Abstract
Hip fractures can lead to functional disability and high mortality rates among elderly patients. The aim of this study was to investigate whether chronic obstructive pulmonary disease (COPD) is a risk factor for hip fracture. A retrospective population-based 4-year cohort study was conducted using case–control matched analysis of data from the Taiwan Longitudinal Health Insurance Database 2005 (LHID2005). Patients with a diagnosis of COPD between January 1, 2004 and December 31, 2007 were enrolled. A 2-stage approach and data from the National Health Interview Survey 2005 were applied to adjust for missing confounders in the LHID2005 cohort. Hazard ratios (HRs) and adjusted HRs were estimated hip fracture risk for the COPD. We enrolled 16,239 patients in the COPD cohort and 48,747 (1:3) patients in non-COPD cohort. The hip fracture incidences were 649 per 100,000 person-years in the study cohort and 369 per 100,000 person-years in non-COPD cohort. The hip fracture HR during the follow-up period was 1.78 (P < 0.001) and the adjusted hip fracture HR was 1.57 (P < 0.001) after adjustment for covariates by using the 2-stage approach method. Patients with COPD were at hip fracture risk and fracture-prevention strategies are essential for better quality of care.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a slow progressive disease characterized by chronic inflammation of the airways and airflow obstruction. COPD has a prevalence of 5–13% and is the fourth leading cause of death worldwide1,2. COPD is one of the most prevalent causes of death in North America and by 2020 it will be the third largest disease burden worldwide3,4. COPD mainly affects pulmonary function, but also affects nonrespiratory systems5,6. In addition, previous studies have reported muscle strength and exercise capacity deficits among patients with COPD resulting in impairment of postural control and balance function7,8,9,10.
Hip fracture can lead to functional disability and high mortality rates in elderly people11,12. To regain function in independent daily living, nearly all patients with hip fracture require surgery and approximately 50% of patients regain previous mobility13. In addition, approximately 25% of patients receive long-term nursing home care despite independently performing daily activities before experiencing hip fracture14,15. The medical cost incurred because of hip fracture is high, and an economic burden of more than $20 billion was estimated in 199716. Ninety percent hip fractures are caused by falls17, and fall injuries are common in patients with COPD18. A recent prospective observational study indicated that approximately one third of ambulatory patients with COPD had fall accidents during a 6-month follow-up period. We hypothesized that COPD is associated with hip fracture because fall injury rates are high among patients with COPD.
Falls in patients with COPD could have major complications, including mortality and morbidities such as hip fracture, potentially imposing an economic burden on health care services. Although previous studies have indicated a high fall incidence among patients with COPD, hip fracture risk has not been investigated extensively19. A large-scale population-based study analyzing COPD and hip fracture risk is lacking. Moreover, hip fracture prevention is a major public health concern, and identifying hip fracture risk factors is correlated to effective fall strategy establishment. Therefore, we conducted this retrospective population-based cohort study to investigate the hip fracture risk among patients with COPD.
Methods
Study design and study population
Data source
A retrospective population-based cohort study was conducted using case–control matched analysis. Patient data were obtained from the Taiwan Longitudinal Health Insurance Database 2005 (LHID2005). The National Health Insurance program, established in Taiwan in March 1995, has over 25 million enrollees and covers more than 99% of the population of Taiwan. The LHID2005 contains data on 25.68 million claims from one million beneficiaries randomly sampled from the Registry for Beneficiaries of the National Health Insurance Research Database (NHIRD). The claims files contain information on ambulatory care; inpatient care; pharmacy use; date of service; International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic codes; and claimed medical expenses. The National Health Research Institutes manages the claims data and provides scrambled random identification numbers for insured patients to protect their privacy. For ethical reasons, the database provides de-identified secondary data. The data were analyzed anonymously and the requirement for informed consent was waived by institution of review board and this study is accordance to the guideline of STROBE (STrengthening the Reporting of OBservational studies in Epidemiology).
Study patients
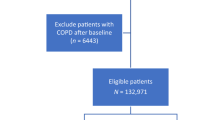
Patients with ambulatory care claims containing ICD-9-CM code 490–496 (COPD) between January 1, 2004 and December 31, 2007 were identified. To ensure that the COPD diagnoses were accurate, patients who received consistent diagnoses according to the ICD-9-CM at least 3 times in outpatient clinics or a primary diagnosis of COPD during hospitalization within 1 year were selected. Initially, 21,341 patients with COPD were enrolled. However, 4880 patients whose data were missing or were aged <50 years and 222 patients with diagnoses of previously sustained hip fracture (ICD-9-CM code 820 and 821) were excluded. The study cohort comprised 16,239 patients with COPD, and the control cohort comprised 48,717 patients without COPD in a 1:3 ratio matched by age and sex in group level. And the patients with previous hip fracture were also excluded in control cohort. Each patient was monitored for 4 years, from the entry date to the diagnosis of hip fracture in an outpatient clinic, primary diagnosis during hospitalization, or the end of 2008.
Baseline comorbidities and inhalation medication
Data on baseline variables, namely age, sex, hypertension (ICD-9-CM codes 401–405), hyperlipidemia (ICD-9-CM codes 272.0–272.4), stroke (ICD-9-CM codes 430–438), diabetes mellitus (DM; ICD-9-CM codes 250, 251), and autoimmune diseases (rheumatoid arthritis, RA; ICD-9-CM code 714.0; systemic lupus erythematous, SLE; ICD-9-CM code 710.0), were obtained for all patients. In addition, usage histories of nonsteroidal anti-inflammatory drugs (NSAIDs) and inhalation medications, such as ipratropium bromide administered using a metered-dose inhaler (MDI); fenoterol hydrobromide administered using an MDI, terbutaline sulfate administered using a Turbuhaler, or salbutamol sulfate administered using an MDI; tiotropium administered using a HandiHaler; formoterol administered using a Turbuhaler or salmeterol administered using an MDI; and formoterol/budesonide administered using a Turbuhaler or salmeterol/fluticasone administered using an MDI, were considered.
Statistical analysis and 2-stage propensity score calibration
A Cox model was used to calculate an up to 4-year hip fracture hazard function and evaluate the hip fracture risk between the COPD and control cohorts, after adjustment for age, sex, DM, hypertension, hyperlipidemia, stroke, autoimmune diseases (RA, SLE), and inhaled medication and NSAID use.
To adjust for missing confounders, namely smoking, alcohol use, and body mass index (BMI), in the LHID cohort, a 2-stage approach was applied. In previous studies with 2-stage designs, the method for adjusting for missing confounders involved combining samples from the main data and validating data18,19. According to the inclusion criteria, we identified 350 patients with COPD in the main study (LHID cohort) and 1050 age- and sex-matched participants in the National Health Interview Survey 2005 (NHIS2005) conducted during 2004–2007 (comparison cohort). The comparison cohort had data on BMI, alcohol use, and smoking, which are crucial variables for patients with COPD that were lacking in the LHID cohort. Thus, a 2-stage propensity score matching method described by Stürmer et al. was employed to adjust for the missing high-dimensional confounders20,21,22.
Let X denote an indicator variable for COPD. A value 1 is chosen for patients with COPD and 0 otherwise. Let Xc be a vector of observed confounders, namely patient age, sex, hypertension, stroke, hyperlipidemia, DM, autoimmune diseases, and inhaled medication and NSAID use. Let U denote an indicator for the missing confounders, smoking, alcohol use, and BMI. The propensity score is defined by the equation PS = Pr (X = 1|Xc), and the estimated PS and hip fracture association in a Cox proportional hazard model is defined as The propensity score
The propensity score  is defined as the error-prone variable and
is defined as the error-prone variable and  is defined as the gold standard in the validation study. The measurement error model is
is defined as the gold standard in the validation study. The measurement error model is , and the regression calibration after adjustment for Xc and U confounding factors estimator for the effect of X is
, and the regression calibration after adjustment for Xc and U confounding factors estimator for the effect of X is  21. The estimated
21. The estimated  is obtained after adjusting for missing confounders. Lin and Chen proposed TSC statistical methods. Unlike the aforementioned methods, the validity of the TSC method does not rely on a measurement error model23. We used the TSC method to estimate beta parameters and obtained results similar to those of the aforementioned process. Furthermore, hip fracture hazard curves based on time-to-event analysis (Kaplan–Meier method) for patients with COPD and the comparison cohort and hip fracture hazard curves stratified by inhaled medications usage for the COPD cohort were plotted. All data analyses were performed using the SAS statistical package (Version 9.4; SAS Institute, Cary, NC, USA). A P value of <0.05 was considered statistically significant.
is obtained after adjusting for missing confounders. Lin and Chen proposed TSC statistical methods. Unlike the aforementioned methods, the validity of the TSC method does not rely on a measurement error model23. We used the TSC method to estimate beta parameters and obtained results similar to those of the aforementioned process. Furthermore, hip fracture hazard curves based on time-to-event analysis (Kaplan–Meier method) for patients with COPD and the comparison cohort and hip fracture hazard curves stratified by inhaled medications usage for the COPD cohort were plotted. All data analyses were performed using the SAS statistical package (Version 9.4; SAS Institute, Cary, NC, USA). A P value of <0.05 was considered statistically significant.
Results
The COPD cohort in the LHID comprised 16,239 patients with COPD, and the control cohort comprised 48,717 patients without COPD. A total of 350 patients with COPD and 1050 comparison participants without COPD from the NHIS were included in the validation cohort. The demographic characteristics and comorbid medical disorders of these cohorts are shown in Table 1.
The incidence of hip fracture was 649 per 10,000 person-years and 369 per 10,000 person-years in the COPD and control cohorts, respectively. In patients with COPD, the crude hazard ratio (HR) for hip fracture occurrence was 1.78 (95% confidence interval [CI], 1.57–2.01, P < 0.001). After adjustment for age, sex, hypertension, stroke, hyperlipidemia and DM, autoimmune diseases, and inhaled medication and NSAID use, the adjusted HR was 1.59 (95% CI, 1.38–1.82, P < 0.001). After 2-stage propensity score calibration, the adjusted HR was 1.57 (95% CI, 1.36–1.81, P < 0.001) (Table 2).
Table 3 lists the incidence and hazard ratios for hip fracture in COPD patients with inhalation medication (N = 10,362) and without inhalation medication (N = 5,877) in comparison with the control cohort (N = 48,717). The incidence of hip fracture was 717 per 10,000 person-years in the COPD and inhaled medication cohort, whereas it was 595 per 10,000 person-years in the COPD without inhaled medication cohort. The crude HR of hip fracture occurrence for patients with COPD using inhaled medication was 2.04 (95% CI, 1.72–2.41, P < 0.001), and the adjusted HR was 1.72 (95% CI, 1.45–2.04, P < 0.001). The crude HR for patients with COPD not using inhaled medication was 1.63 (95% CI, 1.40–1.89, P < 0.001), and the adjusted HR was 1.46 (95% CI, 1.25–1.69, P < 0.001).
Kaplan–Meier hazard curves for hip fracture in the COPD and control cohorts over the 4-year follow-up period are shown in Fig. 1. Log-rank test analysis revealed that the patients in the COPD cohort had higher risk (HR = 1.78, P < 0.001) than those of the patients in the non-COPD cohort (Fig. 1). Patients with COPD using inhaled medications had higher HRs (HR = 1.25, 95% CI 1.03–1.52, P = 0.027) for hip fracture than those of patients not using inhaled medication (Fig. 2).
Discussion
Our large-scale population-based study revealed that patients with COPD were at an increased risk of hip fracture after we controlled for other possible contributing factors. Previous studies have revealed that most hip fractures were caused by falls and that the prevalence of falls was high among patients with COPD20. Therefore, we hypothesized that patients with COPD are at a risk of hip fracture. The pathogenesis of hip fractures could be explained by fall mechanisms among patients with COPD.
A previous study indicated that muscle strength, balance, and gait pattern could be intrinsic factors contributing to falls17,18,19. Muscle strength reduction and balance impairment can be observed in patients with COPD24. Moreover, Butcher et al. observed that patients with COPD had gait deficits9,10, which can be precipitating factors for hip fracture in patients with COPD. Adequate muscle strength and endurance are essential for maintaining postural stability and reducing postural sway8. Mathur et al. reported that patients with moderate to severe COPD had decreased muscle volume and strength and increased thigh intramuscular fat25. In addition to muscle strength, muscle endurance is affected by COPD. A case control study comparing the knee extensor muscle of patients with COPD and healthy participants indicated that patients with COPD showed compromised endurance and most of them could not complete the study protocol26. Patients with COPD had increased body sway during rest with difficulty in maintaining balance during motion of more than an arm distance27. Janssens et al. demonstrated that in patients with COPD, particularly those with inspiratory muscle weakness, postural instability was caused by decreased proprioception signal reliance on back muscles8,28. Furthermore, gait deficit is considered a contributing factor for falls in patients with COPD. Butcher et al. demonstrated that gait speed was lower in patients with COPD compared with healthy control participants in a 6-meter walking test29. In addition, a previous study noted a shorter walking distance in patients with COPD8. However, the direct correlation of gait speed and distance with falls remains uninvestigated. Moreover, kinematic variables of gait deficits, such as gait variability among patients with COPD, remain inadequately studied, and additional studies are warranted.
Nutrition deficit and muscle mass loss are common problems in patients with COPD28. Hip muscles prevent blunt injury in lateral side falls. Therefore, frail patients are less protected and more vulnerable to hip fracture30. Furthermore, vitamin D deficiency is associated with muscle weakness and postural instability, which increase the fall risk31. In addition, vitamin D deficiency is associated with secondary hyperparathyroidism, which stimulates bone resorption and increases the fracture risk32. A previous study showed that patients with COPD had low vitamin D levels33. Thus, nutrition deficit could be a factor contributing to the increased hip fracture risk among patients with COPD.
It is well established that smoking is an important risk factor for COPD and is associated with bone mineral density and increased fracture risk34. The adverse effect of smoking could explain the increased hip fracture risk for patients with COPD. Nicotine exposure reduces calcium absorption and influences bone modeling, resulting in low bone mineral density35,36,37. Therefore, smoking is a risk factor for both osteoporosis and COPD, and is a contributing factor for hip fracture among patients with COPD.
Corticosteroid use is a pathogenic factor for hip fractures among patients with COPD. It is estimated that more than 61.5% and 8.3% patients with COPD use inhaled medication and oral corticosteroids, respectively38,39. A cross-sectional study on patients with severe COPD treated with glucocorticoids with adequate calcium and vitamin levels revealed a 68% prevalence of osteoporosis and osteopenia40. A case control study with a large sample size revealed that patients with COPD using inhaled corticosteroids had a higher fracture risk than that of patients with COPD not using inhaled corticosteroids41. In addition, a systematic review and meta-analysis study revealed that a high dosage of inhaled corticosteroids is associated with an increased risk of fractures, including hip fractures, among patients with COPD. In addition to osteoporosis, respiratory and peripheral muscle weakness is caused by oral corticosteroids42. Long-term corticosteroid use may lead to muscle weakness, which is a pathogenic factor for hip fracture among patients with COPD. Furthermore, the study results revealed that patients with COPD using inhaled medication had a higher risk of experiencing hip fracture than that of patients not using the medication. Thus, steroids may play a crucial role in increasing the hip fracture risk among patients with COPD.
This study is the first to investigate COPD as a risk factor for hip fracture. Nevertheless, it is subject to several possible limitations. First, information on daily activities, smoking habits, body weight, and nutrition status is not recorded and quantified in the NHIRD. These factors are associated with the risk of hip fracture. Although smoking and malnutrition are common in patients with COPD, these confounders cannot be controlled completely in a large population-based study using the NHIRD. Therefore, we used a 2-stage propensity score calibration method and NHIS 2005 data for eliminating the confounding bias caused by smoking, alcohol use, and BMI. Second, COPD diagnosis and medical comorbidities were determined using ICD codes from the NHRID, and no information on the accuracy of these codes is available. To reduce the bias caused by the incorrect use of codes, we included patients who received 5 consecutive diagnoses of COPD in outpatient clinics or a primary diagnosis of osteoarthritis during hospitalization to ensure the validity of COPD diagnosis. Third, the influence of socioeconomic status on the risk of hip fracture was not presented in this study. Patients with higher socioeconomic status family generally had better medical resource and safer working environment than those families from lower socioeconomic status. COPD cohort could have lower socioeconomic status and lead them at higher risk of hip fracture. For considering this potential bias cuased by different socioeconomic status among COPD and non-COPD cohorts, we adjusted variable of income in further analysis and the data of adjusted HR was 1.60 (95% CI, 1.39–1.84, P < 0.001), which did not change the outcome of this study. Finally, the COPD severity stage and detailed medication data were not recorded in the NHIRD and can influence the hip fracture risk. To eliminate these biases, we controlled for possible confounders such as age, steroid use, and comorbidities among the study and control cohorts. However the limitations of propensity score analyses cannot eliminate all confounding definitely and no detailed data of oral glucocorticoid and osteoporosis medication usage were mentioned in this study.
Conclusion
This population-based retrospective cohort study revealed that patients with COPD were at a 1.57-times greater risk of sustaining hip fracture. Several factors contribute to hip fracture risk, such as falls, steroid use, muscle weakness, gait deficit, impaired balance, smoking, and nutrition deficit. We recommend implementing an appropriate hip fracture prevention strategy in the public health field by using a multidisciplinary approach to improve the quality of care for patients with COPD. Additional studies investigating the effect of hip fracture risk factors in patients with COPD are warranted.
Additional Information
How to cite this article: Huang, S.-W. et al. Chronic Obstructive Pulmonary Disease Increases the Risk of Hip Fracture: A Nationwide Population-Based Cohort Study. Sci. Rep. 6, 23360; doi: 10.1038/srep23360 (2016).
References
Vestbo, J. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 187, 347–65 (2013).
Mannino, D. M. & Buist, A. S. Global burden of COPD: risk factors, prevalence, and future trends. Lancet 370, 765–73 (2007).
Rabe, K. F. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176, 532–55 (2007).
Lopez, A. D. et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J 27, 397–412 (2006).
Wouters, E. F., Creutzberg, E. C. & Schols, A. M. Systemic effects in COPD. Chest 121, 127S–130S (2002).
Dourado, V. Z. et al. Systemic manifestations in chronic obstructive pulmonary disease. J Bras Pneumol 32, 161–71 (2006).
Ries, A. L. et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 131, 4S–42S (2007).
Butcher, S. J., Meshke, J. M. & Sheppard, M. S. Reductions in functional balance, coordination, and mobility measures among patients with stable chronic obstructive pulmonary disease. J Cardiopulm Rehabil 24, 274–80 (2004).
Smith, M. D., Chang, A. T., Seale, H. E., Walsh, J. R. & Hodges, P. W. Balance is impaired in people with chronic obstructive pulmonary disease. Gait Posture 31, 456–60 (2010).
Roig, M., Eng, J. J., Macintyre, D. L., Road, J. D. & Reid, W. D. Postural Control Is Impaired in People with COPD: An Observational Study. Physiother Can 63, 423–31 (2011).
Boonen, S. et al. Functional outcome and quality of life following hip fracture in elderly women: a prospective controlled study. Osteoporos Int 15, 87–94 (2004).
Rosell, P. A. & Parker, M. J. Functional outcome after hip fracture. A 1-year prospective outcome study of 275 patients. Injury 34, 529–32 (2003).
Morris, A. H., Zuckerman, J. D., Policy, A. C. o. H. & Practice, U. S. A. A. A. o. O. S. National Consensus Conference on Improving the Continuum of Care for Patients with Hip Fracture. J Bone Joint Surg Am 84A, 670–4 (2002).
Leibson, C. L., Tosteson, A. N., Gabriel, S. E., Ransom, J. E. & Melton, L. J. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc 50, 1644–50 (2002).
Magaziner, J. et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55, M498–507 (2000).
Braithwaite, R. S., Col, N. F. & Wong, J. B. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc 51, 364–70 (2003).
Norton, R., Campbell, A. J., Lee-Joe, T., Robinson, E. & Butler, M. Circumstances of falls resulting in hip fractures among older people. J Am Geriatr Soc 45, 1108–12 (1997).
Lawlor, D. A., Patel, R. & Ebrahim, S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ 327, 712–7 (2003).
Roig, M. et al. Falls in people with chronic obstructive pulmonary disease: an observational cohort study. Respir Med 105, 461–9 (2011).
Lin, H. W. & Chen, Y. H. Adjustment for missing confounders in studies based on observational databases: 2-stage calibration combining propensity scores from primary and validation data. Am J Epidemiol 180, 308–17 (2014).
Sturmer, T., Schneeweiss, S., Avorn, J. & Glynn, R. J. Adjusting effect estimates for unmeasured confounding with validation data using propensity score calibration. Am J Epidemiol 162, 279–89 (2005).
Lin, H. W. & Chen, Y. H. Association Analysis under Population Stratification: A Two-Stage Procedure Utilizing Population- and Family-Based Analyses. Hum Hered 69, 160–70 (2010).
Rosner, B., Spiegelman, D. & Willett, W. C. Correction of logistic regression relative risk estimates and confidence intervals for measurement error: the case of multiple covariates measured with error. Am J Epidemiol 132, 734–45 (1990).
American Geriatrics Society Panel on, E. & Osteoarthritis. Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J Am Geriatr Soc 49, 808–23 (2001).
Lord, S. R., Allen, G. M., Williams, P. & Gandevia, S. C. Risk of falling: predictors based on reduced strength in persons previously affected by polio. Arch Phys Med Rehabil 83, 757–63 (2002).
Mathur, S., Takai, K. P., Macintyre, D. L. & Reid, D. Estimation of thigh muscle mass with magnetic resonance imaging in older adults and people with chronic obstructive pulmonary disease. Phys Ther 88, 219–30 (2008).
Janaudis-Ferreira, T., Wadell, K., Sundelin, G. & Lindstrom, B. Thigh muscle strength and endurance in patients with COPD compared with healthy controls. Respir Med 100, 1451–7 (2006).
Eisner, M. D. et al. COPD as a systemic disease: impact on physical functional limitations. Am J Med 121, 789–96 (2008).
Janssens, L. et al. Proprioceptive changes impair balance control in individuals with chronic obstructive pulmonary disease. PLoS One 8, e57949 (2013).
Schols, A. M. et al. Prevalence and characteristics of nutritional depletion in patients with stable COPD eligible for pulmonary rehabilitation. Am Rev Respir Dis 147, 1151–6 (1993).
Farmer, M. E. et al. Anthropometric indicators and hip fracture. The NHANES I epidemiologic follow-up study. J Am Geriatr Soc 37, 9–16 (1989).
Pfeifer, M., Begerow, B. & Minne, H. W. Vitamin D and muscle function. Osteoporos Int 13, 187–94 (2002).
Lips, P. et al. Reducing fracture risk with calcium and vitamin D. Clin Endocrinol (Oxf) 73, 277–85 (2010).
Forli, L. et al. Vitamin D deficiency, bone mineral density and weight in patients with advanced pulmonary disease. J Intern Med 256, 56–62 (2004).
Ward, K. D. & Klesges, R. C. A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif Tissue Int 68, 259–70 (2001).
Jutberger, H. et al. Smoking predicts incident fractures in elderly men: Mr OS Sweden. J Bone Miner Res 25, 1010–6 (2010).
Law, M. R. & Hackshaw, A. K. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect. BMJ 315, 841–6 (1997).
Krall, E. A. & Dawson-Hughes, B. Smoking increases bone loss and decreases intestinal calcium absorption. J Bone Miner Res 14, 215–20 (1999).
Walker, L. M., Preston, M. R., Magnay, J. L., Thomas, P. B. & El Haj, A. J. Nicotinic regulation of c-fos and osteopontin expression in human-derived osteoblast-like cells and human trabecular bone organ culture. Bone 28, 603–8 (2001).
Tashkin, D. P. et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 359, 1543–54 (2008).
Jorgensen, N. R. et al. The prevalence of osteoporosis in patients with chronic obstructive pulmonary disease: a cross sectional study. Respir Med 101, 177–85 (2007).
Lee, T. A. & Weiss, K. B. Fracture risk associated with inhaled corticosteroid use in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 169, 855–9 (2004).
Acknowledgements
This study is based partly on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by the National Health Research Institutes in Taiwan and was supported by the National Science Council of Taiwan under grant number MOST 104-2118-M-031 -001.
Author information
Authors and Affiliations
Contributions
Conception and design, drafting of the article: S.-W.H. and H.-W.L. Analysis and interpretation of the data: S.-W.H. and H.-W.L. Critical revision of the article for important intellectual content: S.-W.H. and W.-T.W. Final approval of the article: T.-H.L., H.-W.L. and H.-C.C. Provision of study materials and patients: L.-C.C. Statistical expertise: H.-W.L. Administrative, technical, and logistic support: W.-T.W.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Huang, SW., Wang, WT., Chou, LC. et al. Chronic Obstructive Pulmonary Disease Increases the Risk of Hip Fracture: A Nationwide Population-Based Cohort Study. Sci Rep 6, 23360 (2016). https://doi.org/10.1038/srep23360
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep23360
This article is cited by
-
Hemiarthroplasty versus total hip arthroplasty for femoral neck fractures in patients with chronic obstructive pulmonary disease
European Journal of Trauma and Emergency Surgery (2021)
-
Inhaled corticosteroids in COPD and onset of type 2 diabetes and osteoporosis: matched cohort study
npj Primary Care Respiratory Medicine (2019)
-
Influence of hospital adverse events and previous diagnoses on hospital care cost of patients with hip fracture
Archives of Osteoporosis (2019)
-
Comparison of predictors of hip fracture and mortality after hip fracture in community-dwellers with and without Alzheimer’s disease – exposure-matched cohort study
BMC Geriatrics (2016)
-
COPD: osteoporosis and sarcopenia
COPD Research and Practice (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.