Abstract
Several particle engineering technologies have recently emerged, which have enabled inhaled microspheres to seek to manipulate pulmonary biopharmaceuticals, and to improve therapeutic efficacy for both local and systemic treatments. These microspheres may be designed to sustain drug release, to prolong lung retention, to achieve drug targeting and/or to enhance drug absorption and thereby, to seek the potentials of reducing dosing frequency and/or drug dose, while maintaining therapeutic efficacy and/or reducing adverse effects. While product development is still in process, in many cases, considerable therapeutic benefits and/or new therapeutic opportunities can be envisaged. ‘Proof-of-concept’ results are now available for various drug classes including β2-adrenoceptor agonists, corticosteroids, antimycobacterial antibacterials, estradiol and therapeutic macromolecules such as insulin. Nevertheless, their development success must overcome several critical and unique challenges including toxicological evaluations of microsphere materials, and, clearly, successful products should meet the needs of the patient and the market place. Unfortunately, such issues have not always been addressed or examined adequately in the current studies, and thus we may anticipate paradigm shifts in the research of several groups seeking to develop products with improved therapeutic profiles. Nevertheless, it seems likely that improved inhalation products, with greater therapeutic efficacy and reduced adverse effects, will result from next-generation respirable microspheres. These may be expected to contain drugs intended for both local and systemic activity.





Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Dipiro JT, Talbert RL, Yee GC, et al., editors. Pharmacotherapy. 5th ed. Chapter 26: Asthma, Chapter 27: Chronic obstructive pulmonary disease, Chapter 74: Diabetes mellitus, Chapter 83: Hormone replacement therapy and Chapter 110: Tuberculosis. New York: McGraw-Hill, 2002
Patton JS. Mechanisms of macromolecule absorption by the lungs. Adv Drug Deliv Rev 1996; 19: 3–36
Adjei AL, Gupta PK, editors. Inhalation delivery of therapeutic peptides and proteins. New York: Marcel Dekker, 1997
Byron PR, Sakagami M, Rypacek F. New pulmonary biopharmaceutics: rate-determining absorption and macro-molecular transporters. In: Dalby RN, Byron PR, Farr SJ, et al., editors. Respiratory drug delivery VII. Raleigh (NC): Serentec Press, 2000: 41–8
Hochhaus G, Derendorf H, Talton J, et al. Factors involved in the pulmonary targeting of inhaled glucocorticoids. In: Schleimer RP, O’Byrne PM, Szefler SJ, et al., editors. Inhaled steroids in asthma. New York: Marcel Dekker, 2002: 283–307
Rosenborg J, Borgstrom L, Jendbro M, et al. Long-acting beta-agonists: pharmacokinetic an dynamic insights conferred by altered routes and modes of administration. In: Dalby RN, Byron PR, Farr SJ, et al., editors. Respiratory drug delivery VII. Raleigh (NC): Serentec Press, 2000: 49–58
Zeng XM, Martin GP, Marriott C. The controlled delivery of drugs to the lung. Int J Pharm 1995; 124: 149–64
Pritchard JN. Controlled delivery: can you really convert a good drug into a great one? In: Dalby RN, Byron PR, Farr SJ, et al., editors. Respiratory drug delivery VIII. Raleigh (NC): David Horwood International Publishing, 2002: 249–56
Peart J, Clarke MJ. New developments in dry powder inhaler technology. Am Pharm Rev 2001; Fall: 37–45
Edwards DA, Dunbar C. Bioengineering of therapeutic aerosols. Annu Rev Biomed Eng 2002; 4: 93–107
Byron PR. Prediction of drug residence times in regions of the human respiratory tract following aerosol inhalation. J Pharm Sci 1986; 75: 433–8
Lansley AB. Mucociliary clearance and drug delivery via the respiratory tract. Adv Drug Deliv Rev 1993; 11: 299–327
Bowden DH. The alveolar macrophage. Environ Health Perspect 1984; 55: 327–41
Jones BG, Dickinson PA, Gumbleton M, et al. The inhibition of phagocytosis of respirable microspheres by alveolar and peritoneal macrophages. Int J Pharm 2002; 236: 65–79
Byron PR, Philips EM. Absorption, clearance and dissolution in the lung. In: Byron PR, editor. Respiratory drug delivery. Boca Raton (FL): CRC Press, 1990: 107–42
Byron PR, Patton JS. Drug delivery via the respiratory tract. J Aerosol Med 1994; 7: 49–75
Byron PR. Physicochemical effects on lung disposition of pharmaceutical aerosols. Aerosol Sci Technol 1993; 18: 223–9
Gudapaty SR, Liener IE, Hoidal JR, et al. The prevention of elastase-induced emphysema in hamsters by intratracheal administration of a synthetic elastase inhibitor bound to albumin microspheres. Am Rev Respir Dis 1985; 132: 159–63
Lai Y, Mehta RC, Thacker AA, et al. Sustained bronchodilation with isoproterenol poly(glycolide-co-lactide) microspheres. Pharm Res 1993; 10: 119–25
Ben-Jebria A, Chen D, Eskew ML, et al. Large porous particles for sustained protection from carbachol-induced bronchoconstriction in guinea pigs. Pharm Res 1999; 16: 555–61
Sakagami M, Kinoshita W, Sakon K, et al. Mucoadhesive beclomethasone microspheres for powder inhalation: their pharmacokinetics and pharmacodynamics evaluation. J Control Release 2002; 80: 207–18
Talton J, Fitz-Gerald J, Singh R, et al. Nano-thin coating for improved lung targeting of glucocorticoid dry powders: in-vitro and in-vivo characteristics. In: Dalby RN, Byron PR, Farr SJ, et al., editors. Respiratory drug delivery VII. Raleigh (NC): Serentec Press, 2000: 67–74
Suarez S, O’Hara P, Kazantseva M, et al. Airways delivery of rifampicin microparticles for the treatment of tuberculosis. J Antimicrob Chemother 2001; 48: 431–4
Suarez S, O’Hara P, Kazantseva M, et al. Respirable PLGA microspheres containing rifampicin for the treatment of tuberculosis: screening in an infectious disease model. Pharm Res 2001; 18: 1315–9
Sharma R, Saxena D, Dwivedi AK, et al. Inhalable microparticles containing drug combinations to target alveolar macrophages for treatment of pulmonary tuberculosis. Pharm Res 2001; 18: 1405–10
Anderson PJ, Zhou X, Breen P, et al. Pharmacokinetics of (R,S)-albuterol after aerosol inhalation in healthy adult volunteers. J Pharm Sci 1998; 87: 841–4
Nelson HS. Beta-adrenergic bronchodilators. N Engl J Med 1995; 333: 499–506
Drazen JM, Israel E, Boushey HA, et al. Comparison of regularly scheduled with as-needed use of albuterol in mild asthma: asthma clinical research networks. N Engl J Med 1996; 335: 841–7
Hunter AC, Moghimi SM. Therapeutic synthetic polymers: a game of Russian roulette? Drug Discov Today 2002; 7: 998–1001
Wang J, Ben-Jebria A, Edwards DA. Inhalation of estradiol for sustained systemic delivery. J Aerosol Med 1999; 12: 27–36
Hrkash J, Batycky R, Chen D, et al. AIR insulin: complete diabetes therapy via inhalation of fast-acting and slow-acting dry powder aerosols [abstract]. Diabetes 2000; 49: A9
Edwards DA, Hanes J, Caponetti G, et al. Large porous particles for pulmonary drug delivery. Science 1997; 276: 1868–71
Kawashima Y, Yamamoto H, Takeuchi H, et al. Pulmonary delivery of insulin with nebulized DL-lactide/glycolide copolymer (PLGA) nanospheres to prolong hypoglycemic effects. J Control Release 1999; 62: 279–87
Blair J, Coghlan D, Langner E, et al. Sustained delivery of insulin via the lung using Solidose® technology. In: Dalby RN, Byron PR, Farr SJ, et al., editors. Respiratory drug delivery VIII. Raleigh (NC): Davis Horwood International Publishing, 2002: 411–3
Garcia-Contreras L, Morcöl T, Bell SJD, et al. Evaluation of novel particles as pulmonary delivery systems for insulin in rats. AAPS PharmSci 2003; 5: 83–93
Steiner S, Pfutzner A, Wilson BR, et al. Technosphere™/insulin: proof of concept study with a new insulin formulation for pulmonary delivery. Exp Clin Endocrinol Diabetes 2002; 110: 17–21
Smith DJ, Gambone LM, Tarara T, et al. Liquid dose pulmonary instillation of gentamicin Pulmospheres® formulations: tissue distribution and pharmacokinetics in rabbits. Pharm Res 2001; 18: 1556–61
Bot AI, Tarara TE, Smith DJ, et al. Novel lipid-based hollow-porous microparticles as a platform for immunoglobulin delivery to the respiratory tract. Pharm Res 2000; 17: 275–83
Morimoto K, Katsumata H, Yabuta T, et al. Gelatin microspheres as a pulmonary delivery system: evaluation of salmon calcitonin absorption. J Pharm Pharmacol 2000; 52: 611–7
Brattsand R. Drug development of inhaled steroids. In: Schleimer RP, O’Byrne PM, Szefler SJ, et al., editors. Inhaled steroids in asthma. New York: Marcel Dekker, 2002: 3–33
Nagai T, Machida Y, Suzuki Y, et al. Method and preparation for administration to the mucosa of the oral or nasal cavity. US Patent 4,226,848, 1980 Oct 7
Okuda M, Okamoto M, Nomura Y, et al. Clinical study on beclomethasone dipropionate powder preparation (TL-102) in perennial nasal allergy. Rhinology 1986; 24: 113–23
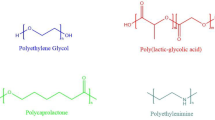
Li S, Vert M. Biodegradable polymers: polyesters. In: Mathiowitz E, editor. Encyclopedia of controlled drug delivery. New York: John Wiley, 1999: 71–93
Jendbro M, Johansson C-J, Strandberg P, et al. Pharmacokinetics of budesonide and its major ester metabolite after inhalation and intravenous administration of budesonide in the rat. Drug Metab Dispos 2001; 29: 769–76
Kim A, Krasnova TK, Romanova V. Use of inhalation of ultrasonic aerosols and galvanic current in the treatment of patients with pulmonary tuberculosis. Ter Arkh 1987; 59: 96–8
Yokota S, Miki K. Effects of INH (Isoniazid) inhalation in patients with endobronchial tuberculosis (EBTB). Kekkaku 1999; 74: 873–7
FDA, US Public Health Service, Department of Health and Human Services. US FDA enforcement report [online]. Available from URL: http://www.fda.gov/bbs/topics/ENFORCE/ENF00006.html [Accessed 2005 Feb 10]
Sturdee DW. Current hormone replacement therapy: what are the shortcomings? Advances in delivery. Int J Clin Pract 1999; 53: 468–72
White CM, Ferraro-Borgida MJ, Fossati AT, et al. The pharmacokinetics of intravenous estradiol: preliminary study. Pharmacotherapy 1998; 18: 1343–6
Schulz H, Brand P, Kohlhaufl M, et al. Application of estradiol by large porous particle inhalation [abstract]. J Aerosol Med 1999; 12: 98
Heinemann L, Pfutzner A, Heise T. Alternative routes of administration as an approach to improve insulin therapy: update on dermal, oral, nasal and pulmonary insulin delivery. Curr Pharm Des 2001; 7: 1327–51
Heinemann L, Traut T, Heise T. Time-action profile of inhaled insulin. Diabetic Med 1997; 14: 63–72
Sakagami M. Insulin disposition in the lung following oral inhalation in humans: a meta-analysis of its pharmacokinetics. Clin Pharmacokinet 2004; 43(8): 539–52
Farr SJ, McElduff A, Mather LE, et al. Pulmonary insulin administration using the AERx® system: physiological and physiochemical factors influencing insulin effectiveness in healthy fasting subjects. Diabetes Technol Ther 2000; 2: 185–97
BioSante Pharmaceuticals. Protein delivery (insulin) [online]. Available from URL: http://www.biosantepharma.com/products/protein_delivery.html [Accessed 2005 Feb 10]
Hill MR, Vaughan LM. Effect of delivery mode on pharmacokinetics of inhaled drugs: experience with beclomethasone. In: Dalby RN, Byron PR, Farr SJ, editors. Respiratory drug delivery VI. Buffalo Grove (IL): Interpharm Press, 1998: 53–60
Patton JS, Bukar J, Nagarajan S. Inhaled insulin. Adv Drug Deliv Rev 1999; 35: 235–47
Tracy MA. Development and scale-up of microsphere protein delivery system. Biotechnol Prog 1998; 14: 108–15
Stefely JS. Novel excipients for inhalation drug delivery: expanding the capability of the MDI. Drug Delivery Technology [online]. Available from URL: http://drugdeliverytech.com/cgi-bin/articles.cgi?.idArticle=76 [Accessed 2005 Feb 10]
Armstrong DJ, Elliott PN, Ford JL, et al. Poly-(D,L-lactic acid) microspheres incorporating histological dyes for intra-pulmonary histopathological investigations. J Pharm Pharmacol 1996; 48: 258–62
Hastings RH, Grady M, Sakuma T, et al. Clearance of different-sized proteins from the alveolar space in humans and rabbits. J Appl Physiol 1992; 73: 1310–6
Liggett SB, Green SA. Molecular biology of the beta2-adrenergic receptor: focus on interactions of agonist with receptor. In: Romain P, O’Byrne PM, editors. Beta2-agonists in asthma treatment. New York: Marcel Dekker, 1997: 19–34
Brindley C, Falcoz C, Mackie AE, et al. Absorption kinetics after inhalation of fluticasone propionate via the Diskhaler®, Diskus® and metered-dose inhaler in healthy volunteers. Clin Pharmacokinet 2000; 39 Suppl. 1: 1–8
Donnelly R, Seale JP. Clinical pharmacokinetics of inhaled budesonide. Clin Pharmacokinet 2001; 40: 427–40
Garcia-Marcos L, Schuster A, Cobos Barroso N. Inhaled corticosteroids plus long-acting beta(2)-agonists as a combined therapy in asthma. Expert Opin Pharmacother 2003; 4: 23–39
Gualandi-Signorini AM, Giorgi G. Insulin formulations: a review. Eur Rev Med Pharmacol Sci 2001; 5: 73–83
Davis SS. Parenteral polymers. Drug Discov Today 2002; 7: 1159–61
Acknowledgements
The authors are grateful to Joanne Peart, PhD, for sharing her insights on this subject. The Medical College of Virginia Foundation has supported this research and the authors. There are no conflicts of interest regarding this research and publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sakagami, M., Byron, P.R. Respirable Microspheres for Inhalation. Clin Pharmacokinet 44, 263–277 (2005). https://doi.org/10.2165/00003088-200544030-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200544030-00004