Abstract
Self-measured blood pressure (BP) at home, that is, home BP, is a stronger prognosticator than office BP. However, some physicians seem to think that office BP measurement is sufficient to manage hypertension. We aimed to assess whether interventions based on using home BP affect clinical outcomes including BP levels when compared with usual care based on office BP. Using the PubMed and the Cochrane Library databases (until July 2017), we searched randomized controlled trials comparing home BP-based treatment to usual care in adults with essential hypertension aged ≥18 years in an area with an established medical system. Outcomes were (1) cardiovascular events and related deaths and (2) changes in ambulatory BP levels. For outcomes of cardiovascular events and related deaths, there were no appropriate studies for the present meta-analysis. For outcomes of BP change, the analysis based on all 12 studies found by our search showed that home BP-based treatment was significantly associated with a 1.18 mmHg larger reduction in the average ambulatory systolic BP than the control group (P = 0.04). However, a high heterogeneity was observed (I2 = 75%, P < 0.0001). Based on nine studies employing a lower target BP for home BP than for office BP, the differences in the averages of the ambulatory systolic/diastolic BP changes between the two groups were 3.62/2.16 mmHg, respectively (P < 0.0001). No significant heterogeneity was observed (I2 = 0%, P ≤ 0.59). Home BP-based treatment is strongly recommended to control BP, especially in the setting of a lower home BP target than an office BP target level.
Similar content being viewed by others
Introduction
High blood pressure (BP) is still strongly related to health loss worldwide [1], and hence, the proper management of hypertension is an important task for public health. To manage high BP adequately, a reliable measurement of BP is essential.
BP obtained based on casual measurements at the office has been the primary BP information available for the diagnosis and treatment of hypertension. On the other hand, self-measured BP at home, that is, home BP, is more reliable and reproducible [2, 3] and, therefore, is a stronger predictor of cardiovascular disease and is more strongly related to targeted organ damage than office BP [4,5,6,7,8,9,10,11]. Furthermore, since home BP can provide a greater number of readings, it allows us to precisely evaluate long-term BP and the BP-lowering effects of antihypertensive drugs [3]. In the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH) 2014, home BP has a higher priority than office BP for the diagnosis of hypertension [12].
While there are many studies indicating the usefulness of home BP measurements, a few physicians think that office BP measurement is sufficient to manage hypertension in a clinical practice [13]. This divergence of views on home BP measurements should be resolved. Previous meta-analyses [14,15,16,17,18] demonstrated that antihypertensive treatment based on home BP could be more effective in improving BP control than that based on office BP. However, these meta-analyses evaluated the BP reduction in each arm mainly using office BP, which has a white coat effect [14,15,16,17,18]. Meanwhile, data on ambulatory BP reduction before and after patient allocation are available in several randomized controlled studies examining the clinical usefulness of home BP-based treatment. Ambulatory BP is sufficiently reliable to be used for evaluations of antihypertensive drug effects [19]. Ambulatory BP monitoring can be a third option for BP measurement when we examine the effect of home BP-based treatment interventions. Therefore, we aimed to assess whether interventions using home BP can affect ambulatory BP levels as well as clinical outcomes, including cardiovascular outcomes, when compared with usual care based on office BP.
Methods
Outline and outcomes
These clinical question (CQ) 1 members conducted this meta-analysis to assess whether antihypertensive treatment based on home BP is superior to that based on office BP for achieving the following outcomes:
-
1.
Cardiovascular events and related deaths (cardiovascular outcome).
-
2.
Change in ambulatory BP levels (BP change outcome).
We conducted a systematic review of the literature using the approach recommended by the PRISMA statement [20].
Search strategy
Relevant studies were identified by searching PubMed and the Cochrane Library database (until 4 July 2017). Two systematic reviewers (MS and TM) separately constructed the search strategy and searched the databases using relevant text words including home BP, telemedicine, telemonitoring, and randomized controlled trial (see online supplement, Supplementary Tables 1–7). For the outcome relating to BP change, Reviewer No. 1 searched the database after January 2012 because Omboni et al. and Duan et al. had already picked up studies reported before our searches (see online supplement, Supplementary Tables 1 and 2) [14, 15]. Reviewer No. 1 further used the text words related to cardiovascular disease when the outcome was set as cardiovascular disease (see online supplement, Supplementary Tables 3 and 4). Reviewer No. 2 used the same search strategy regardless of the type of outcomes (see online supplement, Supplementary Tables 5 and 6). The search was limited to randomized controlled trials reported in English. Reference lists from identified trials by each reviewer and review articles were manually scanned to identify any other relevant studies.
Eligibility criteria
We included randomized controlled trials comparing home BP-based treatment to usual care in adults with essential hypertension aged ≥18 years old in an area with an established medical system. Studies adding any support to home BP intervention were included in the present meta-analysis. For cardiovascular outcomes, we excluded studies not assessing any cardiovascular events or deaths. For BP change outcomes, we excluded studies evaluating only office BP as an outcome since the white coat effect might be affecting office BP.
Methods of review
The two systematic review members independently reviewed each study that was found and gathered based on the search strategy. Disagreements were resolved by consensus or by discussion with the group members for this CQ1 (TO and SH). When a similar meta-analysis report was found, we reviewed it and used the appropriate studies that were included in the report. We abstracted data from each report including the authors, year of publication, study design, study procedure and target BP level in both the intervention and control arm, sample size, the number of participants, participants’ characteristics, duration of follow-up, and outcomes including the number of deaths, the number or rate of cardiovascular events, systolic/diastolic BP at baseline and end of study, and the amplitude of BP change.
The Cochrane Collaboration Risk of Bias Tool was used to evaluate risk of bias. Discrepancies were resolved by the project methodologist and/or the chief medical officer.
Quality assessment of the risk of bias was undertaken for the included studies, which was assessed by two authors (MS and TM) in accordance with the guidelines of the Cochrane Handbook for Systematic Reviews of Interventions: version 5.0.2 (The Cochrane Collaboration, Oxford, UK). Quality was assessed for each study in terms of random risk of selection, performance bias, detection bias, and attrition bias. We evaluated the total quality of the meta-analysis in terms of indirectness, inconsistency, imprecision, and publication bias using the three grades of “not serious”, “serious”, and “very serious”.
Statistical analysis
Mantel–Haenszel fixed-effect meta-analysis was used to assess the cardiovascular outcome. The BP change outcome was assessed as the difference in BP changes between the two study arms. This change was computed by the average value at baseline subtracted from that available at the end of follow-up. Although 24-h ambulatory BP was primarily used, we used daytime BP instead in studies not reporting 24-h ambulatory BP values. Weighted mean differences with 95% confidence intervals were calculated using a fixed effects model. The SD of the BP change in each study arm was necessary to evaluate the significance and the 95% confidence intervals. In case the SD of the BP changes was missing, it was calculated by the following formula: a square root of (squared SD of BP value at baseline + SD of BP value at last follow-up). When either the SD of BP at baseline or SD of BP at the end of follow-up was missing, an average value from the other studies reporting the corresponding value was imputed [21]. As sensitivity analyses, we performed additional analyses after excluding the studies employing the same target BP for both the home BP and office BP arms. Home BP is usually 5 mmHg lower than office BP [12]. For example, a target home systolic BP of 140 mmHg corresponds to a target office systolic BP of 145 mmHg. Under this situation, if the target office systolic BP is set as 140 mmHg for the usual care group, the potential high target BP in home BP-based treatment can result in a higher follow-up ambulatory BP than in usual care, regardless of the home BP-treatment effect. We further conducted a stratification analysis according to the use of a telemonitoring technique for the intervention arm. An analysis after excluding the study reporting only daytime BP changes was also performed. Publication bias was examined graphically by funnel plots. Statistical heterogeneity among studies was assessed by the chi-square test. All analyses were conducted by Review Manager (RevMan) Version 5.3.5. Statistical significance was accepted as an α-level of less than 0.05 on two-sided tests. Data are expressed as the mean ± standard deviation (SD) unless otherwise noted. The Delphi method, in which the JSH guideline committee members anonymously answered a questionnaire sent twice or more, was used to decide the conclusion of the present analysis.
Results
Cardiovascular outcome
We screened 4845 records and assessed 60 articles for eligibility. However, there were no appropriate studies for the present meta-analysis for cardiovascular outcomes, mostly because there was no information reported for cardiovascular events or death (see online supplement, Supplementary Figure 1). One study reported the number of patients hospitalized because of heart failure or other cardiovascular disease [22]. However, other information was missing, and only heart failure patients were included in that study [22]. We finally concluded that the study was not eligible.
BP change outcome
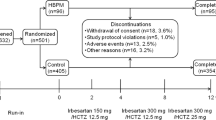
We first screened 3004 records, and the present meta-analysis finally included 12 studies [23,24,25,26,27,28,29,30,31,32,33,34] (see online supplement, Supplementary Figure 2). Of those, seven studies combined a telemonitoring technique with home BP measurements in the intervention group (Table 1).
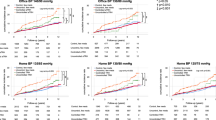
Summary of outcomes
Table 2 shows the BP change in each study. In the analysis of all 12 studies included, home BP-based treatment was significantly associated with a 1.18 [0.03, 2.32] mmHg larger reduction in the average ambulatory systolic BP than the control group (P = 0.04), although there was no significant difference in diastolic ambulatory BP (0.18 [−0.60, 0.95], P = 0.66) (Fig. 1). However, a high heterogeneity was observed in the analysis (I2 = 75%, P < 0.0001 in ambulatory systolic BP and I2 = 74%, P < 0.0001 in ambulatory diastolic BP) (Fig. 1). We then excluded three studies [23, 33, 34] employing the same target BP for both home and office BP. The meta-analysis including the remaining nine studies [24,25,26,27,28,29,30,31,32] showed a greater reduction in average ambulatory BP in the home BP-based treatment group than that in the control group without heterogeneity (I2 = 0%, P = 0.59 in ambulatory systolic BP and I2 = 0%, P = 0.53 in ambulatory diastolic BP) (Fig. 2). The differences in the BP changes between the intervention and control groups were 3.64 mmHg for ambulatory systolic BP and 2.16 mmHg for ambulatory diastolic BP (P < 0.0001 in both systolic and diastolic BP). Similar results were observed in the analysis based on the studies using a telemonitoring technique for home BP intervention (the difference in ambulatory BP [95% confidence intervals]: −3.96 [−5.56, −2.36] for systolic BP, −2.03 [−3.29, −0.76] for diastolic BP) (see online supplement, Supplementary Figure 3). In the analysis based on the two studies without a telemonitoring technique, the difference in BP changes among groups were similar but relatively small (the difference in ambulatory BP [95% confidence intervals]: −2.56 [−5.49, 0.38] for systolic BP, −2.41 [−4.15, −0.68] for diastolic BP), and the difference in systolic BP change between groups was not significant (P = 0.09) (see online supplement, Supplementary Figure 4).
Home BP-based treatment versus usual care for ambulatory BP changes in 12 studies. The difference in ambulatory BP changes between interventions (home BP-based treatment) and control (usual care) groups. The ambulatory BP change was calculated as ambulatory BP at follow-up examination—that is at baseline. The difference in ambulatory BP was calculated as ambulatory BP change in the intervention group−ambulatory BP change in the control group
We excluded the five studies [23, 26,27,28, 30] that only reported daytime BP changes and not 24-h ambulatory BP changes. The meta-analysis based on the remaining seven studies [24, 25, 29, 31,32,33,34] revealed no significant difference in 24-h ambulatory systolic/diastolic BP changes between the intervention and control groups (the difference in 24-h ambulatory BP [95% confidence intervals]: −0.53 [−1.87, 0.80] for systolic BP, 0.22 [−0.66, 1.10] for diastolic BP) (Supplementary Figure 5). However, a strong heterogeneity among studies was observed (I2 = 85%, P < 0.0001 in systolic BP and I2 = 84%, P < 0.0001 in diastolic BP) (Supplementary Figure 5). After further excluding two studies [33, 34] using a different BP goal for each treatment arm, home BP-based treatment was significantly associated with a −4.08 [−5.88, −2.27]/−2.64 [−3.96, −1.32] mmHg larger reduction in average 24-h ambulatory systolic/diastolic BP than the control group (P < 0.0001), respectively, showing no significant heterogeneity between studies (I2 = 17%, P = 0.31 in systolic BP and I2 = 10%, P = 0.35 in diastolic BP) (Supplementary Figure 6).
Risk of bias
In eight studies, the randomization procedures were appropriate and were concealed from physicians and researchers until the analysis was complete [24, 26,27,28, 31,32,33,34]. The randomization method or the allocation concealment used was unclear in other studies [23, 25, 29, 30], although most of them just stated that the patients were randomly assigned to either study arm. Since the patients must have measured their home BP and physicians mostly titrate antihypertensive therapy based on the home BP values, it is impossible to blind the patients or clinicians to the allocation, potentially causing a high-performance bias. The detailed evaluations for risk of bias including attrition bias are indicated in Supplementary Table 1 (see online supplement).
The present meta-analysis included one study based on patients with essential hypertension but having a history of stroke or transient ischemic attack [26]. Since other studies included hypertensive patients, which are common in a general clinical practice, the risk of indirectness was not serious from this point of view. However, taking the seven studies [26,27,28,29,30,31,32] using telemonitoring systems into account, the risk of indirectness was finally considered to be “serious” since telemonitoring systems have not become widespread.
High heterogeneity was observed in the analysis based on all 12 studies. Since only three studies employing the same target BP strongly affected it, the inconsistency of the present results was taken as “serious”. The risk of imprecision was “not serious” because of the large number of patients (total n = 2953). A “serious” publication bias was likely to be present since the funnel plot showed an asymmetry due to the small sample sizes of the individual studies (see online supplement, Supplementary Figure 6).
Discussion
Antihypertensive treatment according to home BP was associated with a greater reduction in ambulatory BP when compared with office BP-based treatment in the present meta-analysis (Fig. 1). However, we observed a high heterogeneity, which could be caused by the three studies [23, 33, 34] employing the same target BP for both home and office readings. These three studies were conducted before the difference between home BP and office BP was widely recognized [23, 33, 34]. In two of these studies, the same reference values seemed to be used because doing so enabled the physician at the coordinating center who adjusted the treatment to remain blinded during treatment decisions [33, 34]. The incidence of cardiovascular disease by office BP corresponded to that of a 5 mmHg lower value of home BP in a previous meta-analysis [7]. As recommended by most of the current guidelines [12, 35, 36] other than the ACC/AHA guidelines, a target home BP set at 5 mmHg lower than that for the office BP is considered to be reasonable. This threshold can also be useful for ambulatory BP reduction based on the present results.
We could not perform a meta-analysis of cardiovascular outcomes since there were no appropriate randomized controlled trials. Therefore, no direct effects of home BP-based treatment on the prevention of cardiovascular disease could be assessed in the present study. However, from the results of the BP change outcome, it is clear that home BP-based treatment can be more useful to control BP than conventional treatment. Our outcome measure was based on ambulatory BP, which is a stronger predictor of cardiovascular disease and a more accurate index for assessing hypotensive effects than office BP [8, 12, 19, 37, 38]. Since an elevated ambulatory BP is a robust risk factor for cardiovascular disease [12, 37], we concluded that home BP-based treatment can strongly contribute to the prevention of cardiovascular disease. In the sensitivity analysis after excluding the studies using a different BP goal for each treatment arm (Fig. 2), the home BP-based treatment was found to contribute to a mean ambulatory systolic/diastolic BP reduction of 3.64/2.16 mmHg when compared with the office BP-based treatment. Based on the cardiovascular risk estimation by a previous meta-analysis based on 24-h ambulatory BP [37], these reductions in ambulatory systolic/diastolic BP would be expected to reduce cardiovascular disease risk by 16.6%/16.2%, respectively. In the present study, when the included studies were restricted to those based on 24-h ambulatory BP data, a very similar difference in BP change between groups was observed (Supplementary Figure 6). Furthermore, the Hypertension Objective Treatment Based on Measurement by Electrical Devices of BP (HOMED-BP) study demonstrated that home BP more strongly predicted cardiovascular risk than office BP in Japanese hypertensive patients [4, 39]. Home BP measurements allow us to evaluate the patients’ BP, the antihypertensive effects, and seasonable and day-to-day BP variation during treatment in the long term. Home BP measurements are also considered useful for improving patients’ adherence [12]. Most hypertension management guidelines already recommend home BP measurements per se [12, 35, 36, 40]. Consequently, home BP-based treatment is a reasonable approach to prevent cardiovascular disease. Since home BP devices have been widespread among the Japanese [12], general practitioners in such a country may adopt home BP-based treatment easily. However, targeting the goal recommended by the JSH guideline would be necessary to achieve appropriate BP control and subsequent reduction of cardiovascular risk. Of the excluded three studies [23, 33, 34] employing the same target BP for both home and office readings, one study seems to have been conducted before the target BP based on home BP measurement was established [23].
After conduction of the present meta-analysis, McManus et al. [41] reported new results from Telemonitoring and/or Self-monitoring in Hypertension 4 (TASMINH4) trial. The TASMINH4 trial assessed the efficacy of home BP-based treatment, with or without telemonitoring, compared with usual care in United Kingdom hypertensive patients. Although the primary outcome was office BP measured by an automated device, home BP was targeted at 5 mmHg lower than office BP in the intervention arm [41]. When compared with usual care, the home BP-based treatment without or with telemonitoring was associated with a mean 3.5 or 4.7 mmHg larger reduction in systolic BP, respectively [41]. Their findings support our results.
The methods of BP measurement and ascertainment of events were not identical among cohorts. Similarly, substantial differences in participant characteristics among cohorts were observed, which may affect our findings. The cumulative cardiovascular death risk in individuals up to 84 years old clearly increased across BP categories. Since the present study includes only Japanese populations, there is no race-ethnic heterogeneity. Therefore, the influence of the differences between cohorts may be limited.
We found several high risks of bias. Most studies had very high performance bias because of their study design. Physicians adjusted treatments according to patients’ home BP and therefore needed to know the treatment allocation. However, a physician’s approach is essential for home BP-based treatment. The high-performance bias in the present study would not be expected to affect our conclusion.
Conclusion
Home BP-based treatment is strongly recommended from the present results. However, the home BP target level needs to be that recommended by the JSH guideline. An appropriate method for home BP measurement is also necessary.
Change history
10 June 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317:165–82.
Imai Y, Obara T, Asamaya K, Ohkubo T. The reason why home blood pressure measurements are preferred over clinic or ambulatory blood pressure in Japan. Hypertens Res. 2013;36:661–72.
Imai Y, Kario K, Shimada K, Kawano Y, Hasebe N, Matsuura H, et al. The Japanese Society of Hypertension Guidelines for Self-monitoring of Blood Pressure at Home (Second Edition). Hypertens Res. 2012;35:777–95.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, et al. Hypertension objective treatment based on measurement by electrical devices of blood pressure. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res. 2012;35:1102–10.
Ohkubo T, Asayama K, Kikuya M, Metoki H, Hoshi H, Hashimoto J, et al. How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens. 2004;22:1099–104.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–5.
Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, Kikuya M. et al. International Database of Home blood pressure in relation to Cardiovascular Outcome Investigators. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension. 2013;61:27–34.
Satoh M, Asayama K, Kikuya M, Inoue R, Metoki H, Hosaka M, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: The Ohasama Study. Hypertension. 2016;67:48–55.
Fujiwara T, Yano Y, Hoshide S, Kanegae H, Kario K. Association of cardiovascular outcomes with masked hypertension defined by home blood pressure monitoring in a Japanese general practice population. JAMA Cardiol. 2018;3:583–90.
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S. et al. J-HOP Study Group. Morning and evening hHome blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: The Japan Morning Surge-Home Blood Pressure Study. Hypertension. 2016;68:54–61.
Hoshide S, Kario K, Yano Y, Haimoto H, Yamagiwa K, Uchiba K. et al. J-HOP Study Group. Association of morning and evening blood pressure at home with asymptomatic organ damage in the J-HOP Study. Am J Hypertens. 2014;27:939–47.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M. et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Obara T, Ohkubo T, Fukunaga H, Kobayashi M, Satoh M, Metoki H, et al. Practice and awareness of physicians regarding home blood pressure measurement in Japan. Hypertens Res. 2010;33:428–34.
Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens. 2013;31:455–67. discussion 467-468
Duan Y, Xie Z, Dong F, Wu Z, Lin Z, Sun N, et al. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertens. 2017;31:427–37.
Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57:29–38.
Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–94.
Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004;329:145.
JCS Joint Working Group. Guidelines for the clinical use of 24 h ambulatory blood pressure monitoring (ABPM) (JCS 2010): – digest version. Circ J. 2012;76:508–19.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol. 2006;59:7–10.
Cleland JG, Louis AA, Rigby AS, Janssens U, Balk AH. Ten-Hms Investigators. Noninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the Trans-European Network-Home-Care Management System (TEN-HMS) study. J Am Coll Cardiol. 2005;45:1654–64.
Broege PA, James GD, Pickering TG. Management of hypertension in the elderly using home blood pressures. Blood Press Monit. 2001;6:139–44.
Fuchs SC, Ferreira-da-Silva AL, Moreira LB, Neyeloff JL, Fuchs FC, Gus M, et al. Efficacy of isolated home blood pressure monitoring for blood pressure control: randomized controlled trial with ambulatory blood pressure monitoring—MONITOR study. J Hypertens. 2012;30:75–80.
Godwin M, Lam M, Birtwhistle R, Delva D, Seguin R, Casson I, et al. A primary care pragmatic cluster randomized trial of the use of home blood pressure monitoring on blood pressure levels in hypertensive patients with above target blood pressure. Fam Pract. 2010;27:135–42.
Hanley J, Fairbrother P, Krishan A, McCloughan L, Padfield P, Paterson M, et al. Mixed methods feasibility study for a trial of blood pressure telemonitoring for people who have had stroke/transient ischaemic attack (TIA). Trials. 2015;16:117.
Madsen LB, Kirkegaard P, Pedersen EB. Blood pressure control during telemonitoring of home blood pressure. A randomized controlled trial during 6 months. Blood Press. 2008;17:78–86.
McKinstry B, Hanley J, Wild S, Pagliari C, Paterson M, Lewis S, et al. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ. 2013;346:f3030.
Neumann CL, Menne J, Rieken EM, Fischer N, Weber MH, Haller H, et al. Blood pressure telemonitoring is useful to achieve blood pressure control in inadequately treated patients with arterial hypertension. J Hum Hypertens. 2011;25:732–8.
Parati G, Omboni S, Albini F, Piantoni L, Giuliano A, Revera M. et al. Tele BPCare Study Group. Home blood pressure telemonitoring improves hypertension control in general practice. The TeleBPCare study. J Hypertens. 2009;27:198–203.
Rinfret S, Lussier MT, Peirce A, Duhamel F, Cossette S, Lalonde L. et al. Loyal Study Investigators. The impact of a multidisciplinary information technology-supported program on blood pressure control in primary care. Circ Cardiovasc Qual Outcomes. 2009;2:170–7.
Rogers MA, Small D, Buchan DA, Butch CA, Stewart CM, Krenzer BE, et al. Home monitoring service improves mean arterial pressure in patients with essential hypertension. A randomized, controlled trial. Ann Intern Med. 2001;134:1024–32.
Staessen JA, Den Hond E, Celis H, Fagard R, Keary L, Vandenhoven G, O’Brien ET. Treatment of Hypertension Based on Home or Office Blood Pressure Trial Investigators. Antihypertensive treatment based on blood pressure measurement at home or in the physician’s office: a randomized controlled trial. JAMA. 2004;291:955–64.
Verberk WJ, Kroon AA, Lenders JW, Kessels AG, van Montfrans GA, Smit AJ. et al.Home Versus Office Measurement Reduction of Unnecessary Treatment Study Investigators. Self-measurement of blood pressure at home reduces the need for antihypertensive drugs: a randomized, controlled trial. Hypertension. 2007;50:1019–25.
National Institute for Health and Clinical Excellence (NICE). Hypertension (CG127): clinical management of primary hypertension in adults. https://www.nice.org.uk/guidance/CG127. Accessed 9 2018.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M. et al. ESC Scientific Document Group. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Li Y, Wei FF, Thijs L, Boggia J, Asayama K, Hansen TW. et al. International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes Investigators. Ambulatory hypertension subtypes and 24-hour systolic and diastolic blood pressure as distinct outcome predictors in 8341 untreated people recruited from 12 populations. Circulation. 2014;130:466–74.
Asayama K, Thijs L, Li Y, Gu YM, Hara A, Liu YP. et al. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Setting thresholds to varying blood pressure monitoring intervals differentially affects risk estimates associated with white-coat and masked hypertension in the population. Hypertension. 2014;64:935–42.
Noguchi Y, Asayama K, Staessen JA, Inaba M, Ohkubo T, Hosaka M. et al. HOMED-BP study group. Predictive power of home blood pressure and clinic blood pressure in hypertensive patients with impaired glucose metabolism and diabetes. J Hypertens. 2013;31:1593–602.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
McManus RJ, Mant J, Franssen M, Nickless A, Schwartz C, Hodgkinson J. et al.TASMINH Investigators. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018;391:949–59.
Acknowledgements
This study was supported by the JSH guideline committee.
Authors’ contributions
MS and TM wrote the first draft of this manuscript. All authors conducted this study and commented on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Satoh, M., Maeda, T., Hoshide, S. et al. Is antihypertensive treatment based on home blood pressure recommended rather than that based on office blood pressure in adults with essential hypertension? (meta-analysis). Hypertens Res 42, 807–816 (2019). https://doi.org/10.1038/s41440-019-0221-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0221-y
Keywords:
This article is cited by
-
The quality of patients’ self-blood pressure measurements: a cross-sectional study
BMC Cardiovascular Disorders (2021)
-
A randomized controlled trial on home blood pressure monitoring and quality of care in stage 2 and 3 hypertension
Hypertension Research (2021)
-
Predictive power of home blood pressure measurement for cardiovascular outcomes in patients with type 2 diabetes: KAMOGAWA-HBP study
Hypertension Research (2021)
-
Home and office blood pressure: time to look at the individual patient
Hypertension Research (2021)
-
Differences between home blood pressure and strictly measured office blood pressure and their determinants in Japanese men
Hypertension Research (2021)