Abstract
The frequency of endoscopic complications is likely to rise owing to the increased number of indications for therapeutic procedures and also to the increased complexity of endoscopic techniques. Informed patient consent should be obtained as part of the procedure. Prevention of endoscopic adverse events is based on knowledge of the relevant risk factors and their mechanisms of occurrence. Thus, suitable training of future gastroenterologists and endoscopists is required for these complex procedures. When facing a complication, appropriate management is generally provided by an early diagnosis followed by prompt therapeutic care tailored to the situation. The most common complications of diagnostic and therapeutic upper gastrointestinal endoscopy, retrograde cholangiopancreatography, small bowel endoscopy and colonoscopy are reviewed here. Different modalities of medical, endoscopic or surgical management are also considered.
Key Points
-
Avoiding unnecessary invasive examinations is the best way to prevent endoscopic complications
-
Correct information about the patient and informed patient consent are paramount
-
Acquiring and maintaining expertise and competency in specific procedures is essential to reduce the risk of adverse events
-
Standardized treatments, training and guidelines are required to prevent and manage adverse events
-
Assessing center-specific and operator-specific complication rates could lead to improved quality and safety of endoscopic procedures
-
The appropriate management of complications requires early diagnosis and prompt therapeutic care
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cotton, P. B. Outcomes of endoscopy procedures: struggling towards definitions. Gastrointest. Endosc. 40, 514–518 (1994).
Cotton, P. B. et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest. Endosc. 71, 446–454 (2010).
Quine, M. A. et al. A. Prospective audit of upper gastrointestinal endoscopy in two regions of England: safety, staffing, and sedation methods. Gut 36, 462–467 (1995).
Bowles, C. J. et al. A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut 53, 277–283 (2004).
Boustière, C. et al. Endoscopy and antiplatelet agents. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 43, 445–461 (2011).
Kimmery, M. B. et al. Technology assessment position paper: transmission of infection by gastrointestinal endoscopy. Gastrointest. Endosc. 39, 885–888 (1993).
ASGE Quality Assurance In Endoscopy Committee et al. Multisociety guideline on reprocessing flexible gastrointestinal endoscopes: 2011. Gastrointest. Endosc. 73, 1075–1084 (2011).
Beilenhoff, U. et al. ESGE/ESGENA guideline for process validation and routine testing for reprocessing endoscopes in washer-disinfectors, according to the European Standard prEN ISO 15883 parts 1, 4 and 5. Endoscopy 39, 85–94 (2007).
[No authors listed] Occupational exposure to bloodborne pathogens; needlestick and other sharps injuries; final rule. Occupational Safety and Health Administration (OSHA), Department of Labor. Final rule; request for comment on the Information Collection (Paperwork) Requirements. Fed. Regist. 66, 5318–5325 (2001).
U.S. Public Health Service. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HBV, HCV and HIV and recommendations for post-exposure prophylaxis. MMWR Recomm. Rep. 50, 1–52 (2001).
Silvis, S. E., Nebel, O., Rogers, G., Sugawa, C. & Mandelstam, P. Endoscopic complications. Results of the 1974 American Society for Gastrointestinal Endoscopy Survey. JAMA 235, 928–930 (1976).
Montalvo, R. D. & Lee, M. Retrospective analysis of iatrogenic Mallory–Weiss tears occurring during upper gastrointestinal endoscopy. Hepatogastroenterology 43, 174–177 (1996).
Van Os, E. C., Kamath, P. S., Gostout, C. J. & Heit, J. A. Gastroenterological procedures among patients with disorders of hemostasis: evaluation and management recommendations. Gastrointest. Endosc. 50, 536–543 (1999).
Straumann, A. et al. Eosinophilic esophagitis: analysis of food impaction and perforation in 251 adolescent and adult patients. Clin. Gastroenterol. Hepatol. 6, 598–600 (2008).
Robles-Medranda, C., Villard, F., Bouvier, R., Dumortier, J. & Lachaux, A. Spontaneous esophageal perforation in eosinophilic esophagitis in children. Endoscopy 40 (Suppl. 2), E171 (2008).
Green, J. Guidelines on Complications of Gastrointestinal Endoscopy. British Society of Gastroenterology [online], (2006).
Boeckxtaens, G. E. et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N. Engl. J. Med. 364, 1807–1816 (2011).
Clouse, R. E. Complications of endoscopic gastrointestinal dilation techniques. Gastrointest. Endosc. Clin. N. Am. 6, 323–341 (1996).
Hernandez, L. V., Jacobson, J. W. & Harris, M. S. Comparison among the perforation rates of Maloney, balloon, and savary dilation of esophageal strictures. Gastrointest. Endosc. 51, 460–462 (2000).
Metman, E. H. et al. Risk factors for immediate complications after progressive pneumatic dilation for achalasia. Am. J. Gastroenterol. 94, 1179–1185 (1999).
Cox, J. G. et al. Balloon or bougie for dilatation of benign esophageal stricture? Dig. Dis. Sci. 39, 776–781 (1994).
Saeed, Z. A. et al. Prospective randomized comparison of polyvinyl bougies and through-the-scope balloons for dilation of peptic strictures of the esophagus. Gastrointest. Endosc. 41, 189–195 (1995).
Nicholson, D. A. et al. The cost effectiveness of metal oesophageal stenting in malignant disease compared with conventional therapy. Clin. Radiol. 54, 212–215 (1999).
Dumonceau, J. M., Cremer, M., Lalmand, B. & Devière, J. Esophageal fistula sealing: choice of stent, practical management, and cost. Gastrointest. Endosc. 49, 70–78 (1999).
Eisendrath, P. et al. Endotherapy including temporary stenting of fistulas of the upper gastrointestinal tract after laparoscopic bariatric surgery. Endoscopy 39, 625–630 (2007).
Swinnen, J. et al. Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest. Endosc. 73, 890–899 (2011).
Verschuur, E. M., Steyerberg, E. W., Kuipers, E. J. & Siersema, P. D. Effect of stent size on complications and recurrent dysphagia in patients with esophageal or gastric cardia cancer. Gastrointest. Endosc. 65, 592–601 (2007).
Sgourakis, G. et al. The use of self-expanding stents in esophageal and gastroesophageal junction cancer palliation: a meta-analysis and meta-regression analysis of outcomes. Dig. Dis. Sci. 55, 3018–3030 (2010).
May, A. et al. A prospective randomized trial of two different endoscopic resection techniques for early stage cancer of the esophagus. Gastrointest. Endosc. 58, 167–175 (2003).
Okano, A., Hajiro, K., Takakuwa, H., Nishio, A. & Matsushita, M. Predictors of bleeding after endoscopic mucosal resection of gastric tumors. Gastrointest. Endosc. 57, 687–690 (2003).
Ahmad, N. A., Kochman, M. L., Long, W. B., Furth, E. E. & Ginsberg, G. G. Efficacy, safety, and clinical outcomes of endoscopic mucosal resection: a study of 101 cases. Gastrointest. Endosc. 55, 390–396 (2002).
Katada, C. et al. Esophageal stenosis after endoscopic mucosal resection of superficial esophageal lesions. Gastrointest. Endosc. 57, 165–169 (2003).
Apel, D., Jakobs, R., Spiethoff, A. & Riemann, J. F. Follow-up after endoscopic snare resection of duodenal adenomas. Endoscopy 37, 444–448 (2005).
Dumot, J. A. & Greenwald, B. D. Argon plasma coagulation, bipolar cautery, and cryotherapy: ABC's of ablative techniques. Endoscopy 40, 1026–1032 (2008).
Pouw, R. E., Sharma, V. K., Bergman, J. J. & Fleischer, D. E. Radiofrequency ablation for total Barrett's eradication: a description of the endoscopic technique, its clinical results and future prospects. Endoscopy 40, 1033–1040 (2008).
Marmo, R. et al. Dual therapy versus monotherapy in the endoscopic treatment of high-risk bleeding ulcers: a meta-analysis of controlled trials. Am. J. Gastroenterol. 102, 279–289 (2007).
Lazo, M. D. et al. Effect of injection sclerosis with alcohol on the rebleeding rate of gastroduodenal peptic ulcers with nonbleeding visible vessels: a prospective, controlled trial. Am. J. Gastroenterol. 87, 843–846 (1992).
Rutgeerts, P. et al. Neodymium-YAG laser photocoagulation versus multipolar electrocoagulation for the treatment of severely bleeding ulcers: a randomized comparison. Gastrointest. Endosc. 33, 199–202 (1987).
Lau, J. Y. W. et al. Endoscopic retreatment compared with surgery in patients with recurrent bleeding after initial endoscopic control of bleeding ulcers. N. Engl. J. Med. 340, 751–756 (1999).
Gilbert, D. A. et al. Status evaluation: hot biopsy forceps. American Society for Gastrointestinal Endoscopy. Technology Assessment Committee. Gastrointest. Endosc. 38, 753–756 (1992).
Lo, G. H. et al. Emergency banding ligation versus sclerotherapy for the control of active bleeding from esophageal varices. Hepatology 25, 1101–1104 (1997).
Stiegmann, G. V. et al. Endoscopic sclerotherapy as compared with endoscopic ligation for bleeding esophageal varices. N. Engl. J. Med. 326, 1527–1532 (1992).
de Franchis, R. Updating consensus in portal hypertension: report of the Baveno III Consensus Workshop on definitions, methodology and therapeutic strategies in portal hypertension. J. Hepatol. 33, 846–852 (2001).
Binmoeller, K. F. Glue for gastric varices: some sticky issues. Gastrointest. Endosc. 52, 298–301 (2000).
Ikenberry, S. O. et al. Management of ingested foreign bodies and food impaction. Gastrointest. Endosc. 73, 1085–1091 (2011).
Kirschniak, A. et al. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest. Endosc. 66, 162–167 (2007).
Kirschniak, A. et al. Endoscopic treatment of gastric perforation caused by acute necrotizing pancreatitis using over-the-scope clips: a case report. Endoscopy 39, 1100–1102 (2007).
Raju, G. S. Endoscopic closure of gastrointestinal leaks. Am. J. Gastroenterol. 104, 1315–1320 (2009).
Kowalczyk, L. Algorithm for the management of endoscopic perforations: a quality improvement project. Am. J. Gastroenterol. 106, 1022–1027 (2011).
Mensink, P. B. et al. Complications of double balloon enteroscopy: a multicenter survey. Endoscopy 39, 613–615 (2007).
Möschler, O., May, A., Müller, M. K., Ell, C. & German DBE Study Group. Complications in and performance of double-balloon enteroscopy (DBE): results from a large prospective DBE database in Germany. Endoscopy 43, 484–489 (2011).
Kopacova, M., Tacheci, I., Rejchrt, S., Bartova, J. & Bures, J. Double balloon enteroscopy and acute pancreatitis. World J. Gastroenterol. 21, 2331–2340 (2010).
Karagiannis, S., Faiss, S. & Mavrogiannis, C. Capsule retention: a feared complication of wireless capsule endoscopy. Scand. J. Gastroenterol. 44, 1158–1165 (2009).
Atay, O. et al. Risk of capsule endoscope retention in pediatric patients: a large single-center experience and review of the literature. J. Pediatr. Gastroenterol. Nutr. 49, 196–201 (2009).
Thomson, A., Naidoo, P. & Crotty, B. Bowel preparation for colonoscopy: a randomized prospective trail comparing sodium phosphate and polyethylene glycol in a predominantly elderly population. J. Gastroenterol. Hepatol. 11, 103–107 (1996).
Garbay, J. R., Suc, B., Rotman, N., Fourtanier, G. & Escat, J. Multicentre study of surgical complications of colonoscopy. Br. J. Surg. 83, 42–44 (1996).
Lohsiriwat, V. Colonoscopic perforation: incidence, risk factors, management and outcome. World J. Gastroenterol. 16, 425–430 (2010).
Repici, A. & Tricerri, R. Endoscopic polypectomy: techniques, complications and follow-up. Tech. Coloproctol. 8, s283–s290 (2204).
Agresta, F., Michelet, I., Mainente, P. & Bedin, N. Laparoscopic management of colonoscopic perforations. Surg. Endosc. 14, 592–593 (2000).
Holmes, J. F. et al. Performance of helical computed tomography without oral contrast for the detection of gastrointestinal injuries. Ann. Emerg. Med. 43, 120–128 (2004).
Alfonso-Ballester, R., Lo Pez-Mozos, F., Mart-Obiol, R., Garcia-Botello, S. A. & Lledo-Matoses, S. Laparoscopic treatment of endoscopic sigmoid colon perforation: a case report and literature review. Surg. Laparosc. Endosc. Percutan. Tech. 16, 44–46 (2006).
Hansen, A. J., Tessier, D. J., Anderson, M. L. & Schlinkert, R. T. Laparoscopic repair of colonoscopic perforations: indications and guidelines. J. Gastrointest. Surg. 11, 655–659 (2007).
Albuquerque, W., Moreira, E., Arantes, V., Bittencourt, P. & Queiroz, F. Endoscopic repair of a large colonoscopic perforation with clips. Surg. Endosc. 22, 2072–2074 (2008).
Barbagallo, F. et al. Successful endoscopic repair of an unusual colonic perforation following polypectomy using an endoclip device. World J. Gastroenterol. 13, 2889–2891 (2007).
Kilic, A. & Kavic, S. M. Laparoscopic colotomy repair following colonoscopic polypectomy. JSLS 12, 93–96 (2008).
Makharia, G. K., Madan, K., Garg, P. K. & Tandon, R. K. Colonoscopic barotrauma treated by conservative management: role of high-flow oxygen inhalation. Endoscopy 34, 1010–1013 (2002).
Sileri, P., Del Vecchio Blanco, G., Benavoli, D. & Gaspari, A. L. Iatrogenic rectal perforation during operative colonoscopy: closure with endoluminal clips. JSLS 13, 69–72 (2009).
Donckier, V. & André, R. Treatment of colon endoscopic perforations. Acta Chir. Belg. 93, 60–62 (1993).
Avgerinos, D. V., Llaguna, O. H., Lo, A. Y. & Leitman, I. M. Evolving management of colonoscopic perforations. J. Gastrointest. Surg. 12, 1783–1789 (2008).
Trecca, A., Gaj, F. & Gagliardi, G. Our experience with endoscopic repair of large colonoscopic perforations and review of the literature. Tech. Coloproctol. 12, 315–321 (2008).
Parodi, A., Repici, A., Pedroni, A., Blanchi, S. & Conio, M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos). Gastrointest. Endosc. 72, 881–886 (2010).
Seebach, L., Bauerfeind, P. & Gubler, C. “Sparing the surgeon”: clinical experience with over-the-scope clips for gastrointestinal perforation. Endoscopy 42, 1108–1111 (2010).
Kirschniak, A., Subotova, N., Zieker, D., Königsrainer, A. & Kratt, T. The Over-The-Scope Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg. Endosc. 25, 2901–2905 (2011).
Orsoni, P. et al. Colonic perforation due to colonoscopy: a retrospective study of 48 cases. Endoscopy 29, 160–164 (1997).
Araghizadeh, F. Y., Timmcke, A. E., Opelka, F. G., Hicks, T. C. & Beck, D. E. Colonoscopic perforations. Dis. Colon Rectum 44, 713–716 (2001).
Cobb, W. S. et al. Colonoscopic perforations: incidence, management, and outcomes. Am. Surg. 70, 750–757 (2004).
Iqbal, C. W. et al. Surgical management and outcomes of 165 colonoscopic perforations from a single institution. Arch. Surg. 143, 701–706 (2008).
Waye, J. D., Lewis, B. S. & Yessayan, S. Colonoscopy: a prospective report of complications. J. Clin. Gastroenterol. 15, 347–351 (1992).
Gibbs, D. H. et al. Postpolypectomy colonic hemorrhage. Dis. Colon Rectum 39, 806–810 (1996).
Rosen, L., Bub, D. S., Reed, J. F. 3rd & Nastasee, S. A. Hemorrhage following colonoscopic polypectomy. Dis. Colon Rectum 36, 1126–1131 (1993).
Sorbi, D. et al. Postpolypectomy lower GI bleeding: descriptive analysis. Gastrointest. Endosc. 51, 690–696 (2000).
Shiffman, M. L., Farrel, M. T. & Yee, Y. S. Risk of bleeding after endoscopic biopsy or polypectomy in patients taking aspirin or other NSAIDS. Gastrointest. Endosc. 40, 458–462 (1994).
Hui, A. J. et al. Risk of colonoscopic polypectomy bleeding with anticoagulants and antiplatelet agents: analysis of 1657 cases. Gastrointest. Endosc. 59, 44–48 (2004).
Van Gossum, A., Cozzoli, A., Adler, M., Taton, G. & Cremer, M. Colonoscopic snare polypectomy: analysis of 1485 resections comparing two types of current. Gastrointest. Endosc. 38, 472–475 (1992).
Shioji, K. et al. Prophylactic clip application does not decrease delayed bleeding after colonoscopic polypectomy. Gastrointest. Endosc. 57, 691–694 (2003).
Lee, C. K. et al. Prophylactic argon plasma coagulation ablation does not decrease delayed postpolypectomy bleeding. Gastrointest. Endosc. 70, 353–361 (2009).
Ahishali, E. et al. Chemical colitis due to glutaraldehyde: case series and review of the literature. Dig. Dis. Sci. 54, 2541–2545 (2009).
Michetti, C. P., Smeltzer, E. & Fakhry, S. M. Splenic injury due to colonoscopy: analysis of the world literature, a new case report and recommendations for management. Am. Surg. 76, 1198–1204 (2010).
Cotton, P. B. et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest. Endosc. 37, 383–393 (1991).
Andriulli, A. et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am. J. Gastroenterol. 102, 1781–1788 (2007).
Williams, E. J. et al. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy 39, 793–801 (2007).
Wang, P. et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am. J. Gastroenterol. 104, 31–40 (2009).
Freeman, M. L. et al. Complications of endoscopic biliary sphincterotomy. N. Engl. J. Med. 335, 909–918 (1996).
Ferreira, L. E., Fatima, J. & Baron, T. H. Clinically significant delayed postsphincterotomy bleeding: a twelve year single center experience. Minerva Gastroenterol. Dietol. 53, 215–223 (2007).
Freeman, M. L. Adverse outcomes of endoscopic retrograde cholangiopancreatography. Rev. Gastroenterol. Disord. 2, 147–168 (2002).
Loperfido, S. et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest. Endosc. 48, 1–10 (1998).
Vandervoort, J. et al. Risk factors for complications after performance of ERCP. Gastrointest. Endosc. 56, 652–656 (2002).
Maldonado, M. E., Brady, P. G., Mamel, J. J. & Robinson, B. Incidence of pancreatitis in patients undergoing sphincter of Oddi manometry (SOM). Am. J. Gastroenterol. 94, 387–390 (1999).
Poon, R.T. et al. Intravenous bolus somatostatin after diagnostic cholangiopancreatography reduces the incidence of pancreatitis associated with therapeutic endoscopic retrograde cholangiopancreatography procedures: a randomised controlled trial. Gut 52, 1768–1773 (2003).
Vásconez, C. et al. Injection treatment of hemorrhage induced by endoscopic sphincterotomy. Endoscopy 30, 37–39 (1998).
Kuran, S. et al. Endoscopic sphincterotomy-induced hemorrhage: treatment with heat probe. Gastrointest. Endosc. 63, 506–511 (2006).
Baron, T. H., Norton, I. D. & Herman, L. Endoscopic hemoclip placement for post-sphincterotomy bleeding. Gastrointest. Endosc. 52, 662 (2000).
Mosca, S. & Galasso, G. Immediate and late bleeding after endoscopic sphincterotomy. Endoscopy 31, 278–279 (1999).
Kohler, A. et al. A new HF current generator with automatically controlled system (Endocut mode) for endoscopic sphincterotomy--preliminary experience. Endoscopy 30, 351–355 (1998).
Norton, I. D. et al. A randomized trial of endoscopic biliary sphincterotomy using pure-cut versus combined cut and coagulation waveforms. Clin. Gastroenterol. Hepatol. 3, 1029–1033 (2005).
Attasaranya, S. et al. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest. Endosc. 67, 1046–1052 (2008).
Stapfer, M. et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann. Surg. 232, 191–198 (2000).
Genzlinger, J. L. et al. Significance of retroperitoneal air after endoscopic retrograde cholangiopancreatography with sphincterotomy. Am. J. Gastroenterol. 94, 1267–1270 (1999).
Christensen, M., Matzen, P., Schulze, S. & Rosenberg, J. Complications of ERCP: a prospective study. Gastrointest. Endosc. 60, 721–731 (2004).
Avgerinos, D. V., Llaguna, O. H., Lo, A. Y., Voli, J. & Leitman, I. M. Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg. Endosc. 23, 833–838 (2009).
Heo, J. H. et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest. Endosc. 66, 720–726 (2007).
Motte, S. et al. Risk factors for septicemia following endoscopic biliary stenting. Gastroenterology 101, 1374–1381 (1991).
Byl, B. & Devière, J. Antibiotic prophylaxis before endoscopic retrograde cholangiopancreatography. Ann. Intern. Med. 126, 1001–1002 (1997).
Harris, A., Chan, A. C., Torres-Viera, C., Hammett, R. & Carr-Locke, D. Meta-analysis of antibiotic prophylaxis in endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy 31, 718–724 (1999).
Freeman, M. L. et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest. Endosc. 54, 425–434 (2001).
Masci, E. et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am. J. Gastroenterol. 96, 417–423 (2001).
Cotton, P. B. et al. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest. Endosc. 70, 80–88 (2009).
Dumonceau, J. M. et al. European Society of Gastrointestinal Endoscopy (ESGE) Guideline: prophylaxis of post-ERCP pancreatitis. Endoscopy 42, 503–515 (2010).
Elmunzer, B. J. et al. A meta-analysis of rectal NSAIDs in the prevention of post-ERCP pancreatitis. Gut 57, 1262–1267 (2008).
Cheung, J., Tsoi, K. K., Quan, W. L., Lau, J. Y. & Sung, J. J. Guidewire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. Gastrointest. Endosc. 70, 1211–1219 (2009).
Masci, E., Mariani, A., Curioni, S. & Testoni, P. A. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy 35, 830–834 (2003).
Singh, P. et al. Does prophylactic pancreatic stent placement reduce the risk of post-ERCP acute pancreatitis? A meta-analysis of controlled trials. Gastrointest. Endosc. 60, 544–550 (2004).
Mazaki, T., Masuda, H. & Takayama, T. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: a systematic review and meta-analysis. Endoscopy 42, 842–853 (2010).
Freeman, M. L., Overby, C. & Qi, D. Pancreatic stent insertion: consequences of failure and results of a modified technique to maximize success. Gastrointest. Endosc. 59, 8–14 (2004).
Kozarek, R. A. Pancreatic stents can induce ductal changes consistent with chronic pancreatitis. Gastrointest. Endosc. 36, 93–95 (1990).
Smith, M. T., Sherman, S., Ikenberry, S. O., Hawes, R. H. & Lehman, G. A. Alterations in pancreatic ductal morphology following polyethylene pancreatic stent therapy. Gastrointest. Endosc. 44, 268–275 (1996).
Chahal, P. et al. Short 5Fr vs long 3Fr pancreatic stents in patients at risk for post-endoscopic retrograde cholangiopancreatography pancreatitis. Clin. Gastroenterol. Hepatol. 7, 834–839 (2009).
Zolotarevsky, E. et al. Prophylactic 5-Fr pancreatic duct stents are superior to 3-Fr stents: a randomized controlled trial. Endoscopy 43, 325–330 (2011).
Tarnasky, P. R. et al. Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology 115, 1518–1524 (1998).
Harewood, G. C., Pochron, N. L. & Gostout, C. J. Prospective, randomized, controlled trial of prophylactic pancreatic stent placement for endoscopic snare excision of the duodenal ampulla. Gastrointest. Endosc. 62, 367–370 (2005).
Woods, K. E. & Willingham, F. F. Endoscopic retrograde cholangiopancreatography associated pancreatitis: A 15-year review. World J. Gastrointest. Endosc. 2, 165–178 (2010).
Deviere, J. Pancreatic stents. Gastrointest. Endosc. Clin. N. Am. 21, 499–510 (2011).
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to all aspects of this Review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Blero, D., Devière, J. Endoscopic complications—avoidance and management. Nat Rev Gastroenterol Hepatol 9, 162–172 (2012). https://doi.org/10.1038/nrgastro.2012.3
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2012.3
This article is cited by
-
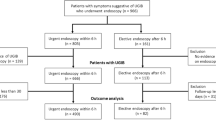
Prediction of esophagogastroduodenoscopy therapeutic usefulness for in-ICU suspected upper gastrointestinal bleeding: the SUGIBI score study
Annals of Intensive Care (2024)
-
Endoscopic transpapillary drainage in disconnected pancreatic duct syndrome after acute pancreatitis and trauma: long-term outcomes in 31 patients
BMC Gastroenterology (2019)
-
Choosing a Career in Advanced Endoscopy or General Gastroenterology
Digestive Diseases and Sciences (2017)
-
Upper gastrointestinal endoscopy: expected post-procedural findings and adverse events
Emergency Radiology (2016)
-
Management von Komplikationen bei endoskopischen Interventionen im oberen Gastrointestinaltrakt
Der Chirurg (2015)