Opinion statement
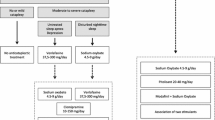
In the absence of sleep deprivation (either because of behavioral or medical causes) or pharmacologically induced sleepiness, hypersomnia is a manifestation of one of the central disorders of hypersomnolence, such as narcolepsy types 1 and 2, idiopathic hypersomnia, and recurrent hypersomnias such as Kleine-Levin syndrome. Narcolepsy and most primary hypersomnias are chronic conditions, thus, before committing an individual to chronic, possibly, life-long treatments, an accurate diagnosis is important. The key to effective management of hypersomnia, thus, lies in a thorough history, detailed physical examination, and appropriate diagnostic tests. Secondary causes of hypersomnia are expected to resolve once these disorders are treated. The treatment of central hypersomnias, on the other hand, is guided by a level of diagnostic certainty as to the etiology of the hypersomnia. Narcolepsy, for example, has well defined pathophysiologic and diagnostic criteria, including low levels of hypocretin in cerebrospinal fluid (CSF) and specific findings on a polysomnography/multiple sleep latency test (PSG/MSLT). For these patients, life-long therapy is the norm and involves initiating treatment usually with modafinil, armodafinil, or sodium oxybate, with methylphenidate, amphetamine-like stimulants, atomoxetine, or antidepressants used as second-line therapy. Pharmacologic therapy is usually done in concert with behavioral modifications such as scheduled napping for the best response. On the other hand, the etiology and pathophysiology of non-hypocretin-related hypersomnias (eg, idiopathic hypersomnia, Kleine-Levine syndrome) are unknown. For these reasons, treatment of these disorders is more challenging and less well defined. A trial of modafinil or armodafinil may be considered as first line therapy along with behavioral modifications. Methylphenidate, amphetamine-based stimulants, and even clarithromycin have also been used. There is no effective cure for hypersomnia, and the current therapy is purely symptomatic. Thus, initial patient education, addressing treatment expectations, as well as continued regular follow-up to monitor treatment response are vital to effective management of hypersomnia. The focus of this article is limited to a discussion of treatment of central disorders of hypersomnolence.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •Of importance •• Of major importance
American Academy of Sleep Medicine. The international classification of sleep disorders: diagnostic & coding manual. 2nd ed. Westchester: American Academy of Sleep Medicine; 2005. p. xviii. 297p. This is authoritative text for diagnosis of sleep disorders worldwide.
Castiglioni P, Lombardi C, Di Rienzo M, Lugaresi E, Montagna P, Cortelli P, et al. What are the causes of excessive daytime sleepiness in patients with sleep-disordered breathing? Eur Respir J. 2008;32(2):526–7.
Gerhardstein R, Day R, Rosenthal L. Narcolepsy and other causes of excessive daytime sleepiness. Respir Care Clin N Am. 1999;5(3):427–46. viii–ix.
Hublin C, Kaprio J, Partinen M, Heikkila K, Koskenvuo M. Daytime sleepiness in an adult, Finnish population. J Intern Med. 1996;239(5):417–23.
Lavie P. Sleep habits and sleep disturbances in industrial workers in Israel: main findings and some characteristics of workers complaining of excessive daytime sleepiness. Sleep. 1981;4(2):147–58.
Ohayon MM, Caulet M, Philip P, Guilleminault C, Priest RG. How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med. 1997;157(22):2645–52.
Mitler MM, Carskadon MA, Czeisler CA, Dement WC, Dinges DF, Graeber RC. Catastrophes, sleep, and public policy: consensus report. Sleep. 1988;11(1):100–9.
Broughton R, Ghanem Q, Hishikawa Y, Sugita Y, Nevsimalova S, Roth B. Life effects of narcolepsy in 180 patients from North America, Asia and Europe compared to matched controls. Can J Neurol Sci J Can Sci Neurol. 1981;8(4):299–304.
Rosekind MR. Underestimating the societal costs of impaired alertness: safety, health and productivity risks. Sleep Med. 2005;6 Suppl 1:S21–5.
Rey de Castro J, Gallo J, Loureiro H. Tiredness and sleepiness in bus drivers and road accidents in Peru: a quantitative study. Pan Am J Public Health. 2004;16(1):11–8.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5.
Rogers AE, Meehan J, Guilleminault C, Grumet FC, Mignot E. HLA DR15 (DR2) and DQB1*0602 typing studies in 188 narcoleptic patients with cataplexy. Neurology. 1997;48(6):1550–6.
Mignot E, Hayduk R, Black J, Grumet FC, Guilleminault C. HLA DQB1*0602 is associated with cataplexy in 509 narcoleptic patients. Sleep. 1997;20(11):1012–20.
Dauvilliers Y, Mayer G, Lecendreux M, Neidhart E, Peraita-Adrados R, Sonka K, et al. Kleine-Levin syndrome: an autoimmune hypothesis based on clinical and genetic analyses. Neurology. 2002;59(11):1739–45.
Krahn LE, Pankratz VS, Oliver L, Boeve BF, Silber MH. Hypocretin (orexin) levels in cerebrospinal fluid of patients with narcolepsy: relationship to cataplexy and HLA DQB1*0602 status. Sleep. 2002;25(7):733–6.
Mignot E, Lammers GJ, Ripley B, Okun M, Nevsimalova S, Overeem S, et al. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Arch Neurol. 2002;59(10):1553–62.
Bourgin P, Zeitzer JM, Mignot E. CSF hypocretin-1 assessment in sleep and neurological disorders. Lancet Neurol. 2008;7(7):649–62.
Morgenthaler TI, Kapur VK, Brown T, Swick TJ, Alessi C, Aurora RN, et al. Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30(12):1705–11.
Rogers AE, Aldrich MS, Lin X. A comparison of three different sleep schedules for reducing daytime sleepiness in narcolepsy. Sleep. 2001;24(4):385–91.
Achermann P, Werth E, Dijk DJ, Borbely AA. Time course of sleep inertia after nighttime and daytime sleep episodes. Arch Ital Biol. 1995;134(1):109–19.
Lopez-Cruz L, Pardo M, Salamone JD, Correa M. Differences between the nonselective adenosine receptor antagonists caffeine and theophylline in motor and mood effects: studies using medium to high doses in animal models. Behav Brain Res. 2014;270C:213–22.
Van Dongen HP, Price NJ, Mullington JM, Szuba MP, Kapoor SC, Dinges DF. Caffeine eliminates psychomotor vigilance deficits from sleep inertia. Sleep. 2001;24(7):813–9.
Reyner LA, Horne JA. Early morning driver sleepiness: effectiveness of 200 mg caffeine. Psychophysiology. 2000;37(2):251–6.
Broughton RJ, Fleming JA, George CF, Hill JD, Kryger MH, Moldofsky H, et al. Randomized, double-blind, placebo-controlled crossover trial of modafinil in the treatment of excessive daytime sleepiness in narcolepsy. Neurology. 1997;49(2):444–51. This is the landmark paper that ushered in modafinil and changed the way we treat daytime sleepiness.
Czeisler CA, Walsh JK, Wesnes KA, Arora S, Roth T. Armodafinil for treatment of excessive sleepiness associated with shift work disorder: a randomized controlled study. Mayo Clin Proc. 2009;84(11):958–72.
Schwartz JR, Khan A, McCall WV, Weintraub J, Tiller J. Tolerability and efficacy of armodafinil in naive patients with excessive sleepiness associated with obstructive sleep apnea, shift work disorder, or narcolepsy: a 12-month, open-label, flexible-dose study with an extension period. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2010;6(5):450–7.
Bastuji H, Jouvet M. Successful treatment of idiopathic hypersomnia and narcolepsy with modafinil. Prog Neuro-Psychopharmacol Biol Psychiatry. 1988;12(5):695–700.
Adler CH, Caviness JN, Hentz JG, Lind M, Tiede J. Randomized trial of modafinil for treating subjective daytime sleepiness in patients with Parkinson's disease. Mov Disord Off J Mov Disord Soc. 2003;18(3):287–93.
Rammohan KW, Lynn DJ. Modafinil for fatigue in MS: a randomized placebo-controlled double-blind study. Neurology. 2005;65(12):1995–7. author reply -7.
Orlikowski D, Chevret S, Quera-Salva MA, Laforet P, Lofaso F, Verschueren A, et al. Modafinil for the treatment of hypersomnia associated with myotonic muscular dystrophy in adults: a multicenter, prospective, randomized, double-blind, placebo-controlled, 4-week trial. Clin Ther. 2009;31(8):1765–73.
Wisor JP, Eriksson KS. Dopaminergic-adrenergic interactions in the wake promoting mechanism of modafinil. Neuroscience. 2005;132(4):1027–34.
Schwartz JR, Feldman NT, Bogan RK, Nelson MT, Hughes RJ. Dosing regimen effects of modafinil for improving daytime wakefulness in patients with narcolepsy. Clin Neuropharmacol. 2003;26(5):252–7.
Rugino T. A review of modafinil film-coated tablets for attention-deficit/hyperactivity disorder in children and adolescents. Neuropsychiatr Dis Treat. 2007;3(3):293–301.
Lecendreux M, Bruni O, Franco P, Gringras P, Konofal E, Nevsimalova S, et al. Clinical experience suggests that modafinil is an effective and safe treatment for paediatric narcolepsy. J Sleep Res. 2012;21(4):481–3. This is an important paper that highlights the fact, that despite the absence of FDA approval, modafinil can be safe in children.
Wise MS, Arand DL, Auger RR, Brooks SN, Watson NF, American Academy of Sleep M. Treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30(12):1712–27.
Ivanenko A, Tauman R, Gozal D. Modafinil in the treatment of excessive daytime sleepiness in children. Sleep Med. 2003;4(6):579–82.
U. S. Xyrem Multicenter Study Group. Sodium oxybate demonstrates long-term efficacy for the treatment of cataplexy in patients with narcolepsy. Sleep Med. 2004;5(2):119–23.
Borgen LA, Cook HN, Hornfeldt CS, Fuller DE. Sodium oxybate (GHB) for treatment of cataplexy. Pharmacotherapy. 2002;22(6):798–9. discussion 9.
US Xyrem Multicenter Study Group. A randomized, double blind, placebo-controlled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsy. Sleep. 2002;25(1):42–9.
Scharf MB, Hauck M, Stover R, McDannold M, Berkowitz D. Effect of gamma-hydroxybutyrate on pain, fatigue, and the alpha sleep anomaly in patients with fibromyalgia. Preliminary report. J Rheumatol. 1998;25(10):1986–90.
Gahlinger PM. Club drugs: MDMA, gamma-hydroxybutyrate (GHB), Rohypnol, and ketamine. Am Fam Physician. 2004;69(11):2619–26.
Huang YS, Guilleminault C. Narcolepsy: action of two gamma-aminobutyric acid type B agonists, baclofen and sodium oxybate. Pediatr Neurol. 2009;41(1):9–16.
Anonymous. The abrupt cessation of therapeutically administered sodium oxybate (GHB) does not cause withdrawal symptoms. J Toxicol Clin Toxicol. 2003;41(2):131–5.
Seiden LS, Sabol KE, Ricaurte GA. Amphetamine: effects on catecholamine systems and behavior. Annu Rev Pharmacol Toxicol. 1993;33:639–77.
Dovedova EL. The mechanism of amphetamine action of the neuromediator system of the brain. Vopr Med Khim. 1994;40(2):7–9.
Mitler MM, Hajdukovic R, Erman M, Koziol JA. Narcolepsy. J Clin Neurophysiol Off Publ Am Electroencephalographic Soc. 1990;7(1):93–118.
Mitler MM, Hajdukovic R, Erman M. Treatment of narcolepsy with methamphetamine. Sleep. 1993;16(4):306–17.
Stiefel G, Besag FM. Cardiovascular effects of methylphenidate, amphetamines and atomoxetine in the treatment of attention-deficit hyperactivity disorder. Drug Saf Int J Med Toxicol Drug Experience. 2010;33(10):821–42.
Guilleminault C. Amphetamines and narcolepsy: use of the Stanford database. Sleep. 1993;16(3):199–201. This is another landmark paper exploring the treatment of narcolepsy in the pre modafinil age.
Yoss RE, Daly D. Treatment of narcolepsy with ritalin. Neurology. 1959;9(3):171–3.
Leonard BE, McCartan D, White J, King DJ. Methylphenidate: a review of its neuropharmacological, neuropsychological and adverse clinical effects. Hum Psychopharmacol. 2004;19(3):151–80.
Schenk JO. The functioning neuronal transporter for dopamine: kinetic mechanisms and effects of amphetamines, cocaine and methylphenidate. Prog Drug Res Fortschr Arzneimittelforschung Prog Rech Pharm. 2002;59:111–31.
Daly DD, Yoss RE. The treatment of narcolepsy with methyl phenylpiperidylacetate: a preliminary report. Proc Staff Meet Mayo Clin. 1956;31(23):620–5.
Puymirat J, Bouchard JP, Mathieu J. Efficacy and tolerability of a 20-mg dose of methylphenidate for the treatment of daytime sleepiness in adult patients with myotonic dystrophy type 1: a 2-center, randomized, double-blind, placebo-controlled, 3-week crossover trial. Clin Ther. 2012;34(5):1103–11.
Parkes JD, Schachter M. Mazindol in the treatment of narcolepsy. Acta Neurol Scand. 1979;60(4):250–4.
Iijima S, Sugita Y, Teshima Y, Hishikawa Y. Therapeutic effects of mazindol on narcolepsy. Sleep. 1986;9(1 Pt 2):265–8.
Bymaster FP, Katner JS, Nelson DL, Hemrick-Luecke SK, Threlkeld PG, Heiligenstein JH, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2002;27(5):699–711.
Swanson J, Baler RD, Volkow ND. Understanding the effects of stimulant medications on cognition in individuals with attention-deficit hyperactivity disorder: a decade of progress. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2011;36(1):207–26.
Kirov R, Moyanova S. Age-related effect of ritanserin on the sleep-waking phases in rats. Int J Neurosci. 1998;93(3–4):265–78.
Kirov R, Moyanova S. Ritanserin-induced changes in sleep-waking phases in rats. Acta Physiol Pharmacol Bulg. 1995;21(4):87–92.
Lammers GJ, Arends J, Declerck AC, Kamphuisen HA, Schouwink G, Troost J. Ritanserin, a 5-HT2 receptor blocker, as add-on treatment in narcolepsy. Sleep. 1991;14(2):130–2.
Mayer G. Ritanserin improves sleep quality in narcolepsy. Pharmacopsychiatry. 2003;36(4):150–5.
Ruiu S, Marchese G, Saba PL, Gessa GL, Pani L. The 5-HT2 antagonist ritanserin blocks dopamine re-uptake in the rat frontal cortex. Mol Psychiatry. 2000;5(6):673–7.
Garcia PS, Jenkins A. Inhibition of the GABA(A) receptor by a macrolide but not by a lincosamide antibiotic. Annual Meeting of the American Society of Anesthesiologists abstract number A1385; 2009.
Trotti LM, Saini P, Freeman AA, Bliwise DL, Garcia PS, Jenkins A, et al. Improvement in daytime sleepiness with clarithromycin in patients with GABA-related hypersomnia: Clinical experience. J Psychopharmacol. 2013;28(7):697–2.
Rezvanian E, Watson NF. Kleine-levin syndrome treated with clarithromycin. J Clin Sleep Medi JCSM Off Publ Am Acad Sleep Med. 2013;9(11):1211–2.
Bandettini di Poggio M, Anfosso S, Audenino D, Primavera A. Clarithromycin-induced neurotoxicity in adults. J Clin Neurosci Off J Neurosurg Soc Australas. 2011;18(3):313–8.
Jespersen CM, Als-Nielsen B, Damgaard M, Hansen JF, Hansen S, Helo OH, et al. Randomised placebo controlled multicentre trial to assess short term clarithromycin for patients with stable coronary heart disease: CLARICOR trial. BMJ. 2006;332(7532):22–7.
Winkel P, Hilden J, Fischer Hansen J, Hildebrandt P, Kastrup J, Kolmos HJ, et al. Excess sudden cardiac deaths after short-term clarithromycin administration in the CLARICOR trial: why is this so, and why are statins protective? Cardiology. 2011;118(1):63–7.
Cercek B. Increased risk of mortality following antibiotic treatment in patients with coronary artery disease? Cardiology. 2008;111(4):277–9.
Compliance with Ethics Guidelines
Conflict of Interest
Olufemi Adenuga and Hrayr Attarian declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Adenuga, O., Attarian, H. Treatment of Disorders of Hypersomnolence. Curr Treat Options Neurol 16, 302 (2014). https://doi.org/10.1007/s11940-014-0302-9
Published:
DOI: https://doi.org/10.1007/s11940-014-0302-9