
Induction or adjuvant chemotherapy for radical multimodality therapy
Introduction
The radical treatment of malignant pleural mesothelioma (MPM) with multimodality therapy including radical surgery, chemotherapy and radiotherapy has been associated with prolonged survival outcomes (1,2). The addition of chemotherapy to cancer-directed surgery has been shown to improve survival compared with surgery alone, with an even larger survival benefit with the addition of radiation therapy (3). However, there is limited evidence regarding the long-term survival benefits, particularly in the context of the high morbidity and mortality associated with this type of radical approach to treatment (2,4-17). The majority of these studies are non-randomised and utilize variations of the three modalities, with no standardized approach agreed on internationally. A recent systematic review outlined the lack of evidence regarding the use of multimodality therapy in MPM, with only two randomized trials available for analysis (18-20). Neither trial was powered to detect a difference in clinical outcome and as such conclusions regarding efficacy of multimodality therapy cannot be drawn from them. Radical surgery with either extrapleural pneumonectomy (EPP) or extended pleurectomy decortication (EPD) aims to achieve macroscopic complete resection of the tumour (12,21-23). An R0 resection can rarely be achieved, except possibly in cases of localized mesothelioma tumours or early stage tumours after neoadjuvant therapy, and there is a high risk of local disease progression, therefore systemic therapy is recommended with chemotherapy, and/or radiation therapy alongside radical surgery (24-26).
The combination of cisplatin and pemetrexed is the standard first line chemotherapy treatment in MPM due to the survival advantage over cisplatin alone (27). This survival increase was small but has been the only treatment shown to give a survival benefit, and as such has been included in almost all published multimodality treatment strategies. There have been recent advances in targeted agents and immunotherapy strategies with antibodies against programmed cell death protein 1/programmed cell death ligand 1 (PD1/PDL1) and cytotoxic t-lymphocyte associated protein 4 (CTLA4), yet platinum-pemetrexed remains the only proven systemic therapy for MPM.
The optimal timing of platinum-pemetrexed chemotherapy within the context of multimodality therapy has not yet been established (28). There are proponents of neoadjuvant and of adjuvant therapy with no evidence to strongly support one approach above the other with radical surgery (4-6,8-11,29-31). As yet there have been no published trials comparing the two, although several phase 2 studies have shown that chemotherapy as a part of multimodality therapy is safe and may be beneficial (11,32-35). Following this chemotherapy treatment there are limited systemic treatment options outside clinical trials. There is therefore also a rationale for reserving this chemotherapy option following maximal debulking with radical surgery until there is evidence of disease progression (28).
Neoadjuvant chemotherapy
Neoadjuvant chemotherapy is often utilized as part of multimodality treatment, particularly in the context of EPP and adjuvant hemithoracic radiotherapy. A standardized regimen using platinum-pemetrexed doublet has been shown to be feasible in these patients (2,6,8-11,29). Although the studies investigating the use of neoadjuvant chemotherapy have usually reported good median overall survival outcomes of between 16.8–25.5 months, the efficacy of this approach has not been proven and these studies are fraught with issues such as failure to complete all modes of treatment and no intention to treat analyses. High levels of patient fitness are required to undergo this type of regime and it may be that the relatively good survival outcomes are a consequence of patient selection.
There are several rationales for giving neoadjuvant therapy as opposed to adjuvant therapy in the context of radical surgery. In other tumour types, neoadjuvant therapy is usually utilized to downstage a tumour, in order to render patients operable or allow for more easily tolerated surgical approaches to be pursued, or to improve prognosis directly through reduction of micrometastatic disease prior to surgery. Downstaging by reduction of the tumour bulk may play a part in the efficacy of neoadjuvant chemotherapy in MPM (5,11). However, it does not give a quantifiable technical advantage at operation. A complete pathological response to chemotherapy is rare, with studies showing a response rate of 29–67%, and has not been shown to give a long-term benefit to overall or progression free survival (27,29,36,37). Distant spread is uncommon in MPM with disease progression following surgical resection usually occurring in the ipsilateral hemithorax (38-41). This may suggest that micrometastatic disease is of lower importance in MPM than in other tumour types, thus negating this particular perceived benefit of systemic neoadjuvant treatment.
Many believe that chemotherapy is better tolerated in the neoadjuvant setting due to the morbidity associated with radical surgery, and therefore more cycles can be given (4-6,8,9,11,29). However, the standard approach in MPM is usually to give three or four cycles of neoadjuvant therapy compared with six after surgery so as to not delay surgical resection (35,42-44). Particularly with the increasing use of EPD, the number tolerated post-operatively has been shown to exceed that given as induction therapy in some cases (28). It may be true that the chemotherapy better reaches the tumour pre-operatively due to the intact blood supply but this has not been proven.
Possibly the most important factor in the good results seen following neoadjuvant chemotherapy is patient selection. Disease progression during chemotherapy can render patients unresectable and therefore will select out those patients with tumours which have a more aggressive phenotype. It also selects out patients who are unable to tolerate chemotherapy and who would also most likely have a poorer outcome in terms of morbidity and mortality from radical surgery. This leads to a fitter cohort of patients undergoing radical resection after neoadjuvant chemotherapy, who may have a better prognosis biological phenotype. There is another theory that has been put forward against neoadjuvant chemotherapy in that in the context of intratumour heterogeneity, chemo-sensitive cells will be killed pre-operatively, leaving a smaller bulk of tumour but which may comprise of a population of more aggressive chemo-resistant cells (45,46). This could explain the rapid tumour progression that is sometimes seen in patients following radical surgery and neoadjuvant chemotherapy.
For these reasons any future trials of neoadjuvant chemotherapy must include an intention to treat analysis and not simply report outcomes of those who underwent the entire trial protocol. The attrition from these trials skew the results, and the patient selection bias inherent in retrospective studies make it difficult to determine the true benefit, or harm, of neoadjuvant chemotherapy.
Adjuvant chemotherapy
There is currently limited evidence in support of adjuvant chemotherapy following radical surgery for MPM. Many of the previous trials of multimodality therapy have used the protocol of neoadjuvant chemotherapy, radical surgery (EPP in the main) and adjuvant hemithoracic radiotherapy as previously discussed. True adjuvant chemotherapy is chemotherapy commenced within 3 months of operation.
There is evidence from the International Association for the Study of Lung Cancer (IASLC) staging committee project that the provision of adjuvant therapy is an independent prognostic factor for survival from MPM (47). With the increasing use of EPD rather than EPP, hemithoracic radiation is less commonly used and more centres are moving to upfront radical surgery followed by chemotherapy. Following EPP many patients are not able to tolerate chemotherapy in the immediate adjuvant period, however with this increasing use of EPD, post-operative recovery is faster and most patients are able to commence chemotherapy within 8 weeks of surgery (17,28,30,48). One retrospective study found that survival of patients who underwent radical surgery plus adjuvant chemotherapy had a significant survival over those who received chemotherapy alone (19.8 vs. 11.7 months) and that the receipt of chemotherapy was an independent prognostic factor for survival (49). However, given that there is only one proven line of chemotherapy available, some oncologists advocate reserving this until there is evidence of disease progression as there will otherwise be limited therapeutic options on relapse (27). There is also an argument for reserving the use of platinum-pemetrexed as many of the clinical trial protocols of novel therapies include these agents, and there is the possibility that previous treatment may lead to trial exclusion.
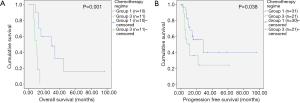
There may be a benefit to giving “true” adjuvant chemotherapy over reserving it until progression in patients who have non-epithelioid disease and/or pathological nodal disease (28) (Figure 1). These patients have poor prognosis tumours in the first instance and are most likely to develop progression relatively quickly. In patients with N1 disease [8th TNM staging system, N2 disease if referring to the 7th TNM staging system (50)] who undergo radical surgery, their survival is similar to those who have chemotherapy treatment alone so additional systemic therapy is required and the new ASCO guidelines mandate that that be neoadjuvant chemotherapy in cases of histologically proven N1 disease (26,27). It follows that in unsuspected N1 disease found at operation, then adjuvant chemotherapy would be required.
If adjuvant chemotherapy is planned, it must be ensured that the patient is likely to be fit enough to undergo this treatment following radical surgery. If they are thought to be of borderline fitness for surgery, with poor ECOG performance status for example, it may be more appropriate for them to undergo neoadjuvant chemotherapy given that their fitness will be worsened in the immediate post-operative setting regardless of the operation type, EPP or EPD (23,28).
The “EORTC Randomized Phase II Study of Pleurectomy/Decortication (P/D) Preceded or Followed by Chemotherapy in Patients With Early Stage Malignant Pleural Mesothelioma” trial is currently ongoing (NCT02436733). It aims to evaluate the optimum timing of chemotherapy as part of multimodality therapy for MPM by comparing pleurectomy/decortication either preceded by three cycles of cisplatin-pemetrexed chemotherapy, or followed by three cycles of cisplatin-pemetrexed. The study is due to close in 2020 and will hopefully shed light on the ideal timing of chemotherapy treatment.
Alternative administrations of chemotherapy
The most common site of progression following radical surgery for MPM is in the ipsilateral hemithorax, and with the relatively high local progression rate, the use of intrapleural therapies have become more prevalent (24,38,39,51). These have mainly used platinum-based heated chemotherapy or photodynamic therapy (PDT). The objective of radical surgery, either by EPP or EPD, is to achieve complete macroscopic resection, and by definition cannot achieve an R0 resection. Thus, intracavitary therapies have been introduced to improve the effect of local resection.
The combination of heat, intracavitary perfusion is usually at 42 °C, along with a chemotherapeutic agent results in increased cell membrane permeability, having a direct cytotoxic effect on tumour cells (52). The heat increases the cytotoxicity of particular chemotherapy agents, and can increase the drug penetration into tissues in a temperature-dependent way (53-57). Intraoperative instillation of platinum-based chemotherapy into the chest has been shown to be safe in selected experienced institutions, and can lead to favourable median overall and progression free survival outcomes (15,58-60). The optimum dose has not yet been established, with varying protocols between studies (61,62). One study showed an increase in time to progression from 12.8 to 27.1 months, and overall survival from 22.8 to 35.5 months in clinically matched patients receiving hyperthermic intrapleural chemotherapy (63). This route of administration requires further evaluation in a randomised trial setting, and although published results look promising, the institutional requirements and prolongation of operation times may preclude its uptake in many centres.
The use of intraoperative PDT following surgery for MPM has been investigated in a few small phase I and II trials, and observational studies (64-66). A photosensitizing agent is administered to the patient, usually Photofrin (porfimer sodium) or Foscam (meta-tetra hydroxylphenyl chlorin). A light source with a specific wavelength is then placed into the pleura following resection. When the light source is activated, the oxygen present becomes a more reactive form known as “singlet oxygen”. This causes cell membrane damage and triggers a cytotoxic immune response. Overall survival of up to 32 months has been reported, although the levels of local progression, effectively local treatment failure, have been high. One randomized control trial of PDT following radical surgery showed there to be no benefit to adding PDT to the normal multimodality radical treatment of MPM (67). A recent publication has shown a 36-month overall survival following EPD and intraoperative PDT, with adjuvant chemotherapy. This survival increased to 88 months in pathological node negative patients (68). The future of multimodality therapy for MPM may involve the use of an intraoperative therapy alongside radical resection and either neoadjuvant or adjuvant therapy, but this requires further randomized trial investigation, and improved methods of utilization.
ASCO guidelines 2018
Evidence based guidelines regarding the management of MPM have recently been published by an expert panel within the American Society of Clinical Oncology (ASCO) (26). They have produced recommendations spanning diagnostics, staging and treatment options. Several recommendations were made regarding the use of chemotherapy as part of radical treatment alongside radical surgery as outlined below.
- Maximal surgical cytoreduction as a single modality treatment is generally insufficient; additional antineoplastic treatment (chemotherapy and/or radiation therapy) should be administered;
- Since surgical cytoreduction is not expected to yield an R0 resection, it is strongly recommended that multimodality therapy with chemotherapy and/or radiation therapy should be administered;
- Chemotherapy may be given pre- or postoperatively in the context of multimodality treatment;
- In the context of multimodality treatment, four to six cycles of pemetrexed/platin-based chemotherapy may be administered pre- or postoperatively;
- Patients with transdiaphragmatic disease, multifocal chest wall invasion, or histologically confirmed contralateral mediastinal or supraclavicular lymph node involvement should undergo neoadjuvant treatment before consideration of maximal surgical cytoreduction;
- Patients with ipsilateral, histologically confirmed mediastinal lymph node involvement should only undergo maximal surgical cytoreduction in the context of multimodality therapy (neoadjuvant or adjuvant chemotherapy).
Conclusions
At present there is no consensus regarding the timing of chemotherapy as part of multimodality therapy for MPM (28). It is widely accepted that chemotherapy should be given alongside surgery with radical intent, although further research is required in order to determine the optimum strategy for multimodality treatment of MPM.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Shanghai Chest for the series “Mesothelioma Surgery”. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.06.06). The series “Mesothelioma Surgeryy” was commissioned by the editorial office without any funding or sponsorship. AJS served as the unpaid Guest Editor of the series. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rusch VW, Giroux D, Kennedy C, et al. Initial analysis of the international association for the study of lung cancer mesothelioma database. J Thorac Oncol 2012;7:1631-9. [Crossref] [PubMed]
- Cao C, Tian D, Manganas C, et al. Systematic review of trimodality therapy for patients with malignant pleural mesothelioma. Ann Cardiothorac Surg 2012;1:428-37. [PubMed]
- Nelson DB, Rice DC, Niu J, et al. Long-term survival outcomes of cancer-directed surgery for malignant pleural mesothelioma: Propensity score matching analysis. J Clin Oncol 2017;35:3354-62. [Crossref] [PubMed]
- Buduhan G, Menon S, Aye R, et al. Trimodality therapy for malignant pleural mesothelioma. Ann Thorac Surg 2009;88:870-875; discussion 876. [Crossref] [PubMed]
- de Perrot M, Feld R, Cho BC, et al. Trimodality therapy with induction chemotherapy followed by extrapleural pneumonectomy and adjuvant high-dose hemithoracic radiation for malignant pleural mesothelioma. J Clin Oncol 2009;27:1413-8. [Crossref] [PubMed]
- Flores RM, Krug LM, Rosenzweig KE, et al. Induction chemotherapy, extrapleural pneumonectomy, and postoperative high-dose radiotherapy for locally advanced malignant pleural mesothelioma: a phase II trial. J Thorac Oncol 2006;1:289-95. [Crossref] [PubMed]
- Pagan V, Ceron L, Paccagnella A, et al. 5-year prospective results of trimodality treatment for malignant pleural mesothelioma. J Cardiovasc Surg (Torino) 2006;47:595-601. [PubMed]
- Rea F, Marulli G, Bortolotti L, et al. Induction chemotherapy, extrapleural pneumonectomy (EPP) and adjuvant hemi-thoracic radiation in malignant pleural mesothelioma (MPM): Feasibility and results. Lung Cancer 2007;57:89-95. [Crossref] [PubMed]
- Van Schil PE, Baas P, Gaafar R, et al. Trimodality therapy for malignant pleural mesothelioma: Results from an EORTC phase II multicentre trial. Eur Respir J 2010;36:1362-9. [Crossref] [PubMed]
- Weder W, Kestenholz P, Taverna C, et al. Neoadjuvant chemotherapy followed by extrapleural pneumonectomy in malignant pleural mesothelioma. J Clin Oncol 2004;22:3451-7. [Crossref] [PubMed]
- Weder W, Stahel RA, Bernhard J, et al. Multicenter trial of neo-adjuvant chemotherapy followed by extrapleural pneumonectomy in malignant pleural mesothelioma. Ann Oncol 2007;18:1196-202. [Crossref] [PubMed]
- Sugarbaker DJ, Flores RM, Jaklitsch MT, et al. Resection margins, extrapleural nodal status, and cell type determine postoperative long-term survival in trimodality therapy of malignant pleural mesothelioma: Results in 183 patients. J Thorac Cardiovasc Surg 1999;117:54-63; discussion 63-5. [Crossref] [PubMed]
- Rice DC, Stevens CW, Correa AM, et al. Outcomes After Extrapleural Pneumonectomy and Intensity-Modulated Radiation Therapy for Malignant Pleural Mesothelioma. Ann Thorac Surg 2007;84:1685-92; discussion 1692-3.
- Flores RM, Pass HI, Seshan VE, et al. Extrapleural pneumonectomy versus pleurectomy/decortication in the surgical management of malignant pleural mesothelioma: Results in 663 patients. J Thorac Cardiovasc Surg 2008;135:620-6, 626.e1-3.
- Tilleman TR, Richards WG, Zellos L, et al. Extrapleural pneumonectomy followed by intracavitary intraoperative hyperthermic cisplatin with pharmacologic cytoprotection for treatment of malignant pleural mesothelioma: A phase II prospective study. J Thorac Cardiovasc Surg 2009;138:405-11. [Crossref] [PubMed]
- Lucchi M, Chella A, Melfi F, et al. Four-modality therapy in malignant pleural mesothelioma: a phase II study. J Thorac Oncol 2007;2:237-42. [Crossref] [PubMed]
- Lang-Lazdunski L, Bille A, Lal R, et al. Pleurectomy/Decortication is Superior to Extrapleural Pneumonectomy in the Multimodality Management of Patients with Malignant Pleural Mesothelioma. J Thorac Oncol 2012;7:737-43. [Crossref] [PubMed]
- Treasure T, Lang-Lazdunski L, Waller D, et al. Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol 2011;12:763-72. [Crossref] [PubMed]
- Stahel RA, Riesterer O, Xyrafas A, et al. Neoadjuvant chemotherapy and extrapleural pneumonectomy of malignant pleural mesothelioma with or without hemithoracic radiotherapy (SAKK 17/04): A randomised, international, multicentre phase 2 trial. Lancet Oncol 2015;16:1651-8. [Crossref] [PubMed]
- Abdel-Rahman O, Elsayed Z, Mohamed H, et al. Radical multimodality therapy for malignant pleural mesothelioma. Cochrane Database Syst Rev 2018;1:CD012605 [PubMed]
- Rice D, Rusch V, Pass H. Recommendations for uniform definitions of surgical techniques for malignant pleural mesothelioma: a consensus report of the International Association for the Study of Lung Cancer International Staging Committee and the International Mesothelioma Interest. J Thorac Oncol 2011;6:1304-12. [Crossref] [PubMed]
- Sugarbaker DJ, Jaklitsch MT, Bueno R, et al. Prevention, early detection, and management of complications after 328 consecutive extrapleural pneumonectomies. J Thorac Cardiovasc Surg 2004;128:138-46. [Crossref] [PubMed]
- Sharkey AJ, Tenconi S, Nakas A, et al. The effects of an intentional transition from extrapleural pneumonectomy to extended pleurectomy/decortication. Eur J Cardiothorac Surg 2016;49:1632-41. [Crossref] [PubMed]
- Nakas A, von Meyenfeldt E, Lau K, et al. Long-term survival after lung-sparing total pleurectomy for locally advanced (international mesothelioma interest group stage T3-T4) non-sarcomatoid malignant pleural mesothelioma. Eur J Cardiothorac Surg 2012;41:1031-6. [Crossref] [PubMed]
- Baas P, Fennell D, Kerr KM, et al. Malignant pleural mesothelioma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26:v31-9. [Crossref] [PubMed]
- Kindler HL, Ismaila N, Armato SG, et al. Treatment of Malignant Pleural Mesothelioma: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2018;36:1343-73. [Crossref] [PubMed]
- Vogelzang NJ, Rusthoven JJ, Symanowski J, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol 2003;21:2636-44. [Crossref] [PubMed]
- Sharkey AJ, O’Byrne KJ, Nakas A, et al. How does the Timing of Chemotherapy Affect Outcome Following Radical Surgery for Malignant Pleural Mesothelioma? Lung Cancer 2016;100:5-13. [Crossref] [PubMed]
- Krug LM, Pass HI, Rusch VW, et al. Multicenter phase II trial of neoadjuvant pemetrexed plus cisplatin followed by extrapleural pneumonectomy and radiation for malignant pleural mesothelioma. J Clin Oncol 2009;27:3007-13. [Crossref] [PubMed]
- Bölükbas S, Manegold C, Eberlein M, et al. Survival after trimodality therapy for malignant pleural mesothelioma: Radical Pleurectomy, chemotherapy with Cisplatin/Pemetrexed and radiotherapy. Lung Cancer 2011;71:75-81. [Crossref] [PubMed]
- Maggi G, Casadio C, Cianci R, et al. Trimodality management of malignant pleural mesothelioma. Eur J Cardiothorac Surg 2001;19:346-50. [Crossref] [PubMed]
- Rimner A, Zauderer MG, Gomez DR, et al. Phase II study of hemithoracic intensity-modulated pleural radiation therapy (IMPRINT) as part of lung-sparing multimodality therapy in patients with malignant pleural mesothelioma. J Clin Oncol 2016;34:2761-8. [Crossref] [PubMed]
- Krug LM, Kindler HL, Calvert H, et al. Vorinostat in patients with advanced malignant pleural mesothelioma who have progressed on previous chemotherapy (VANTAGE-014): A phase 3, double-blind, randomised, placebo-controlled trial. Lancet Oncol 2015;16:447-56. [Crossref] [PubMed]
- Lindenmann J, Matzi V, Neuboeck N, et al. Multimodal therapy of malignant pleural mesothelioma: Is the replacement of radical surgery imminent? Interact Cardiovasc Thorac Surg 2013;16:237-43. [Crossref] [PubMed]
- Weder W, Opitz I, Stahel R. Multimodality Strategies in Malignant Pleural Mesothelioma. Semin Thorac Cardiovasc Surg 2009;21:172-6. [Crossref] [PubMed]
- Donahoe L, Cho J, De Perrot M. Novel Induction Therapies for Pleural Mesothelioma. Semin Thorac Cardiovasc Surg 2014;26:192-200. [Crossref] [PubMed]
- Opitz I, Weder W. Induction Therapy for Mesothelioma. Semin Thorac Cardiovasc Surg 2015;27:240-9. [Crossref] [PubMed]
- Baldini EH, Recht A, Strauss GM, et al. Patterns of failure after trimodality therapy for malignant pleural mesothelioma. Ann Thorac Surg 1997;63:334-8. [PubMed]
- Jänne PA, Baldini EH. Patterns of failure following surgical resection for malignant pleural mesothelioma. Thorac Surg Clin 2004;14:567-73. [Crossref] [PubMed]
- Baldini EH, Richards WG, Gill R, et al. Updated patterns of failure after multimodality therapy for malignant pleural mesothelioma. J Thorac Cardiovasc Surg 2015;149:1374-81. [Crossref] [PubMed]
- Okubo K, Sonobe M, Fujinaga T, et al. Survival and relapse pattern after trimodality therapy for malignant pleural mesothelioma. Gen Thorac Cardiovasc Surg 2009;57:585-90. [Crossref] [PubMed]
- Weder W, Opitz I. Multimodality therapy for malignant pleural mesothelioma. Ann Cardiothorac Surg 2012;1:502-7. [PubMed]
- Hasegawa S, Okada M, Tanaka F, et al. Trimodality strategy for treating malignant pleural mesothelioma: results of a feasibility study of induction pemetrexed plus cisplatin followed by extrapleural pneumonectomy and postoperative hemithoracic radiation (Japan Mesothelioma Interest Group 0601. Int J Clin Oncol 2016;21:523-30. [Crossref] [PubMed]
- Colaut F, Toniolo L, Vicario G, et al. Pleurectomy/decortication plus chemotherapy: outcomes of 40 cases of malignant pleural mesothelioma. Chir Ital 2004;56:781-6. [PubMed]
- Gerlinger M, Rowan AJ, Horswell S, et al. Intratumor Heterogeneity and Branched Evolution Revealed by Multiregion Sequencing. N Engl J Med 2012;366:883-92. [Crossref] [PubMed]
- Burrell RA, McGranahan N, Bartek J, et al. The causes and consequences of genetic heterogeneity in cancer evolution. Nature 2013;501:338-45. [Crossref] [PubMed]
- Pass HI, Giroux D, Kennedy C, et al. Supplementary Prognostic Variables for Pleural Mesothelioma: A Report from the IASLC Staging Committee. J Thorac Oncol 2014;9:856-64. [Crossref] [PubMed]
- Lang-Lazdunski L, Bille A, Belcher E, et al. Pleurectomy/Decortication, hyperthermic pleural lavage with povidone-iodine followed by adjuvant chemotherapy in patients with malignant pleural mesothelioma. J Thorac Oncol 2011;6:1746-52. [Crossref] [PubMed]
- Bovolato P, Casadio C, Billè A, et al. Does surgery improve survival of patients with malignant pleural mesothelioma?: A multicenter retrospective analysis of 1365 consecutive patients. J Thorac Oncol 2014;9:390-6. [Crossref] [PubMed]
- Rice D, Chansky K, Nowak A, et al. The IASLC Mesothelioma Staging Project: Proposals for Revisions of the N Descriptors in the Forthcoming Eighth Edition of the TNM Classification for Pleural Mesothelioma. J Thorac Oncol 2016;11:2100-11.
- Sharkey AJ, Bilancia R, Tenconi S, et al. The management of the diaphragm during radical surgery for malignant pleural mesothelioma. Eur J Cardiothorac Surg 2016;50:311-6. [Crossref] [PubMed]
- Zhou H, Wu W, Tang X, et al. Effect of hyperthermic intrathoracic chemotherapy (HITHOC) on the malignant pleural effusion: A systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e5532 [Crossref] [PubMed]
- Sugarbaker PH. Laboratory and clinical basis for hyperthermia as a component of intracavitary chemotherapy. Int J Hyperthermia 2007;23:431-42. [Crossref] [PubMed]
- Cavaliere R, Ciocatto EC, Giovanella BC, et al. Selective heat sensitivity of cancer cells. Biochemical and clinical studies. Cancer 1967;20:1351-81. [Crossref] [PubMed]
- Sticca RP, Dach BW. Rationale for hyperthermia with intraoperative intraperitoneal chemotherapy agents. Surg Oncol Clin N Am 2003;12:689-701. [Crossref] [PubMed]
- Overgaard J. Effect of hyperthermia on malignant cells in vivo: A review and a hypothesis. Cancer 1977;39:2637-46. [Crossref] [PubMed]
- Richards WG, Zellos L, Bueno R, et al. Phase I to II study of pleurectomy/decortication and intraoperative intracavitary hyperthermic cisplatin lavage for mesothelioma. J Clin Oncol 2006;24:1561-7. [Crossref] [PubMed]
- Ried M, Potzger T, Braune N, et al. Cytoreductive surgery and hyperthermic intrathoracic chemotherapy perfusion for malignant pleural tumours: Perioperative management and clinical experience. Eur J Cardiothorac Surg 2013;43:801-7. [Crossref] [PubMed]
- Migliore M, Calvo D, Criscione A, et al. Cytoreductive surgery and hyperthermic intrapleural chemotherapy for malignant pleural diseases: preliminary experience. Future Oncol 2015;11:47-52. [Crossref] [PubMed]
- Levchenko EV, Mamontov OI, Senchik KI, et al. Hyperthermic chemoperfusion of the pleural cavity in the combined treatment for malignant pleural mesothelioma. Vopr Onkol 2014;60:482-5. [PubMed]
- Gomez D, Tsao AS. Local and Systemic Therapies for Malignant Pleural Mesothelioma. Curr Treat Options Oncol 2014;15:683-99. [Crossref] [PubMed]
- Bertoglio P, Ambrogi MC, Chella A, et al. Is less also better? A single-institution experience on treatment of early stage Malignant Pleural Mesothelioma. Eur J Surg Oncol 2017;43:1365-71. [Crossref] [PubMed]
- Sugarbaker DJ, Gill RR, Yeap BY, et al. Hyperthermic intraoperative pleural cisplatin chemotherapy extends interval to recurrence and survival among low-risk patients with malignant pleural mesothelioma undergoing surgical macroscopic complete resection. J Thorac Cardiovasc Surg 2013;145:955-63. [Crossref] [PubMed]
- Friedberg JS, Culligan MJ, Mick R, et al. Radical Pleurectomy and Intraoperative Photodynamic Therapy for Malignant Pleural Mesothelioma. Ann Thorac Surg 2012;93:1658-65; discussion 1665-7.
- Friedberg JS, Mick R, Stevenson J, et al. A phase I study of Foscan-mediated photodynamic therapy and surgery in patients with mesothelioma. Ann Thorac Surg 2003;75:952-9. [Crossref] [PubMed]
- Schouwink H, Rutgers ET, Van der Sijp J, et al. Intraoperative photodynamic therapy after pleuropneumonectomy in patients with malignant pleural mesothelioma: Dose finding and toxicity results. Chest 2001;120:1167-74. [Crossref] [PubMed]
- Pass HI, Temeck BK, Kranda K, et al. Phase III randomized trial of surgery with or without intraoperative photodynamic therapy and postoperative immunochemotherapy for malignant pleural mesothelioma. Ann Surg Oncol 1997;4:628-33. [Crossref] [PubMed]
- Friedberg JS, Simone CB, Culligan MJ, et al. Extended Pleurectomy-Decortication-Based Treatment for Advanced Stage Epithelial Mesothelioma Yielding a Median Survival of Nearly Three Years. Ann Thorac Surg 2017;103:912-9. [Crossref] [PubMed]
Cite this article as: Sharkey AJ. Induction or adjuvant chemotherapy for radical multimodality therapy. Shanghai Chest 2018;2:53.


