Abstract
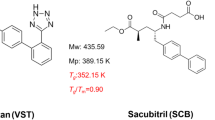
Coamorphous formulation, a homogeneous monophasic amorphous system composed of multiple components, has been demonstrated as an effective approach for delivering drugs with poor aqueous solubility. In this study, we prepared the coamorphous system composed of two poorly soluble drugs febuxostat (FEB) and indomethacin (IMC) by using cryogenic milling. The combination of these two drugs in the coamorphous form can attain a synergistic effect, especially on gout therapy. Coamorphous solid of FEB and IMC in 1:1 molar ratio exhibited superior physical stability compared with the individual amorphous components, as evidenced by X-ray powder diffractions after 30 days of storage at ambient and elevated temperature. In addition, the FEB–IMC coamorphous system has been demonstrated to show enhanced dissolution performance. The intrinsic dissolution rates of two components in the coamorphous system exhibited the synchronized drug release. Based on the FT-IR spectroscopy, the excellent physical stability and synchronized release of FEB–IMC coamorphous system could be attributed to the heterodimer structure formed by strong hydrogen bonding interactions between these drugs. Furthermore, the supersaturation potential of FEB–IMC coamorphous solids was also investigated through the cosolvent quenching method. The FEB–IMC coamorphous system can effectively inhibit the fast crystallization of FEB in the supersaturated solution. However, the maximum achievable supersaturation of IMC in the coamorphous system decreases to only one fifth of that achieved for the pure amorphous IMC. These results are relevant for understanding the physical stability and complex solution behaviors of the coamorphous formulation.








Similar content being viewed by others
References
Di L, Fish PV, Mano T. Bridging solubility between drug discovery and development. Drug Discov Today. 2012;17:486–95.
Murdande SB, Pikal MJ, Shanker RM, Bogner RH. Solubility advantage of amorphous pharmaceuticals: I. A thermodynamic analysis. J Pharm Sci. 2010;99:1254–64.
Taylor LS, Zhang GG. Physical chemistry of supersaturated solutions and implications for oral absorption. Adv Drug Deliv Rev. 2016;101:122–42.
Wyttenbach N, Kuentz M. Glass-forming ability of compounds in marketed amorphous drug products. Eur J Pharm Biopharm. 2017;112:204–8.
Vasconcelos T, Marques S, das Neves J, Sarmento B. Amorphous solid dispersions: rational selection of a manufacturing process. Adv Drug Deliv Rev. 2016;100:85–101.
Shi Q, Moinuddin SM, Cai T. Advances in coamorphous drug delivery systems. Acta Pharm Sin B. 2019;9:19–35.
Newman A, Reutzel-Edens SM, Zografi G. Coamorphous active pharmaceutical ingredient-small molecule mixtures: considerations in the choice of coformers for enhancing dissolution and oral bioavailability. J Pharm Sci. 2018;107:5–17.
Dengale SJ, Grohganz H, Rades T, Lobmann K. Recent advances in co-amorphous drug formulations. Adv Drug Deliv Rev. 2016;100:116–25.
Chavan RB, Thipparaboina R, Kumar D, Shastri NR. Coamorphous systems: a product development perspective. Int J Pharm. 2016;515:403–15.
Korhonen O, Pajula K, Laitinen R. Rational excipient selection for co-amorphous formulations. Exp Opin Drug Del. 2017;14:551–69.
Cottarel G, Wierzbowski J. Combination drugs, an emerging option for antibacterial therapy. Trends Biotechnol. 2007;25:547–55.
Keith CT, Borisy AA, Stockwell BR. Innovation: multicomponent therapeutics for networked systems. Nat Rev Drug Discov. 2005;4:71–8.
Lakshman JP, Cao Y, Kowalski J, SeraJuddin AT. Application of melt extrusion in the development of a physically and chemically stable high-energy amorphous solid dispersion of a poorly water-soluble drug. Mol Pharm. 2008;5:994–1002.
Descamps M, Willart JF. Perspectives on the amorphization/milling relationship in pharmaceutical materials. Adv Drug Deliv Rev. 2016;100:51–66.
Trasi NS, Byrn SR. Mechanically induced amorphization of drugs: a study of the thermal behavior of cryomilled compounds. AAPS PharmSciTech. 2012;13:772–84.
Moinuddin SM, Ruan S, Huang Y, Gao Q, Shi Q, et al. Facile formation of co-amorphous atenolol and hydrochlorothiazide mixtures via cryogenic-milling: enhanced physical stability, dissolution and pharmacokinetic profile. Int J Pharm. 2017;532:393–400.
Willart JF, Descamps M. Solid state amorphization of pharmaceuticals. Mol Pharm. 2008;5:905–20.
Khosravan R, Wu JT, Joseph-Ridge N, Vernillet L. Pharmacokinetic interactions of concomitant administration of febuxostat and NSAIDs. J Clin Pharmacol. 2006;46:855–66.
Maddileti D, Jayabun SK, Nangia A. Soluble cocrystals of the xanthine oxidase inhibitor febuxostat. Cryst Growth Des. 2013;13:3188–96.
Sharma OP, Patel V, Mehta T. Design of experiment approach in development of febuxostat nanocrystal: application of Soluplus® as stabilizer. Powder Technol. 2016;302:396–405.
Conaghan PG, Day RO. Risks and benefits of drugs used in the management and prevention of gout. Drug Saf. 1994;11:252–8.
Löbmann K, Strachan C, Grohganz H, Rades T, Korhonen O, et al. Co-amorphous simvastatin and glipizide combinations show improved physical stability without evidence of intermolecular interactions. Eur J Pharm Biopharm. 2012;81:159–69.
Jensen KT, Larsen FH, Cornett C, Lobmann K, Grohganz H, et al. Formation mechanism of coamorphous drug–amino acid mixtures. Mol Pharm. 2015;12:2484–92.
Qiu JB, Li G, Sheng Y, Zhu MR. Quantification of febuxostat polymorphs using powder X-ray diffraction technique. J Pharm Biomed Anal. 2015;107:298–303.
Wu T, Yu L. Surface crystallization of indomethacin below Tg. Pharm Res. 2006;23:2350–5.
Zhu L, Brian CW, Swallen SF, Straus PT, Ediger MD, et al. Surface self-diffusion of an organic glass. Phys Rev Lett. 2011;106:256103.
Chieng N, Aaltonen J, Saville D, Rades T. Physical characterization and stability of amorphous indomethacin and ranitidine hydrochloride binary systems prepared by mechanical activation. Eur J Pharm Biopharm. 2009;71:47–54.
Löbmann K, Grohganz H, Laitinen R, Strachan C, Rades T. Amino acids as co-amorphous stabilizers for poorly water soluble drugs—part 1: preparation, stability and dissolution enhancement. Eur J Pharm Biopharm. 2013;85:873–81.
Lenz E, Jensen KT, Blaabjerg LI, Knop K, Grohganz H, et al. Solid-state properties and dissolution behaviour of tablets containing co-amorphous indomethacin–arginine. Eur J Pharm Biopharm. 2015;96:44–52.
Qian S, Heng WL, Wei YF, Zhang JJ, Gao Y. Coamorphous lurasidone hydrochloride–saccharin with charge-assisted hydrogen bonding interaction shows improved physical stability and enhanced dissolution with pH-independent solubility behavior. Cryst Growth Des. 2015;15:2920–8.
Gao Y, Liao J, Qi X, Zhang J. Coamorphous repaglinide–saccharin with enhanced dissolution. Int J Pharm. 2013;450:290–5.
Kini A, Patel SB. Phase behavior, intermolecular interaction, and solid state characterization of amorphous solid dispersion of Febuxostat. Pharm Dev Technol. 2017;22:45–57.
Taylor LS, Zografi G. Spectroscopic characterization of interactions between PVP and indomethacin in amorphous molecular dispersions. Pharm Res. 1997;14:1691–8.
Löbmann K, Laitinen R, Grohganz H, Gordon KC, Strachan C, Rades T. Coamorphous drug systems: enhanced physical stability and dissolution rate of indomethacin and naproxen. Mol Pharm. 2011;8:1919–28.
Löbmann K, Laitinen R, Grohganz H, Strachan C, Rades T, Gordon KC. A theoretical and spectroscopic study of co-amorphous naproxen and indomethacin. Int J Pharm. 2013;453:80–7.
Yu L. Amorphous pharmaceutical solids: preparation, characterization and stabilization. Adv Drug Deliv Rev. 2001;48:27–42.
Jung MS, Kim JS, Kim MS, Alhalaweh A, Cho W, et al. Bioavailability of indomethacin–saccharin cocrystals. J Pharm Pharmacol. 2010;62:1560–8.
Skieneh JM, Sathisaran I, Dalvi SV, Rohani S. Co-amorphous form of curcumin–folic acid dihydrate with increased dissolution rate. Cryst Growth Des. 2017;17:6273–80.
Alleso M, Chieng N, Rehder S, Rantanen J, Rades T, et al. Enhanced dissolution rate and synchronized release of drugs in binary systems through formulation: amorphous naproxen–cimetidine mixtures prepared by mechanical activation. J Control Release. 2009;136:45–53.
Saboo S, Mugheirbi NA, Zemlyanov DY, Kestur US, Taylor LS. Congruent release of drug and polymer: a “sweet spot” in the dissolution of amorphous solid dispersions. J Control Release. 2019;298:68–82.
Laitinen R, Lobmann K, Grohganz H, Priemel P, Strachan CJ, et al. Supersaturating drug delivery systems: the potential of co-amorphous drug formulations. Int J Pharm. 2017;532:1–12.
Jackson MJ, Kestur US, Hussain MA, Taylor LS. Dissolution of danazol amorphous solid dispersions: supersaturation and phase behavior as a function of drug loading and polymer type. Mol Pharm. 2016;13:223–31.
Raina SA, Zhang GG, Alonzo DE, Wu J, Zhu D, et al. Enhancements and limits in drug membrane transport using supersaturated solutions of poorly water soluble drugs. J Pharm Sci. 2014;103:2736–48.
Alhalaweh A, Bergstrom CAS, Taylor LS. Compromised in vitro dissolution and membrane transport of multidrug amorphous formulations. J Control Release. 2016;229:172–82.
Li N, Taylor LS. Tailoring supersaturation from amorphous solid dispersions. J Control Release. 2018;279:114–25.
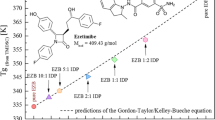
Almeida e Sousa L, Reutzel-Edens SM, Stephenson GA, Taylor LS. Assessment of the amorphous “solubility” of a group of diverse drugs using new experimental and theoretical approaches. Mol Pharm. 2015;12:484–95.
Mosquera-Giraldo LI, Taylor LS. Glass-liquid phase separation in highly supersaturated aqueous solutions of telaprevir. Mol Pharm. 2015;12:496–503.
Wallace AF, Hedges LO, Fernandez-Martinez A, Raiteri P, Gale JD, et al. Microscopic evidence for liquid–liquid separation in supersaturated CaCO3 solutions. Science. 2013;341:885–9.
Lafferrère L, Hoff C, Veesler S. Study of liquid–liquid demixing from drug solution. J Cryst Growth. 2004;269:550–7.
Ilevbare GA, Taylor LS. Liquid–liquid phase separation in highly supersaturated aqueous solutions of poorly water-soluble drugs: implications for solubility enhancing formulations. Cryst Growth Des. 2013;13:1497–509.
Indulkar AS, Box KJ, Taylor R, Ruiz R, Taylor LS. pH-dependent liquid–liquid phase separation of highly supersaturated solutions of weakly basic drugs. Mol Pharm. 2015;12:2365–77.
Trasi NS, Taylor LS. Thermodynamics of highly supersaturated aqueous solutions of poorly water-soluble drugs—impact of a second drug on the solution phase behavior and implications for combination products. J Pharm Sci. 2015;104:2583–93.
Trasi NS, Taylor LS. Dissolution performance of binary amorphous drug combinations—impact of a second drug on the maximum achievable supersaturation. Int J Pharm. 2015;496:282–90.
Arca HC, Mosquera-Giraldo LI, Dahal D, Taylor LS, Edgar KJ. Anti-HIV amorphous solid dispersions: nature and mechanisms of impacts of drugs on each other's solution concentrations. Mol Pharm. 2017;14:3617–27.
Ilevbare GA, Liu HY, Edgar KJ, Taylor LS. Maintaining supersaturation in aqueous drug solutions: impact of different polymers on induction times. Cryst Growth Des. 2013;13:740–51.
Curatolo W, Nightingale JA, Herbig SM. Utility of hydroxypropylmethylcellulose acetate succinate (HPMCAS) for initiation and maintenance of drug supersaturation in the GI milieu. Pharm Res. 2009;26:1419–31.
Acknowledgments
The authors are grateful for financial support of this work by the National Science Foundation of China (Nos. 81872813 and 81803452), the State Project for Essential Drug Research and Development (No. 2017ZX09301075), the Program of State Key Laboratory of Natural Medicines–China Pharmaceutical University (No. SKLNMZZCX201826), and the 111 project (B16046).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing financial interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moinuddin, S.M., Shi, Q., Tao, J. et al. Enhanced Physical Stability and Synchronized Release of Febuxostat and Indomethacin in Coamorphous Solids. AAPS PharmSciTech 21, 41 (2020). https://doi.org/10.1208/s12249-019-1578-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-019-1578-6