Summary
The current symptomatic treatment of Parkinson’s disease mainly relies on agents which are able to restore dopaminergic transmission in the nigrostriatal pathway, such as the dopamine precursor levodopa or direct agonists of dopamine receptors. Ancillary strategies include the use of anticholinergic and antiglutamatergic agents or inhibitors of cerebral dopamine catabolism, such as monoamine oxidase type B inhibitors.
Levodopa is the most widely used and effective drug. Its peculiar pharmacokinetics are characterised by an extensive presystemic metabolism, overcome by the combined use of extracerebral inhibitors of the enzyme aromatic-aminoacid decarboxylase and rapid absorption in the proximal small bowel by a saturable facilitated transport system shared with other large neutral amino acids. Drug transport from plasma to the brain is mediated by the same carriers operating in the intestinal mucosa. The main strategies to assure reproducibility of both drug intestinal absorption and delivery to the brain and clinical effect include standardisation of levodopa administration with respect to meal times and a controlled dietary protein intake.
The levodopa plasma half-life is very short, resulting in marked plasma drug concentration fluctuations which are matched, as the disease progresses, with swings in the therapeutic response (‘wearing-off’ phenomena). ‘Wearing-off’ phenomena can be also associated, at the more advanced disease stages with a ‘negative’, both parkinsonism-exacerbating and dyskinetic effect of levodopa at subtherapeutic plasma concentrations. Dyskinesias may be also related to high-levodopa, excessive plasma concentrations. Recognition of the different levodopa toxic response patterns can be difficult on a clinical basis alone, and simultaneous monitoring of levodopa concentration-effect relationships may prove useful to disclose the underlying mechanism and in planning the correct pharmacokinetic management.
Controlled-release levodopa formulations have been developed in an attempt to smooth out fluctuations in plasma profiles and matched therapeutic responses. The delayed levodopa absorption and lower plasma concentrations which characterise controlled-release formulations compared with standard forms must be taken into account when prescribing dosage regimens and can be complicating factors in the management of the advanced disease stages.
The pharmacokinetic and pharmacodynamic characterisation of the other anti-parkinsonian agents is hampered by the lack of sensitive and specific analytical methods to measure their very low plasma drug concentrations and by the difficulty in quantitatively assessing overall moderate drug clinical effects. In clinical practice an optimal dosage schedule is still generally found for each patient on an empirical basis.
Future strategies should focus on the search for pharmacological agents with a better kinetic profile, particularly a higher and reproducible bioavailability and a predictable relationship between plasma drug concentration and clinical response. Treatments aimed not only at controlling the symptoms, but also at slowing the neurodegenerative process, are currently under intensive investigation.
Similar content being viewed by others
References
Marsden CD. Parkinson’s disease. J Neurol Neurosurg Psychiatry 1994; 57: 672–81
Jankovic J, Marsden CD. Therapeutic strategies in Parkinson’s disease. In: Jankovic J, Tolosa E, editors. Parkinson’s disease and movement disorders. Baltimore: Williams & Wilkins, 1993: 115–44
Parker BM, Cusack BJ, Vestal RE. Pharmacokinetic optimisation of drug therapy in elderly patients. Drugs Aging 1995; 7: 10–8
Nutt JG, Fellman JH. Pharmacokinetics of levodopa. Clin Neuropharmacol 1984; 7: 35–49
Leenders KL, Palmer AJ, Quinn N, et al. Brain dopamine metabolism in patients with Parkinson’s disease measured with positron emission tomography. J Neurol Neurosurg Psychiatry 1986; 49: 853–60
Tedroff J, Aquilonius SM, Hartvig P, et al. Cerebral uptake and utilization of therapeutic beta-11C-L-dopa in Parkinson’s disease measured by positron emission tomography. Relations to motor response. Acta Neurol Scand 1992; 85: 95–102
Vingerhoets FJG, Snow BJ, Lee CS, et al. Longitudinal fluorodopa positron emission tomographic studies of the evolution of idiopathic parkinsonism. Ann Neurol 1994; 36: 759–64
Nutt JG. On-off phenomenon: relation to levodopa pharmacokinetics and pharmacodynamics. Ann Neurol 1987; 22: 535–40
Andersson I, Granerus AK, Jagenburg R, et al. Intestinal decarboxylation of orally administered L-dopa. Acta Med Scand 1975; 198: 415–20
Pinder RM, Brogden RN, Sawyer PR, et al. Levodopa and decarboxylase inhibitors: a review of their clinical pharmacology and use in the treatment of Parkinsonism. Drugs 1976; 11: 329–77
Tissot R, Bartholini G, Pletscher A. Drug-induced changes of extracerebral dopa metabolism in man. Arch Neurol 1969; 20: 187–90
Robertson DRC, Wood ND, Everest H, et al. The effect of age on the pharmacokinetics of levodopa administered alone and in the presence of carbidopa. Br J Clin Pharmacol 1989; 28: 61–9
Hoehn MM. Increased dosage of carbidopa in patients with Parkinson’s disease receiving low doses of levodopa. Arch Neurol 1980; 37: 146–9
Bermejo Pareja F, Martinez-Martin P, Muradas V, et al. Carbidopa dosage modifies L-dopa induced side effects and blood levels of L-dopa and other amino acids in advanced parkinsonism. Acta Neurol Scand 1985; 72: 506–11
Cedarbaum JM, Kutt H, Dhar AK, et al. Effect of supplemental carbidopa on bioavailability of L-dopa. Clin Neuropharmacol 1986; 9: 153–9
Jaffe ME. Clinical studies of carbidopa and l-dopa in the treatment of Parkinson’s disease. In: Yahr MD, editor. Advances in neurology. New York: Raven Press, 1973: 161–72
Tourtellotte JW, Syndulko K, Potvin AR, et al. Increased ratio of carbidopa to levodopa in treatment of Parkinson’s disease. Arch Neurol 1980; 37: 723–6
Rinne UK, Molsa P. Levodopa with benserazide or carbidopa in Parkinson disease. Neurology 1979; 29: 1584–9
Oertel WH, Dodel RC. International guide to drugs for Parkinson’s disease. Mov Disord 1995; 10: 121–31
Wade DN, Mearrick PT, Morris J. Active transport of L-dopa in the intestine. Nature 1973; 242: 463–5
Rivera-Calimlim L, Dujovne CA, Morgan JP, et al. L-dopa treatment failure: explanation and correction. BMJ 1970; 4: 93–4
Nutt JG, Woodward WR, Hammerstad JP, et al. The ‘on-off’ phenomenon in Parkinson’s disease. Relation to levodopa absorption and transport. N Engl J Med 1984; 310: 483–8
Baruzzi A, Contin M, Riva R, et al. Influence of meal ingestion time on pharmacokinetics of orally administered levodopa in Parkinsonian patients. Clin Neuropharmacol 1987; 10: 527–37
Algeri S, Cerletti C, Curcio M, et al. Effect of anticholinergic drugs on gastro-intestinal absorption of L-dopa in rats and in man. Eur J Clin Pharmacol 1976; 35: 293–9
Contin M, Riva R, Martinelli P, et al. Combined levodopa-anti-cholinergic therapy in the treatment of Parkinson’s disease: effect on levodopa bioavailability. Clin Neuropharmacol 1991; 14: 148–55
Morgan JP, Rivera-Calimlim L, Messiha F, et al. Imipramine-mediated interference with levodopa absorption from the gastrointestinal tract in man. Neurology 1975; 25: 1029–34
Waller DG, Roseveare C, Renwick AG, et al. Gastric emptying in healthy volunteers after multiple doses of levodopa. Br J Clin Pharmacol 1991; 32: 691–5
Bentuè-Ferrer D, Allain H, Reymann JM, et al. Lack of pharmacokinetic influence on levodopa by bromocriptine. Clin Neuropharmacol 1988; 11: 83–6
Contin M, Riva R, Martinelli P, et al. No effect of chronic bromocriptine therapy on levodopa pharmacokinetics in patients with Parkinson’s disease. Clin Neuropharmacol 1992; 15: 505–8
Rabey JM, Schwartz M, Graff E, et al. The influence of bromocriptine on the pharmacokinetics of levodopa in Parkinson’s disease. Clin Neuropharmacol 1991; 14: 514–22
Goetz CG, Thelen JA, MacLeod CM, et al. Blood levodopa levels and Unified Parkinson’s Disease Rating Scale function: with and without exercise. Neurology 1993; 43: 1040–2
Carter JH, Nutt JG, Woodward WR. The effect of exercise on levodopa absorption. Neurology 1992; 42: 2042–5
Rivera-Calimlim L, Morgan JP, Dujovne CA, et al. L-dopa absorption and metabolism by the human stomach. J Clin Invest 1970; 49: 79a
Contin M, Riva R, Martinelli P, et al. Response to a standard oral levodopa test in Parkinsonian patients with and without motor fluctuations. Clin Neuropharmacol 1990; 13: 19–28
Gancher ST, Nutt JG, Woodward WR. Peripheral pharmacokinetics of levodopa in untreated, stable and fluctuating Parkinsonian patients. Neurology 1987; 37: 940–4
Kaakkola S, Mannisto PT, Nissinen E, et al. The effect of an increased ratio of carbidopa to levodopa on the pharmacokinetics of levodopa. Acta Neurol Scand 1985; 72: 385–91
Robertson DRC, Renwick AG, Macklin B, et al. The influence of levodopa on gastric emptying in healthy elderly volunteers. Eur J Clin Pharmacol 1992; 42: 409–12
Verhagen Metman L, Hoff J, Mouradian MM, et al. Fluctuations in plasma levodopa and motor responses with liquid and tablet levodopa/carbidopa. Mov Disord 1994; 9: 463–5
Leenders KL, Poewe WH, Palmer AJ, et al. Inhibition of l-(18F) fluorodopa uptake into human brain by amino acids demonstrated by positron emission tomography. Ann Neurol 1986; 20: 258–62
Mena I, Cotzias GC. Protein intake and treatment of Parkinson’s disease with levodopa. N Engl J Med 1975; 292: 181–4
Pincus JH, Barry K. Influence of dietary protein on motor fluctuations in Parkinson’s disease. Arch Neurol 1987; 44: 270–2
Pincus JH, Barry KM. Plasma levels of amino acids correlate with motor fluctuations in Parkinsonism. Arch Neurol 1987; 44: 1006–9
Berry EM, Growdon JH, Wurtman JJ, et al. A balanced carbohydrate: protein diet in the management of Parkinson’s disease. Neurology 1991; 41: 1295–7
Committee on dietary allowances food and nutrition board, editor. Recommended dietary allowances. Washington, DC: National Academy Press, 1989
Juncos JL, Fabbrini G, Mouradian MM, et al. Dietary influences on the antiparkinsonian response to levodopa. Arch Neurol 1987; 44: 1003–5
Messiha F, Hsu T, Bianchine J. Peripheral aromatic L-amino-acids decarboxylase inhibitor in parkinsonism I: effect on O-methylated metabolites of L-2-14C-dopa. J Clin Invest 1972; 51: 452–5
Guldberg HC, Marsden CA. Catechol-O-methyl transferase: pharmacological aspects and physiological role. Pharmacol Rev 1975; 27: 135–206
Sharpless NS, Muenter MD, Tyce GM, et al. 3-Methoxy-4-hydroxyphenylalanine (3-O-methyldopa) in plasma during oral l-dopa therapy of patients with Parkinson’s disease. Clin Chim Acta 1972; 37: 359–69
Pilling JB, Baker J, Iversen LL, et al. Plasma concentrations of L-dopa and 3-methoxydopa and improvement in clinical ratings and motor performance in patients with Parkinsonism treated with L-dopa alone or in combination with amantadine. J Neurol Neurosurg Psychiatry 1975; 38: 129–35
Wade LA, Katzman R. 3-O-methyldopa uptake and inhibition of l-dopa at the blood-brain barrier. Life Sci 1975; 17: 131–6
Reches A, Fahn S. 3-O-methyldopa blocks dopa metabolism in rat corpus striatum. Ann Neurol 1982; 12: 267–71
Gervas JJ, Muradas V, Bazan E, et al. Effects of 3-OM-dopa on monoamine metabolism in rat brain. Neurology 1983; 33: 278–82
Nutt JG, Woodward WR, Gancher ST, et al. 3-O-methyldopa and the response to levodopa in Parkinson’s disease. Ann Neurol 1987; 21: 584–8
Guttman M, Leger G, Cedarbaum JM, et al. 3-O-methyldopa administration does not alter fluorodopa transport into the brain. Ann Neurol 1992; 31: 638–43
Nelson MV, Berchou RC, Lewitt PA, et al. Pharmacokinetic and pharmacodynamic modeling of l-dopa plasma concentrations and clinical effects in Parkinson’s disease after Sinemet. Clin Neuropharmacol 1989; 12: 91–7
Bredberg E, Tedroff J, Aquilonius SM, et al. Pharmacokinetics and effects of levodopa in advanced Parkinson’s disease. Eur J Clin Pharmacol 1990; 39: 385–9
Contin M, Riva R, Martinelli P, et al. Effect of age on the pharmacokinetics of oral levodopa in patients with Parkinson’s disease. Eur J Clin Pharmacol 1991; 41: 463–6
Campbell NRC, Rankine D, Goodridge AE, et al. Sinemet-ferrous sulphate interaction in patients with Parkinson’s disease. Br J Clin Pharmacol 1990; 30: 599–605
Muenter MD, Tyce GM. L-dopa therapy of Parkinson’s disease: plasma l-dopa concentration, therapeutic response, and side effects. Mayo Clin Proc 1971; 46: 231–9
Koller WC. Alternate day levodopa therapy in parkinsonism. Neurology 1982; 32: 324–6
Quattrone A, Zappia M. Oral pulse levodopa therapy in mild Parkinson’s disease. Neurology 1993; 43: 1161–6
Pfeiffer R. Optimization of levodopa therapy. Neurology 1992; 42 Suppl. 1; 39–43
Koller WC. Initiating treatment of Parkinson’s disease. Neurology 1992; 42 Suppl. 1; 33–8
Mizuno Y, Mori H, Kondo T. Practical guidelines for the drug treatment of Parkinson’s disease. CNS Drugs 1994; 1: 410–26
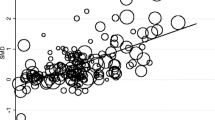
Contin M, Riva R, Martinelli P, et al. Longitudinal monitoring of the levodopa concentration-effect relationship in Parkinson’s disease. Neurology 1994; 44: 1287–92
Contin M, Riva R, Martinelli P, et al. Rate of motor response to oral levodopa and the clinical progression of Parkinson’s disease. Neurology 1996; 46: 1055–8
Fabbrini G, Juncos JL, Mouradian MM, et al. Levodopa pharmacokinetic mechanisms and motor fluctuations in Parkinson’s disease. Ann Neurol 1987; 21: 370–6
Nutt JG, Woodward WR. Levodopa pharmacokinetics and pharmacodynamics in fluctuating parkinsonian patients. Neurology 1986; 36: 739–44
Melamed E, Bitton V, Zelig O. Episodic unresponsiveness to single doses of l-dopa in parkinsonian fluctuators. Neurology 1986; 36: 100–3
Kurlan R, Rothfield KP, Woodward WR, et al. Erratic gastric emptying of levodopa may cause ‘random’ fluctuations of parkinsonian mobility. Neurology 1988; 38: 419–21
Kurth MC, Tetrud JW, Irwin I, et al. Oral levodopa/carbidopa solution versus tablets in Parkinson’s patients with severe fluctuations: a pilot study. Neurology 1993; 43: 1036–9
Steiger MJ, Stocchi F, Bramante L, et al. The clinical efficacy of single morning doses of levodopa methyl ester: dispersible Madopar and Sinemet plus in Parkinson disease. Clin Neuropharmacol 1992; 15: 501–4
Fornadi F, Milani F, Werner M. Madopar dispersible in the treatment of advanced parkinson’s disease. Clin Neuropharmacol 1994; 17 (3 Suppl.): 7S–15S
Neira WD, Sanchez V, Mena MA, et al. The effects of cisapride on plasma l-dopa levels and clinical response in Parkinson’s disease. Mov Disord 1995; 10: 66–70
Djaldetti R, Koren M, Ziv I, et al. Effect of cisapride on response fluctuations in Parkinson’s disease. Mov Disord 1995; 10: 81–4
Carter JH, Nutt JG, Woodward WR, et al. Amount and distribution of dietary protein affects clinical response to levodopa in Parkinson’s disease. Neurology 1989; 39: 552–6
Pincus JH, Barry K. Protein redistribution diet restores motor function in patients with dopa-resistant ‘off’ periods. Neurology 1988; 38: 481–3
Riley D, Lang AE. Practical application of a low-protein diet for Parkinson’s disease. Neurology 1988; 38: 1026–31
Ziegler M, Ranoux D, de Recondo J. Clinical efficacy of a liquid formulation of Levodopa (Madopar Dispersible) in reversing afternoon ‘off’ periods in Parkinson’s disease. Clin Neuropharmacol 1994; 17 (3 Suppl.): 21S–5S
Lhermitte F, Agid Y, Signoret JL. Onset and end-of-dose levodopa-induced dyskinesias. Arch Neurol 1978; 35: 261–3
Mark MH, Sage JI. An analysis of treatment options and outcome in patients with Parkinson’s disease and severe dyskinesias. Ann Clin Lab Sci 1994; 24: 12–21
Paalzow GHM, Paalzow LK. L-dopa: how it may exacerbate parkinsonian symptoms. TIPS 1986; 9: 15–9
Merello M, Lees AJ. Beginning-of-dose motor deterioration following the acute administration of levodopa and apomorphine in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1992; 55: 1024–6
Nutt JG, Gancher ST, Woodward WR. Does an inhibitory action of levodopa contribute to motor fluctuations? Neurology 1988; 38: 1553–7
Contin M, Riva R, Martinelli P, et al. Kinetic-dynamic relationship of oral levodopa: possible biphasic response after sequential doses in Parkinson’s disease. Mov Disord 1992; 7: 244–8
Nutt JG. Levodopa-induced dyskinesia: review, observations, and speculations. Neurology 1990; 40: 340–5
Sage JI, Mark MH, McHale DM, et al. Benefits of monitoring plasma levodopa in Parkinson’s disease patients with drug-induced Chorea. Ann Neurol 1991; 29: 623–8
McHale DM, Sage JI, Sonsalla PK, et al. Complex dystonia of Parkinson’s disease: clinical features and relation to plasma levodopa profile. Clin Neuropharmacol 1990; 13: 164–70
Zimmerman TR, Sage JI, Lang AE, et al. Severe evening dyskinesias in advanced parkinson’s disease: clinical description, relation to plasma levodopa, and treatment. Mov Disord 1994; 9: 173–7
Mouradian MM, Heuser JE, Baronti F, et al. Pathogenesis of dyskinesias in Parkinson’s disease. Ann Neurol 1989; 25: 523–6
Shoulson I, Glaubiger GA, Chase TN. Clinical and biochemical correlations during oral and intravenous levodopa administration in parkinsonian patients. Neurology 1975; 25: 1144–8
Quinn N, Parkes D, Marsden CD. Control of on/off phenomenon by continuous intravenous infusion of levodopa. Neurology 1984; 34: 1131–6
Hardie RJ, Lees AJ, Stern GM. On-off fluctuations in Parkinson’s disease. Brain 1984; 107: 487–506
Kurlan R, Nutt JG, Woodward WR, et al. Duodenal and gastric delivery of levodopa in Parkinsonism. Ann Neurol 1988; 23: 589–95
Sage JI, Schuh L, Heikkila RE, et al. Continuous duodenal infusions of levodopa: plasma concentrations and motor fluctuations in Parkinson’s disease. Clin Neuropharmacol 1988; 11: 36–44
Cedarbaum JM. The promise and limitations of controlled-release oral levodopa administration. Clin Neuropharmacol 1989; 12: 147–66
Dempski RE, Scholtz EC, Oberholtzer ER, et al. Pharmaceutical design and development of a Sinemet controlled-release formulation. Neurology 1989; 39 Suppl. 2; 20–4
Erni W, Held K. The hydrodynamically balanced system: a novel principle of controlled drug release. Eur Neurol 1987; 27 Suppl. 2; 21–7
Yeh KC, August TF, Bush DF, et al. Pharmacokinetics and bio-availability of Sinemet CR: a summary of human studies. Neurology 1989; 39 Suppl. 2; 25–37
LeWitt PA, Nelson MV, Berchou RC, et al. Controlled-release carbidopa/levodopa (Sinemet 50/200 CR4): clinical and pharmacokinetic studies. Neurology 1989; 39 Suppl. 2; 45–53
Crevoisier C, Hoevels B, Zurcher G, et al. Bioavailability of L-dopa after Madopar HBS administration in healthy volunteers. Eur Neurol 1987; 27 Suppl. 1; 36–46
Marion MH, Stocchi F, Malcolm SL, et al. Single-dose studies of a slow-release preparation of levodopa and benserazide (Madopar HBS) in Parkinson’s disease. Eur Neurol 1987; 27 Suppl. 1; 54–8
Hutton JT, Morris JL. Therapeutic advantages of sustained release levodopa formulations in Parkinson’s disease. CNS Drugs 1994; 2: 110–9
Calne DB. Initiating treatment for idiopathic parkinsonism. Neurology 1994; 44 (6 Suppl.): 19S–22S
Goetz CG, Tanner CM, Shannon KM, et al. Controlled-release carbidopa/levodopa (CR4-Sinemet) in Parkinson’s disease patients with and without motor fluctuations. Neurology 1988; 38: 1143–6
Hammerstad JP, Woodward WR, Nutt JG, et al. Controlled release levodopa/carbidopa 25/100 (Sinemet CR 25/100): pharmacokinetics and clinical efficacy in untreated parkinsonian patients. Clin Neuropharmacol 1994; 17: 429–34
Cedarbaum JM, Kutt H, McDowell FH. A pharmacokinetic and pharmacodynamic comparison of Sinemet CR (50/200) and standard Sinemet. Neurology 1989; 39 Suppl. 2; 38–44
Harder S, Baas H, Bergemann N, et al. Concentration-effect relationship of levodopa in patients with Parkinson’s disease after oral administration of an immediate release and a controlled release formulation. Br J Clin Pharmacol 1995; 39: 39–44
Cedarbaum JM, Hoey M, McDowell FH. A double-blind crossover comparison of Sinemet CR4 and standard Sinemet 25/100 in patients with Parkinson’s disease and fluctuating motor performance. J Neurol Neurosurg Psychiatry 1989; 52: 207–12
Malcolm SL, Allen JG, Bird H, et al. Single-dose pharmacokinetics of Madopar HBS in patients and effect of food and antacid of the absorption on Madopar HBS in volunteers. Eur Neurol 1987; 27 Suppl. 1; 28–35
Wilding IR, Hardy JG, Davis SS, et al. Characterisation of the in vivo behaviour of a controlled-release formulation of levodopa (Sinemet CR). Clin Neuropharmacol 1991; 14: 305–21
Deleu D, Jacques M, Michotte Y, et al. Controlled-release carbidopa/levodopa (CR) in parkinsonian patients with response fluctuations on standard levodopa treatment: clinical and pharmacokinetic observations. Neurology 1989; 39 Suppl. 2; 88–92
Rodnitzky RL. The use of Sinemet CR in the management of mild to moderate Parkinson’s disease. Neurology 1992; 42 Suppl. 1; 44–50
Mannisto PT. Clinical potential of catechol-O-methyl-transferase (COMT) inhibitors as adjuvants in Parkinson’s disease. CNS Drugs 1994; 1: 172–9
Kaakkola S, Gordin A, Mannisto PT. General properties and clinical possibilities of new selective inhibitors of catechol O-methyltransferase. Gen Pharmacol 1994; 25: 813–24
Myllyla VV, Sotaniemi KA, Illi A, et al. Effect of entacapone, a COMT inhibitor, on the pharmacokinetics of levodopa and on cardiovascular responses in patients with parkinson’s disease. Eur J Clin Pharmacol 1993; 45: 419–23
Nutt JG, Woodward WR, Beckner RM, et al. Effect of peripheral catechol-O-methyltransferase inhibition on the pharmacokinetics and pharmacodynamics of levodopa in parkinsonian patients. Neurology 1994; 44: 913–9
Kaakkola S, Teravainen H, Ahtila S, et al. Effect of entacapone, a COMT inhibitor, on clinical disability and levodopa metabolism in parkinsonian patients. Neurology 1994; 44: 77–80
Merello M, Lees AJ, Webster R, et al. Effect of entacapone, a peripherally acting catechol-O-methyltransferase inhibitor, on the motor response to acute treatment with levodopa in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 1994; 57: 186–9
Roberts JW, Cora-Locatelli G, Bravi D, et al. Catechol-O-methyltransferase inhibitor tolcapone prolongs levodopa/carbidopa action in parkinsonian patients. Neurology 1994; 44: 2685–8
Limousin P, Pollak P, Pfefen JP, et al. Acute administration of levodopa-benserazide and tolcapone, a COMT inhibitor, in Parkinson’s disease. Clin Neuropharmacol 1995; 18: 258–65
Tohgi H, Abe T, Yamazaki K, et al. Effects of the catechol-O-methyltransferase inhibitor tolcapone in Parkinson’s disease: correlations between concentrations of dopaminergic substances in the plasma and cerebrospinal fluid and clinical improvement. Neurosci Lett 1995; 192: 165–8
Montastruc JL, Rascol O, Senard JM. Current status of dopamine agonists in Parkinson’s disease management. Drugs 1993; 46: 384–93
Wachtel H. Antiparkinsonian dopamine agonists: a review of the pharmacokinetics and neuropharmacology in animals and humans. J Neural Transm Park Dis Dement Sect 1991; 3: 151–201
Schran HF, Bhuta SI, Schwarz HJ, et al. The pharmacokinetics of bromocriptine in man. Adv Biochem Psychopharmacol 1980; 23: 125–39
Drewe J, Mazer N, Abisch E, et al. Differential effect of food on kinetics of bromocriptine in a modified release capsule and a conventional formulation. Eur J Clin Pharmacol 1988; 35: 535–41
Maurer G, Schreier E, Delaborde S, et al. Fate and disposition of bromocriptine in animals and man. Pt II: absorption, elimination and metabolism. Eur J Drug Metab Pharmacokinet 1983; 8: 51–62
Kopitar Z, Vrhovac B, Povsic L, et al. The effect of food and metoclopramide on the pharmacokinetics and side effects of bromocriptine. Eur J Drug Metab Pharmacokinet 1991; 16: 177–81
Ho KY, Thorner MO. Therapeutic applications of bromocriptine in endocrine and neurological diseases. Drugs 1988; 36: 67–82
Ludden TM. Pharmacokinetic interactions of the macrolide antibiotics. Clin Pharmacokinet 1985; 10: 63–79
Nelson MV, Berchou RC, Kareti D, et al. Pharmacokinetic evaluation of erythromycin and caffeine administered with bromocriptine. Clin Pharmacol Ther 1990; 47: 694–7
Parkes JD, Debono AG, Marsden CD. Bromocriptine in Parkinsonism: long-term treatment, dose response, and comparison with levodopa. J Neurol Neurosurg Psychiatry 1976; 39: 1101–8
Teychenne PF, Bergsrud D, Racy A, et al. Bromocriptine: low-dose therapy in Parkinson disease. Neurology 1982; 32: 577–83
Pfeiffer RF, Wilken K, Glaeske C, et al. Low-dose bromocriptine therapy in Parkinson’s disease. Arch Neurol 1985; 42: 586–8
Parkes JD. Domperidone and Parkinson’s disease. Clin Neuropharmacol 1986; 9: 517–32
Agid Y, Pollak P, Bonnet AM, et al. Bromocriptine associated with a peripheral dopamine blocking agent in treatment of Parkinson’s disease. Lancet 1979; I: 570–2
Burns RS, Gopinathan G, Humpel M, et al. Disposition of oral Lisuride in Parkinson’s disease. Clin Pharmacol Ther 1984; 35: 548–56
Humpel M, Nieuweboer B, Hasan SH, et al. Radioimmunoassay of plasma lisuride in man following intravenous and oral administration of lisuride hydrogen maleate; effect on plasma prolactin level. Eur J Clin Pharmacol 1981; 20: 47–51
Rubin A, Lemberger L, Dhahir P. Physiologic disposition of pergolide. Clin Pharmacol Ther 1981; 30: 258–65
Langtry HD, Clissold SP. Pergolide. A review of its pharmacological properties and therapeutic potential in Parkinson’s disease. Drugs 1990; 39: 491–506
Cotzias GC, Papavasiliou PS, Tolosa ES, et al. Treatment of Parkinson’s disease with aporphines. N Engl J Med 1976; 294: 567–72
Gancher ST, Nutt JG, Woodward WR. Absorption of apomorphine by various routes in Parkinsonism. Mov Disord 1991; 6: 212–6
Gancher ST, Woodward WR, Boucher B, et al. Peripheral pharmacokinetics of apomorphine in humans. Ann Neurol 1989; 26: 232–8
Nicolle E, Pollak P, Serre-Debeauvais F, et al. Pharmacokinetics of apomorphine in parkinsonian patients. Fundam Clin Pharmacol 1993; 7: 245–52
Sam E, Jeanjean AP, Maloteaux JM, et al. Apomorphine pharmacokinetics in Parkinsonism after intranasal and subcutaneous application. Eur J Drug Metab Pharmacokinet 1995; 20: 27–33
Kleedorfer B, Turjanski N, Ryan R, et al. Intranasal apomorphine in Parkinson’s disease. Neurology 1991; 41: 761–2
Kapoor R, Turjanski N, Frankel J, et al. Intranasal apomorphine: a new treatment in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1991; 53: y1015
Van Laar T, Jansen ENH, Essink AWG, et al. Intranasal apomorphine in parkinsonian on-off fluctuations. Arch Neurol 1992; 49: 482–4
Hughes AJ, Webster R, Bovingdon M, et al. Sublingual apomorphine in the treatment of Parkinson’s disease complicated by motor fluctuations. Clin Neuropharmacol 1991; 14: 556–61
Durif F, Jeanneau E, Serre-Debeauvais F, et al. Relation between plasma concentration and clinical efficacy after sublingual single dose apomorphine in Parkinson’s disease. Eur J Clin Pharmacol 1991; 41: 493–4
Van Laar T, Jansen ENH, Neef C, et al. Pharmacokinetics and clinical efficacy of rectal apomorphine in patients with Parkinson’s disease: a study of five different suppositories. Mov Disord 1995; 10: 433–9
Frankel JP, Lees AJ, Kempster PA, et al. Subcutaneous apomorphine in the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry 1990; 53: 96–101
Hughes AJ, Bishop S, Kleedorfer B, et al. Subcutaneous apomorphine in Parkinson’s disease: response to chronic administration for up to five years. Mov Disord 1993; 8: 165–70
Muguet D, Broussolle E, Chazot G. Apomorphine in patients with Parkinson’s disease. Biomed Pharmacother 1995; 49: 197–209
Hollmann M, Brode E, Greger G, et al. Biperiden effects and plasma levels in volunteers. Eur J Clin Pharmacol 1984; 27: 619–21
Grimaldi R, Perucca E, Ruberto G, et al. Pharmacokinetic and pharmacodynamic studies following intravenous and oral administration of the antiparkinsonian drug biperiden in normal subjects. Eur J Clin Pharmacol 1986; 30: 735–7
Whiteman PD, Fowle ASE, Hamilton MJ, et al. Pharmacokinetics and pharmacodynamic s of procyclidine in man. Eur J Clin Pharmacol 1985; 28: 73–8
Burke RE, Fahn S. Pharmacokinetics of trihexyphenidyl after short-term and long-term administration to dystonic patients. Ann Neurol 1985; 18:35–40
Garbarg S, Devissaguet JP, Prost M, et al. Comparaison pharmacoclinique de deux formes galeniques de trihexyphenidyle. Encéphale 1983; IX: 167–74
He H, McKay G, Wirshing B, et al. Development and application of a specific and sensitive radioimmunoassay for trihexyphenidyl to a pharmacokinetic study in humans. J Pharm Sci 1995; 84: 561–7
Labout JJM, Thijssen CT, Keijser GGJ, et al. Difference between single and multiple dose pharmacokinetics of orphenadrine hydrochloride in man. Eur J Clin Pharmacol 1982; 21: 343–50
Bast A, van Kemenade FAA, Savenije-Chapel EM, et al. Product inhibition in orphenadrine metabolism as a result of a stable cytochrome P-450-metabolic intermediate complex formed during the disposition of mono-n-desmethyl-orphenadrine (Tofenacine) in the rat. Res Commun Chem Pathol Pharmacol 1983; 40: 391–403
Reidy GF, Mehta I, Murray M. Inhibition of oxidative drug metabolism by orphenadrine: in vitro and in vivo evidence for isozyme-specific complexation of cytochrome P-450 and inhibition kinetics. Mol Pharmacol 1989; 35: 736–43
Birkmayer W, Riederer P, Youdim MBH. Deprenyl in the treatment of Parkinson’s disease. Clin Neuropharmacol 1982; 5: 195–230
Squires RF. Multiple forms of monoamine oxidase in intact mitochondria as characterized by selective inhibitors and thermal stability: a comparison of eight mammalian species. Adv Biochem Psychopharmacol 1972; 5: 355–70
Glover V, Sandier M, Owen F, et al. Dopamine is a monoamine oxidase-B substrate in man. Nature 1977; 265: 80–1
Olanow CW, Calne D. Does selegiline monotherapy in Parkinson’s disease act by symptomatic or protective mechanisms? Neurology 1991; 42 Suppl. 4; 13–26
Heinonen EH, Anttila MI, Lammintausta RAS. Pharmacokinetic aspects of l-deprenyl (selegiline) and its metabolites. Clin Pharmacol Ther 1994; 56: 742–9
Michaelis K, Waitzinger J, Agvaz U, et al. Pharmacokinetics of l-deprenyl and N-desmethyldeprenyl in blood versus plasma after single dose oral administration of 10 mg of selegiline. Pharmacol Res 1993; 10: S331
Yoshida T, Yamada Y, Yamamoto T, et al. Metabolism of deprenyl, a selective monoamine oxidase (MAO) B inhibitor in rat: relationship of metabolism to MAO-B inhibitory potency. Xenobiotica 1986; 16: 129–36
Karoum F, Chuang LW, Eisler T, et al. Metabolism of (−) deprenyl to amphetamine and methamphetamine may be responsible for deprenyl’s therapeutic benefit: a biochemical assessment. Neurology 1982; 32: 503–9
Yasar S, Bergman J. Amphetamine-like effect of l-deprenyl (selegiline) in drug discrimination studies. Clin Pharmacol Ther 1994; 56: 768–73
Golbe LI. Deprenyl as symptomatic therapy in Parkinson’s disease. Clin Neuropharmacol 1988; 11: 387–400
Fowler JS, Volkow ND, Logan J, et al. Slow recovery of human brain MAO B after l-deprenyl (Selegeline) withdrawal. Synapse 1994; 18: 86–93
McGrath PJ, Stewart JW, Quitkin FM. A possible deprenyl induced hypertensive reaction. J Clin Psychopharmacol 1989; 9: 310–1
Suchowersky O, deVries J. Possible interactions between deprenyl and Prozac. Can J Neurol Sci 1990; 17: 352–3
Montastruc JL, Chamontin B, Senard JM, et al. Pseudophaeo-chromocytoma in parkinsonian patient treated with fluoxetine plus selegiline. Lancet 1993; 341: 555
Jermain DM, Hughes PL, Follender AB. Potential fluoxetine-selegiline interaction. Ann Pharmacother 1992; 26: 1300
Sternbach H. The serotonin syndrome. Am J Psychiatry 1991; 148: 705–13
Parkinson Study Group. Effect of deprenyl on the progression of disability in early Parkinson’s disease. N Engl J Med 1989; 321: 1364–71
Tetrud JW, Langston JW. The effect of deprenyl (selegiline) on the natural history of parkinson’s disease. Science 1989; 245: 519–22
Myllyla VV, Sotaniemi KA, Vuorinen JA, et al. Selegiline as initial treatment in de novo parkinsonian patients. Neurology 1992; 42: 339–43
Cedarbaum JM, Silvestri M, Clark M, et al. L-deprenyl, levodopa pharmacokinetics, and response fluctuations in Parkinson’s disease. Clin Neuropharmacol 1990; 13: 29–35
Teychenne PF, Parker S. Double-blind, crossover placebo controlled trial of selegiline in Parkinson’s disease — an interim analysis. Acta Neurol Scand 1989; 126: 119–25
Baronti F, Davis TL, Boldry RC, et al. Deprenyl effects on levodopa pharmacodynamics, mood, and free radical scavenging. Neurology 1992; 42: 541–4
Schachter M, Marsden CD, Parkes JD, et al. Deprenyl in the management of response fluctuations in patients with Parkinson’s disease on levodopa. J Neurol Neurosurg Psychiatry 1980; 43: 1016–21
Brodersen P, Philbert A, Gulliksen G, et al. The effect of L-deprenyl on on-off phenomena in Parkinson’s disease. Acta Neurol Scand 1985; 71: 494–7
Golbe LI, Lieberman AN, Muenter MD, et al. Deprenyl in the treatment of symptom fluctuations in advanced Parkinson’s disease. Clin Neuropharmacol 1988; 11: 45–55
Vezina P, Mohr E, Grimes D. Deprenyl in Parkinson’s disease: mechanisms, neuroprotective effect, indications and adverse effects. Can J Neurol Sci 1992; 19: 142–6
Schwab RS, England Jr AC, Poskanzer DC, et al. Amantadine in the treatment of Parkinson’s disease. JAMA 1969; 208: 1168–70
Greenamyre JT, O’Brien CF. N-Methyl-D-aspartate antagonists in the treatment of Parkinson’s disease. Arch Neurol 1991; 48: 977–81
Aoki FY, Sitar DS. Amantadine kinetics in healthy elderly men: implications for influenza prevention. Clin Pharmacol Ther 1985; 37: 137–44
Horadam VW, Sharp JG, Smilack JD, et al. Pharmacokinetics of amantadine hydrochloride in subjects with normal and impaired renal function. Ann Intern Med 1981; 94: 454–8
Wilson TW, Rajput AH. Amantadine-Dyazide interaction. Can Med AssocJ 1983; 129: 974–5
Somani SK, Degelau J, Cooper SL, et al. Comparison of pharmacokinetic and safety profiles of amantadine 50- and 100-mg daily doses in elderly nursing home residents. Pharmacotherapy 1991; 11: 460–6
Gerlach M, Riederer P, Youdim MBH. Neuroprotective therapeutic strategies. Comparison of experimental and clinical results. Biochem Pharmacol 1995; 50: 1–16
Author information
Authors and Affiliations
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/BF03259706.
Rights and permissions
About this article
Cite this article
Contin, M., Riva, R., Albani, F. et al. Pharmacokinetic Optimisation in the Treatment of Parkinson’s Disease. Clin-Pharmacokinet 30, 463–481 (1996). https://doi.org/10.2165/00003088-199630060-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-199630060-00004