Abstract
Background
Pancreatic ductal adenocarcinoma (PDAC) has the worst survival of common cancers, partly because there are no reliable early detection tests. Unintentional weight loss (≥ 5% decrease from baseline) has been linked to PDAC, but the frequency and severity of weight loss using objective measures, and its relationship to prognosis, have not been well characterized.
Methods
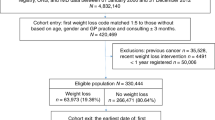
We identified 390 patients with PDAC (all stages) and two or more prediagnosis weights in the electronic medical record. Percentage weight loss in the 365 and 180 days preceding diagnosis was calculated. Results were compared with raw weights of age- and sex-matched non-cancer controls (n = 780). Odds ratios for PDAC were calculated using conditional logistic regression. Cox proportional hazards models were used for survival.
Results
Within 1 year of diagnosis, more PDAC patients lost ≥ 5% weight relative to controls (74.9% vs. 11.2%; p < 0.001), with a median weight loss of 14.2 versus 2.9 lbs. The odds ratio for PDAC comparing weight loss within 1 year of 5 to < 10% was 10.30 (p < 0.001) and 77.82 for ≥ 10% (p < 0.001), compared with stable weight. Weight loss prior to diagnosis was also associated with early-stage PDAC. PDAC cases with ≥ 10% prediagnosis weight loss had worse survival compared with stable weights (hazard ratio [HR] 1.60; p = 0.01). Greater prediagnosis weight loss was associated with poor survival after pancreatectomy (5 to < 10% vs. < 5%, HR 2.40, p = 0.03; ≥ 10% vs. < 5%, HR 2.59, p = 0.03).
Conclusions
Diagnosis of PDAC is preceded by unintentional weight loss in the majority of patients, even at an early stage. Greater prediagnosis weight loss severity is also associated with poor postoperative survival.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Paniccia A, Hosokawa P, Henderson W, et al. Characteristics of 10-T survivors of pancreatic ductal adenocarcinoma. JAMA Surg. 2015;150(8):701–10.
Conroy T, Hammel P, Hebbar M, et al. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med. 2018;379:2395–406.
Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817–25.
Lee J-S, Park SS, Lee YK, Norton JA, Jeffrey SS. Liquid biopsy in pancreatic ductal adenocarcinoma: current status of circulating tumor cells and circulating tumor DNA. Mol Oncol. 2019;13(8):1623–50.
Kaissis G, Braren R. Pancreatic cancer detection and characterization-state of the art cross-sectional imaging and imaging data analysis. Transl Gastroenterol Hepatol. 2019;4:35.
Liu F, Le W, Mei T, et al. In vitro and in vivo targeting imaging of pancreatic cancer using a Fe3O4-SiO2 nanoprobe modified with anti-mesothelin antibody. Int J Nanomed. 2016;11:2195–207.
Wong CJ. Involuntary weight loss. Med Clin N Am. 2014;98(3):625–43.
Marton KI, Sox HC Jr, Krupp J. Involuntary weight loss: diagnostic and prognostic significance. Ann Intern Med. 1981;95(5):568–74.
Rabinovitz M, Pitlik SD, Leifer M, Garty M, Rosenfeld JB. Unintentional weight loss: a retrospective analysis of 154 cases. Arch Intern Med. 1986;146(1):186–7.
Thompson MP, Morris LK. Unexplained weight loss in the ambulatory elderly. J Am Geriatr Soc. 1991;39(5):497–500.
Lankisch PG, Gerzmann M, Gerzmann JF, Lehnick D. Unintentional weight loss: diagnosis and prognosis. The first prospective follow-up study from a secondary referral centre. J Intern Med. 2001;249(1):41–6.
Bilbao-Garay J, Barba R, Losa-García JE, et al. Assessing clinical probability of organic disease in patients with involuntary weight loss: a simple score. Eur J Intern Med. 2002;13(4):240–5.
Metalidis C, Knockaert DC, Bobbaers H, Vanderschueren S. Involuntary weight loss. Does a negative baseline evaluation provide adequate reassurance? Eur J Intern Med. 2008;19(5):345–9.
Wu JM, Lin MH, Peng LN, Chen LK, Hwang SJ. Evaluating diagnostic strategy of older patients with unexplained unintentional body weight loss: a hospital-based study. Arch Gerontol Geriatr. 2011;53(1):e51-54.
Chen SP, Peng LN, Lin MH, Lai HY, Hwang SJ, Chen LK. Evaluating probability of cancer among older people with unexplained, unintentional weight loss. Arch Gerontol Geriatr. 2010;50:s27-29.
Dewys WD, Begg C, Lavin PT, et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med. 1980;69(4):491–7.
Tan BHL, Fearon KCH. Cachexia: prevalence and impact in medicine. Curr Opin Clin Nutr Metab Care. 2008;11(4):400–7.
Aoyagi T, Teerracina KP, Raza A, Matsubara H, Takabe K. Cancer cachexia, mechanism, and treatment. World J Gastrointest Oncol. 2015;7(4):17–29.
Hendifar AE, Chang JI, Huang BZ, Tuli R, Wu BU. Cachexia, and not obesity, prior to pancreatic cancer diagnosis worsens survival and is negated by chemotherapy. J Gastrointest Oncol. 2018;9(1):17–23.
Nemer L, Krishna SG, Shah ZK, et al. Predictors of pancreatic cancer-associated weight loss and nutritional interventions. Pancreas. 2017;46(9):1152–7.
Pausch T, Hartwig W, Hinz U, et al. Cachexia but not obesity worsens the postoperative outcome after pancreatoduodenectomy in pancreatic cancer. Surgery. 2012;152(3 Suppl 1):S81–8.
Peixoto RDA, Speers C, Mcgahan CE, Renouf DJ, Schaeffer DF, Kennecke HF. Prognostic factors and sites of metastasis in unresectable locally advanced pancreatic cancer. Cancer Med. 2015;4(8):1171–7.
Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006;10(9):1191–9.
Yuan C, Babic A, Khalaf N, et al. Diabetes, weight change, and pancreatic cancer risk. JAMA Oncol. 2020;6(10):e202948.
Hendifar AE, Petzel MQB, Zimmers TA, et al. Pancreas cancer-associated weight loss. Oncologist. 2019;24(5):691–701.
Holly EA, Chaliha I, Bracci PM, Gautam M. Signs and symptoms of pancreatic cancer: a population-based case-control study in the San Francisco Bay area. Clin Gastroenterol Hepatol. 2004;2(6):510–7.
Danai LV, Babic A, Rosenthal MH, et al. Altered exocrine function can drive adipose wasting in early pancreatic cancer. Nature. 2018;558:600–4.
Wigmore SJ, Plester CE, Richardson RA, Fearon KCH. Changes in nutritional status associated with unresectable pancreatic cancer. Br J Cancer. 1997;75(1):106–9.
Furukawa H, Iwata R, Moriyama N. Growth rate of pancreatic adenocarcinoma: initial clinical experience. Pancreas. 2001;22(4):366–9.
Kay K, Dolcy K, Bies R, Shah DK. Estimation of solid tumor doubling times from progression-free survival plots using a novel statistical approach. AAPS J. 2019;21(2):27.
Yu J, Blackford AL, Dal Molin M, Wolfgang CL, Goggins M. Time to progression of pancreatic ductal adenocarcinoma from low-to-high tumour stages. Gut. 2015;64:1783–9.
Yachida S, Jones S, Bozic I, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 2010;467(7319):1114–7.
Kindler HL, Niedzwiecki D, Hollis D, et al. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the Cancer and Leukemia Group B (CALGB 80303). J Clin Oncol. 2010;28(22):3617–22.
Philippidis A. 10 Liquid biopsy companies in the money. Clinical Omics. https://www.clinicalomics.com/topics/oncology/10-liquid-biopsy-companies-in-the-money/. Accessed 12 May 2020.
Grail. https://grail.com. Accessed 11 June 2020.
Freenome. https://www.freenome.com. Accessed 11 June 2020.
Guardant. https://guardanthealth.com. Accessed 11 June 2020.
Thirve. Earlier detection. https://thrivedetect.com. Accessed 11 June 2020.
Rey CM. Betting on blood: liquid biopsy companies pursuing both early- and late-stage cancer detection. Clin Omics. 2019;6(3):10–2.
Madhusoodanan J. Firms aim to develop liquid biopsies for early cancer detection. Chem Eng News. 2019;97(47).https://cen.acs.org/analytical-chemistry/diagnostics/Firms-aim-develop-liquid-biopsies/97/i47). Accessed 11 June 2020.
Wu D, Zhou G, Jin P, et al. Detection of colorectal cancer using a simplified SEPT9 gene methylation assay is a reliable method for opportunistic screening. J Mol Diagn. 2016;18(4):535–45.
Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for colorectal cancer: US preventive services task force recommendation statement. JAMA. 2016;315(23):2564–75.
LAM Gets FDA Breakthrough Designation for Liver Cancer Liquid Biopsy. Clinical Omics. 2019. https://www.clinicalomics.com/topics/molecular-dx-topic/lam-gets-fda-breakthrough-designation-for-liver-cancer-liquid-biopsy/. Accessed 20 May 2020.
Thrive joins liquid biopsy race. Nat Biotechnol. 2019;37(7):703.
Ofman JJ, Hall MP, Aravanis AM, Park M. GRAIL and the quest for earlier multi-cancer detection. Nature portfolio. https://media.nature.com/original/magazine-assets/d42473-020-00079-y/d42473-020-00079-y.pdf
Rossi G, Ignatiadis M. Promises and pitfalls of using liquid biopsy for precision medicine. Cancer Res. 2019;79(11):2798–804.
Cescon DW, Bratman SV, Chan SM, Siu LL. Circulating tumor DNA and liquid biopsy in oncology. Nat Cancer. 2020;1(3):276–90.
Chapman CG, Long T, Waxman I. Liquid biopsies in pancreatic cancer: targeting the portal vein. J Pancreatol. 2019;2(3):76–81.
Trudeau MT, Casciani F, Gershuni VM, et al. Defining postoperative weight change after pancreatectomy: factors associated with distinct and dynamic weight trajectories. Surgery. 2020;168(6):1041–7.
Hue JJ, Markt SC, Rao G, Winter JM. Patient-centered weight tracking as an early cancer detection strategy. J Cancer Prev. 2020;25(3):1–8.
Acknowledgment
This work was supported by the University Hospitals Ventures START (Stimulation of Teams, and Activation of Resources and Tools) Fund, with support and guidance from the University Hospitals Research Health Analytics and Informatics Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
All authors declare no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hue, J.J., Sugumar, K., Kyasaram, R.K. et al. Weight Loss as an Untapped Early Detection Marker in Pancreatic and Periampullary Cancer. Ann Surg Oncol 28, 6283–6292 (2021). https://doi.org/10.1245/s10434-021-09861-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09861-8