Abstract
Neurosyphilis literally means syphilitic infection of the central nervous system, but it is often referred to incorrectly as “tertiary syphilis.” Neurosyphilis can occur at any time in the course of syphilis, even in the earliest, primary, stage. Early forms of neurosyphilis primarily affect the meninges, cerebrospinal fluid, and cerebral or spinal cord vasculature. Late forms of neurosyphilis primarily affect the brain and spinal cord parenchyma. Uveitis and hearing loss related to syphilis are most common in early syphilis and may be accompanied by early neurosyphilis. The treatment for syphilis-related eye disease and hearing loss is the same as the treatment for neurosyphilis. Neurosyphilis is more commonly seen in patients infected with HIV, and much of the recent literature pertains to this risk group. This article provides a critical review of recent literature on the diagnosis, clinical findings, risk factors, and management of neurosyphilis.
Similar content being viewed by others
References and Recommended Reading
Lukehart SA, Hook EW III, Baker-Zander SA, et al.: Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med 1988, 109:855–862.
Wharton M, Chorba TL, Vogt RL, et al.: Case definitions for public health surveillance. MMWR Recomm Rep 1990, 39:1–43.
Marra CM, Maxwell CL, Collier AC, et al.: Interpreting cerebrospinal fluid pleocytosis in HIV in the era of potent antiretroviral therapy. BMC Infect Dis 2007, 7:37.
Marra CM, Maxwell CL, Smith SL, et al.: Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis 2004, 189:369–376.
Ghanem KG, Moore RD, Rompalo AM, et al.: Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS 2008, 22:1145–1151.
Timmermans M, Carr J: Neurosyphilis in the modern era. J Neurol Neurosurg Psychiatry 2004, 75:1727–1730.
Hooshmand H, Escobar MR, Kopf SW: Neurosyphilis. A study of 241 patients. JAMA 1972, 219:726–729.
Castro R, Prieto ES, da Luz Martins Pereira F: Nontreponemal tests in the diagnosis of neurosyphilis: an evaluation of the Venereal Disease Research Laboratory (VDRL) and the Rapid Plasma Reagin (RPR) tests. J Clin Lab Anal 2008, 22:257–261.
Larsen SA, Hambie EA, Wobig GH, Kennedy EJ: Cerebrospinal fluid serologic test for syphilis: treponemal and nontreponemal tests. In Advances in Sexually Transmitted Diseases. Edited by Morisset R, Kurstak E. Utrecht, The Netherlands: VNU Science Press; 1985:157–162.
Davis LE, Schmitt JW: Clinical significance of cerebrospinal fluid tests for neurosyphilis. Ann Neurol 1989, 25:50–55.
Marra CM, Critchlow CW, Hook EW III, et al.: Cerebrospinal fluid treponemal antibodies in untreated early syphilis. Arch Neurol 1995, 52:68–72.
Marra CM, Tantalo LC, Maxwell CL, et al.: Alternative cerebrospinal fluid tests to diagnose neurosyphilis in HIVinfected individuals. Neurology 2004, 63:85–88.
Workowski KA, Berman SM: Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep 2006, 55:1–94.
Symptomatic early neurosyphilis among HIV-positive men who have sex with men-four cities, United States, January 2002–June 2004. MMWR Morb Mortal Wkly Rep 2007, 56:625–628.
Hughes GB, Rutherford I: Predictive value of serologic tests for syphilis in otology. Ann Otol Rhinol Laryngol 1986, 95:250–259.
Becker GD: Late syphilitic hearing loss: a diagnostic and therapeutic dilemma. Laryngoscope 1979, 89:1273–1288.
Yimtae K, Srirompotong S, Lertsukprasert K: Otosyphilis: a review of 85 cases. Otolaryngol Head Neck Surg 2007, 136:67–71.
Jeans AR, Wilkins EG, Bonington A: Sensorineural hearing loss due to secondary syphilis. Int J STD AIDS 2008, 19:355–356.
Klemm E, Wollina U: Otosyphilis: report on six cases. J Eur Acad Dermatol Venereol 2004, 18:429–434.
Mishra S, Walmsley SL, Loutfy MR, et al.: Otosyphilis in HIV-coinfected individuals: a case series from Toronto, Canada. AIDS Patient Care STDS 2008, 22:213–219.
Song JJ, Lee HM, Chae SW, Hwang SJ: Bilateral otosyphilis in a patient with HIV infection. Eur Arch Otorhinolaryngol 2005, 262:972–974.
Aldave AJ, King JA, Cunningham ET Jr: Ocular syphilis. Curr Opin Ophthalmol 2001, 12:433–441.
Ormerod LD, Puklin JE, Sobel JD: Syphilitic posterior uveitis: correlative findings and significance. Clin Infect Dis 2001, 32:1661–1673.
Zwink FB, Dunlop EM: Clinically silent anterior uveitis in secondary syphilis. Trans Ophthalmol Soc U K 1976, 96:148–150.
Kitson MT, Yong MK, Hoy JF: Ocular syphilis: are we seeing all there is to see? Med J Aust 2008, 189:411.
Joseph A, Rogers S, Browning A, et al.: Syphilitic acute posterior placoid chorioretinitis in nonimmuno-compromised patients. Eye 2007, 21:1114–1119.
Chao JR, Khurana RN, Fawzi AA, et al.: Syphilis: reemergence of an old adversary. Ophthalmology 2006, 113:2074–2079.
Doris JP, Saha K, Jones NP, Sukthankar A: Ocular syphilis: the new epidemic. Eye 2006, 20:703–705.
Parc CE, Chahed S, Patel SV, Salmon-Ceron D: Manifestations and treatment of ocular syphilis during an epidemic in France. Sex Transm Dis 2007, 34:553–556.
Balba GP, Kumar PN, James AN, et al.: Ocular syphilis in HIV-positive patients receiving highly active antiretroviral therapy. Am J Med 2006, 119:448 e21–5.
Kiss S, Damico FM, Young LH: Ocular manifestations and treatment of syphilis. Semin Ophthalmol 2005, 20:161–167.
Zamani M, Garfinkel RA: Corticosteroid-induced modulation of acute syphilitic posterior placoid chorioretinitis. Am J Ophthalmol 2003, 135:891–894.
Erol N, Topbas S: Acute syphilitic posterior placoid chorioretinitis after an intravitreal triamcinolone acetonide injection. Acta Ophthalmol Scand 2006, 84:435.
Song JH, Hong YT, Kwon OW: Acute syphilitic posterior placoid chorioretinitis following intravitreal triamcinolone acetonide injection. Graefes Arch Clin Exp Ophthalmol 2008, 246:1775–1778.
Gordon SM, Eaton ME, George R, et al.: The response of symptomatic neurosyphilis to high-dose intravenous penicillin G in patients with human immunodeficiency virus infection. N Engl J Med 1994, 331:1469–1473.
Fathilah J, Choo MM: The Jarisch-Herxheimer reaction in ocular syphilis. Med J Malaysia 2003, 58:437–439.
Gurses C, Bilgic B, Topcular B, et al.: Clinical and magnetic resonance imaging findings of HIV-negative patients with neurosyphilis. J Neurol 2007, 254:368–374.
Noone ML, Sinha S, Taly AB, Chandrika S: Periodic lateralized epileptiform discharges in neurosyphilis. Epilepsia 2007, 48:390–393.
Chang YP, Lin RT, Liu CK, et al.: Neurosyphilis presenting with status epilepticus. Neurologist 2006, 12:314–317.
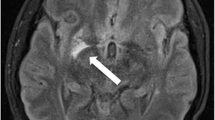
Bash S, Hathout GM, Cohen S: Mesiotemporal T2-weighted hyperintensity: neurosyphilis mimicking herpes encephalitis. AJNR Am J Neuroradiol 2001, 22:314–316.
Szilak I, Marty F, Helft J, Soeiro R: Neurosyphilis presenting as herpes simplex encephalitis. Clin Infect Dis 2001, 32:1108–1109.
Marano E, Briganti F, Tortora F, et al.: Neurosyphilis with complex partial status epilepticus and mesiotemporal MRI abnormalities mimicking herpes simplex encephalitis. J Neurol Neurosurg Psychiatry 2004, 75:833.
Lansberg MG, O’Brien MW, Norbash AM, et al.: MRI abnormalities associated with partial status epilepticus. Neurology 1999, 52:1021–1027.
Hicdonmez T, Utku U, Turgut N, et al.: Reversible postictal MRI change mimicking structural lesion. Clin Neurol Neurosurg 2003, 105:288–290.
Polnikorn N, Witoonpanich R, Vorachit M, et al.: Penicillin concentrations in cerebrospinal fluid after different treatment regimens for syphilis. Br J Vener Dis 1980, 56:363–367.
van der Valk PG, Kraai EJ, van Voorst Vader PC, et al.: Penicillin concentrations in cerebrospinal fluid (CSF) during repository treatment regimen for syphilis. Genitourin Med 1988, 64:223–225.
Tramont EC: Persistence of Treponema pallidum following penicillin G therapy. Report of two cases. JAMA 1976, 236:2206–2207.
Berry CD, Hooton TM, Collier AC, Lukehart SA: Neurologic relapse after benzathine penicillin therapy for secondary syphilis in a patient with HIV infection. N Engl J Med 1987, 316:1587–1589.
Walter T, Lebouche B, Miailhes P, et al.: Symptomatic relapse of neurologic syphilis after benzathine penicillin G therapy for primary or secondary syphilis in HIV-infected patients. Clin Infect Dis 2006, 43:787–790.
Richards BW, Hessburg TJ, Nussbaum JN: Recurrent syphilitic uveitis. N Engl J Med 1989, 320:62.
Taylor MM, Aynalem G, Olea LM, et al.: A consequence of the syphilis epidemic among men who have sex with men (MSM): neurosyphilis in Los Angeles, 2001–2004. Sex Transm Dis 2008, 35:430–434.
Poliseli R, Vidal JE, Penalva De Oliveira AC, Hernandez AV: Neurosyphilis in HIV-infected patients: clinical manifestations, serum venereal disease research laboratory titers, and associated factors to symptomatic neurosyphilis. Sex Transm Dis 2008, 35:425–429.
Libois A, De Wit S, Poll B, et al.: HIV and syphilis: when to perform a lumbar puncture. Sex Transm Dis 2007, 34:141–144.
Zetola NM, Klausner JD: Syphilis and HIV infection: an update. Clin Infect Dis 2007, 44:1222–1228.
Moore J: Studies in asymptomatic neurosyphilis II. The classification, treatment, and prognosis of early asymptomatic neurosyphilis. Bull Johns Hopkins Hosp 1922, 33:231–246.
Rolfs RT, Joesoef MR, Hendershot EF, et al.: A randomized trial of enhanced therapy for early syphilis in patients with and without human immunodeficiency virus infection. The Syphilis and HIV Study Group. N Engl J Med 1997, 337:307–314.
Shann S, Wilson J: Treatment of neurosyphilis with ceftriaxone. Sex Transm Infect 2003, 79:415–416.
Dowell ME, Ross PG, Musher DM, et al.: Response of latent syphilis or neurosyphilis to ceftriaxone therapy in persons infected with human immunodeficiency virus. Am J Med 1992, 93:481–488.
Marra CM, Boutin P, McArthur JC, et al.: A pilot study evaluating ceftriaxone and penicillin G as treatment agents for neurosyphilis in human immunodeficiency virusinfected individuals. Clin Infect Dis 2000, 30:540–544.
Marra CM, Maxwell CL, Tantalo L, et al.: Normalization of cerebrospinal fluid abnormalities after neurosyphilis therapy: does HIV status matter? Clin Infect Dis 2004, 38:1001–1006.
Marra CM, Maxwell CL, Tantalo LC, et al.: Normalization of serum rapid plasma reagin titer predicts normalization of cerebrospinal fluid and clinical abnormalities after treatment of neurosyphilis. Clin Infect Dis 2008, 47:893–899.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marra, C.M. Update on neurosyphilis. Curr Infect Dis Rep 11, 127–134 (2009). https://doi.org/10.1007/s11908-009-0019-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-009-0019-1