-616. [PubMed] [Cited in This Article: ] |
| 21. | Matsuda Y, Ishii Y, Noguchi H, Ishii R. Varus-valgus balance and range of movement after total knee arthroplasty. J Bone Joint Surg Br. 2005;87:804-808. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 86] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Mihalko WM, Krackow KA. Anatomic and biomechanical aspects of pie crusting posterolateral structures for valgus deformity correction in total knee arthroplasty: a cadaveric study. J Arthroplasty. 2000;15:347-353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | McAuley JP, Collier MB, Hamilton WG, Tabaraee E, Engh GA. Posterior cruciate-retaining total knee arthroplasty for valgus osteoarthritis. Clin Orthop Relat Res. 2008;466:2644-2649. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Williot A, Rosset P, Favard L, Brilhault J, Burdin P. Total knee arthroplasty in valgus knee. Orthop Traumatol Surg Res. 2010;May 4; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Buechel FF. A sequential three-step lateral release for correcting fixed valgus knee deformities during total knee arthroplasty. Clin Orthop Relat Res. 1990;170-175. [PubMed] [Cited in This Article: ] |
| 26. | Whiteside LA. Correction of ligament and bone defects in total arthroplasty of the severely valgus knee. Clin Orthop Relat Res. 1993;234-245. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 49] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Burki H, von Knoch M, Heiss C, Drobny T, Munzinger U. Lateral approach with osteotomy of the tibial tubercle in primary total knee arthroplasty. Clin Orthop Relat Res. 1999;156-161. [PubMed] [Cited in This Article: ] |
| 28. | Fiddian NJ, Blakeway C, Kumar A. Replacement arthroplasty of the valgus knee. A modified lateral capsular approach with repositioning of vastus lateralis. J Bone Joint Surg Br. 1998;80:859-861. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 47] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Arima J, Whiteside LA, McCarthy DS, White SE. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am. 1995;77:1331-1334. [PubMed] [Cited in This Article: ] |
| 30. | Miyasaka KC, Ranawat CS, Mullaji A. 10- to 20-year followup of total knee arthroplasty for valgus deformities. Clin Orthop Relat Res. 1997;29-37. [PubMed] [Cited in This Article: ] |
| 31. | Stern SH, Moeckel BH, Insall JN. Total knee arthroplasty in valgus knees. Clin Orthop Relat Res. 1991;5-8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 49] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Sekiya H, Takatoku K, Takada H, Sugimoto N, Hoshino Y. Lateral approach is advantageous in total knee arthroplasty for valgus deformed knee. Eur J Orthop Surg Traumatol. 2014;24:111-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Hirschmann MT, Hoffmann M, Krause R, Jenabzadeh RA, Arnold MP, Friederich NF. Anterolateral approach with tibial tubercle osteotomy versus standard medial approach for primary total knee arthroplasty: does it matter? BMC Musculoskelet Disord. 2010;11:167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB. Soft tissue release in total knee arthroplasty. Cadaver study using knees without deformities. Clin Orthop Relat Res. 1999;264-273. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 111] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 35. | Clarke HD, Fuchs R, Scuderi GR, Scott WN, Insall JN. Clinical results in valgus total knee arthroplasty with the “pie crust” technique of lateral soft tissue releases. J Arthroplasty. 2005;20:1010-1014. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 36. | Aglietti P, Lup D, Cuomo P, Baldini A, De Luca L. Total knee arthroplasty using a pie-crusting technique for valgus deformity. Clin Orthop Relat Res. 2007;464:73-77. [PubMed] [Cited in This Article: ] |
| 37. | Bruzzone M, Ranawat A, Castoldi F, Dettoni F, Rossi P, Rossi R. The risk of direct peroneal nerve injury using the Ranawat “inside-out” lateral release technique in valgus total knee arthroplasty. J Arthroplasty. 2010;25:161-165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Whiteside LA. Selective ligament release in total knee arthroplasty of the knee in valgus. Clin Orthop Relat Res. 1999;130-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 98] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 39. | Krackow KA, Mihalko WM. Flexion-extension joint gap changes after lateral structure release for valgus deformity correction in total knee arthroplasty: a cadaveric study. J Arthroplasty. 1999;14:994-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 81] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 40. | Boyer P, Boublil D, Magrino B, Massin P, Huten D. Total knee replacement in the fixed valgus deformity using a lateral approach: role of the automatic iliotibial band release for a successful balancing. Int Orthop. 2009;33:1577-1583. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Brilhault J, Lautman S, Favard L, Burdin P. Lateral femoral sliding osteotomy lateral release in total knee arthroplasty for a fixed valgus deformity. J Bone Joint Surg Br. 2002;84:1131-1137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 42. | Bremer D, Orth BC, Fitzek JG, Knutsen A. [Briard’s sagittal sliding osteotomy of the lateral condyle in total knee arthoplasty of the severe valgus knee]. Oper Orthop Traumatol. 2012;24:95-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Mullaji AB, Shetty GM. Lateral epicondylar osteotomy using computer navigation in total knee arthroplasty for rigid valgus deformities. J Arthroplasty. 2010;25:166-169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 44. | Krackow KA, Holtgrewe JL. Experience with a new technique for managing severely overcorrected valgus high tibial osteotomy at total knee arthroplasty. Clin Orthop Relat Res. 1990;213-224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 45. | Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61:173-180. [PubMed] [Cited in This Article: ] |
| 46. | Vince KG, Insall JN, Kelly MA. The total condylar prosthesis. 10- to 12-year results of a cemented knee replacement. J Bone Joint Surg Br. 1989;71:793-797. [PubMed] [Cited in This Article: ] |
| 47. | Healy WL, Iorio R, Lemos DW. Medial reconstruction during total knee arthroplasty for severe valgus deformity. Clin Orthop Relat Res. 1998;161-169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 86] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 48. | Peters CL, Mohr RA, Bachus KN. Primary total knee arthroplasty in the valgus knee: creating a balanced soft tissue envelope. J Arthroplasty. 2001;16:721-729. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 49. | Politi J, Scott R. Balancing severe valgus deformity in total knee arthroplasty using a lateral cruciform retinacular release. J Arthroplasty. 2004;19:553-557. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 50. | Laurencin CT, Scott RD, Volatile TB, Gebhardt EM. Total knee replacement in severe valgus deformity. Am J Knee Surg. 1992;5:135-139. [Cited in This Article: ] |
| 51. | Chalidis BE, Ye K, Sachinis NP, Hawdon G, McMahon S. Lateral parapatellar approach with tibial tubercle osteotomy for the treatment of non-correctable valgus knee osteoarthritis: a retrospective clinical study. Knee. 2014;21:204-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 52. | Hadjicostas PT, Soucacos PN, Thielemann FW. Computer-assisted osteotomy of the lateral femoral condyle with non-constrained total knee replacement in severe valgus knees. J Bone Joint Surg Br. 2008;90:1441-1445. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 53. | McNabb DC, Kim RH, Springer BD. Instability after total knee arthroplasty. J Knee Surg. 2015;28:97-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 54. | Wetzner SM, Bezreh JS, Scott RD, Bierbaum BE, Newberg AH. Bone scanning in the assessment of patellar viability following knee replacement. Clin Orthop Relat Res. 1985;215-219. [PubMed] [Cited in This Article: ] |
| 55. | Coonse K, Adams JD. A new operative approach to the knee joint. Surg Gynecol Obstet. 1943;77:344–347. [Cited in This Article: ] |
| 56. | Garvin KL, Scuderi G, Insall JN. Evolution of the quadriceps snip. Clin Orthop Relat Res. 1995;131-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 57. | Dolin MG. Osteotomy of the tibial tubercle in total knee replacement. A technical note. J Bone Joint Surg Am. 1983;65:704-706. [PubMed] [Cited in This Article: ] |
| 58. | Whiteside LA, Ohl MD. Tibial tubercle osteotomy for exposure of the difficult total knee arthroplasty. Clin Orthop Relat Res. 1990;6-9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 91] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 59. | Wolff AM, Hungerford DS, Krackow KA, Jacobs MA. Osteotomy of the tibial tubercle during total knee replacement. A report of twenty-six cases. J Bone Joint Surg Am. 1989;71:848-852. [PubMed] [Cited in This Article: ] |
| 60. | Piedade SR, Pinaroli A, Servien E, Neyret P. Tibial tubercle osteotomy in primary total knee arthroplasty: a safe procedure or not? Knee. 2008;15:439-446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 61. | Insall JN, Easley ME. Surgical techniques and instrumentation in total knee arthroplasty. Surgery of the Knee. 3rd ed. New York NY: Churchill Livingstone 2001; 1717-1738. [Cited in This Article: ] |
| 62. | Hay GC, Kampshoff J, Kuster MS. Lateral subvastus approach with osteotomy of the tibial tubercle for total knee replacement: a two-year prospective, randomised, blinded controlled trial. J Bone Joint Surg Br. 2010;92:862-866. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 63. | Rose HA, Hood RW, Otis JC, Ranawat CS, Insall JN. Peroneal-nerve palsy following total knee arthroplasty. A review of The Hospital for Special Surgery experience. J Bone Joint Surg Am. 1982;64:347-351. [PubMed] [Cited in This Article: ] |
| 64. | Idusuyi OB, Morrey BF. Peroneal nerve palsy after total knee arthroplasty. Assessment of predisposing and prognostic factors. J Bone Joint Surg Am. 1996;78:177-184. [PubMed] [Cited in This Article: ] |