Abstract
Purpose. The size-dependent deposition of microparticles and nanoparticles after oral administration to rats using an experimental model colitis was examined. Local delivery of an entrapped drug could reduce side effects and would be a distinct improvement compared with existing colon delivery devices.
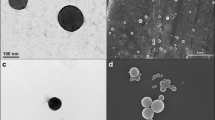
Methods. Ulcerative colitis was induced in Lewis rats with trinitrobenzenesulfonic acid. Fluorescent polystyrene particles with a size of 0.1, 1, or 10 μm were administered for 3 days. The animals then were sacrificed and their guts resected. Particle distribution in the colon was imaged by confocal laser scanning microscopy and quantified by fluorescence spectrophotometry.
Results. In the inflamed tissue, an increased adherence of particles was observed at the thicker mucus layer and in the ulcerated regions. A size dependency of the deposition was found, and an increased number of attached particles to the colon was determined compared with the control group. For 10-μm particles, only fair deposition was observed (control group: 1.4 ± 0.6%; colitis: 5.2 ± 3.8% of administered particle mass). One-micrometer particles showed higher binding (control group: 2.0 ± 0.8%; colitis: 9.1 ± 4.2%). Highest binding was found for 0.1-μm particles (control group: 2.2 ± 1.6%; colitis: 14.5 ± 6.3%). The ratio of colitis/control deposition increased with smaller particle sizes.
Conclusions. The use of submicron-sized carriers holds promise for the targeted delivery of drugs to the inflamed colonic mucosal areas in inflammatory bowel disease.
Similar content being viewed by others
REFERENCES
A. McLeod, D. R. Friend, and T. N. Tozer. Glucocorticoid-dextran conjugates as potential prodrugs colon-specific delivery: Hydrolysis in rat gastrointestinal tract contents. J. Pharm. Sci. 83:1284-1288 (1994).
R. Fedorak, B. Haeberlin, L. R. Empey, N. Cui, H. Nolen III, L. D. Jewell, and D. R. Friend. Colonic delivery of dexamethasone from a prodrug accelerates healing of colitis in rats without adrenal suppression. Gastroenterology 108:1688-1699 (1995).
U. Klotz. Clinical pharmacokinetics of sulphasalazine, its metabolites and other prodrugs of 5-aminosalicylic acid. Clin. Pharmacokinet. 10:285-302 (1985).
S. B. Hanauer. Medical therapy of ulcerative colitis. Lancet 342:412-417 (1993).
P. J. Watts and L. Illum. Colonic drug delivery. Drug Dev. Ind. Pharm. 23:893-913 (1997).
R. Kinget, W. Kalala, L. Vervoort, and G. van den Mooter. Colonic drug targeting. J. Drug Target. 6:129-149 (1998).
H. Tozaki, T. Fujita, J. Komoike, S. I. Kim, H. Terashima, S. Muranishi, S. Okabe, and A. Yamamoto. Colon-specific delivery of budenoside with azopolymer-coated pellets: Therapeutic effects of budenoside with a novel dosage form against 2,4,6-trinitrobenzene sulphonic acid-induced colitis in rats. J. Pharm. Pharmacol. 51:257-261 (1999).
F. H. Hardy, S. S. Davis, R. Khosla, and C. S. Robertson. Gastrointestinal transit of small tablets in patients with ulcerative colitis. Int. J. Pharm. 48:79-82 (1988).
P. J. Watts, L. Barrow, K. P. Steed, C. G. Wilson, R. C. Spiller, C. D. Melia, and M. C. Davies. The transit rate of different-sized model dosage forms through the human colon and the effects of a lactulose-induced catharsis. Int. J. Pharm. 87:215-221 (1992).
M. Rodriguez, J. L. Vila-Jato, and D. Torres. Design of a new multiparticulate system for potential site specific and controlled drug delivery to the colonic region. J. Control. Release 55:67-77 (1998).
H. Nakase, K. Okazaki, Y. Tabata, S. Uose, M. Ohana, K. Uchida, Y. Matsushima, C. Kawanami, C. Oshima, Y. Ikada, and T. Chiba. Development of an oral drug delivery system targeting immune-regulating cells in experimental inflammatory bowel disease: A new therapeutic strategy. J. Pharmacol. Exp. Ther. 292:15-21 (2000).
M. C. Allison, S. Cornwall, L. W. Poulter, A. P. Dhillon, and R. E. Pounder. Macrophage heterogeneity in normal colonic mucosa and in inflammatory bowel disease. Gut 29:1531-1538 (1988).
C. A. Seldenrijk, H. A. Drexhage, and S. G. M. Meuwissen. Dentritic cells and scavanger macrophage in chronic inflammatory bowel disease. Gut 30:484-491 (1989).
C. S. Probert, A. Chott, J. R. Turner, L. J. Saubermann, A. C. Stevens, K. Bodinaku, C. O. Elson, S. P. Balk, and R. S. Blumberg. Persistent clonal expansion of peripheral blood CD4+ lymphocytes in chronic inflammatory bowel disease. J. Immunol. 157:3183-3191 (1996).
Y. Tabata, Y. Inoue, and Y. Ikada. Size effect on systemic and mucosal immune responses induced by oral administration of biodegradable microspheres. Vaccine 14:1677-1685 (1996).
H. Pinto-Alphandary, O. Balland, M. Laurent, A. Andremont, F. Puisieux, and P. Couvreur. Intracellular visualization of ampicillin-loaded nanoparticles in peritoneal macrophages infected in vitro with Salmonella typhimurium. Pharm. Res. 11:38-46 (1994).
J. Stein, J. Ries, and K. E. Barrett. Disruption of intestinal barrier function associated with experimental colitis: Possible role of mast cells. Am. J. Physiol. 274:G203-G209 (1998).
G. Yue, F. F. Sun, C. Dunn, K. Yin, and P. Y. K. Wong. The 21-aminosteroid tirilazad mesylate can ameliorate inflammatory bowel disease in rats. J. Pharmacol. Exp. Ther. 276:265-270 (1996).
J. E. Krawisz, P. Sharon, and W. F. Stenson. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Gastroenterology 87:1344-1350 (1984).
T. Yamada, S. Marshall, R. D. Specian, and M. B. Grisham. A comparative analysis of two models of colitis in rats. Gastroenterology 102:1524-1534 (1992).
G. P. Morris, P. L. Beck, M. S. Herridge, W. T. Depew, M. R. Szewczuk, and J. L. Wallace. Hapten-induced model of chronic inflammation and ulceration in the rat colon. Gastroeneterology 96:795-803 (1989).
M. P. Desai, V. Labhasetwar, G. L. Amidon, and R. J. Levy. Gastrointestinal uptake of biodegradable microparticles: Effects of particle size. Pharm. Res. 13:1838-1845 (1996).
P. U. Jani, G. W. Halbert, J. Langridge, and A. T. Florence. The uptake and translocation of latex nanospheres and microspheres after oral administration to rats. J. Pharm. Pharmacol. 41:809-821 (1989).
P. U. Jani, G. W. Halbert, J. Langridge, and A. T. Florence. Nanoparticle uptake by the ratgastrointestinal mucosa: Quantitation and particle size dependency. J. Pharm. Pharmacol. 42:821-826 (1990).
S. Sakuma, R. Sudo, N. Suzuki, H. Kikuchi, M. Akashi, and M. Hayashi. Mucoadhesion of polystyrene nanoparticles having surface hydrophilic polymeric chains in the gastrointestinal tract. Int. J. Pharm. 177:161-172 (1999).
B. Tirosh, and A. Rubinstein. Migration of adhesive and nonadhesive particles in the rat intestine under altered mucus secretion conditions. J. Pharm. Sci. 87:453-456 (1998).
Y. Tabata and Y. Ikada. Phagocytosis of polymer microspheres by macrophages. Adv. Polymer Sci. 94:107-141 (1990).
C. O. Elson, R. B. Sartor, G. S. Tennyson, and R. H. Riddell. Experimental models of inflammatory bowel disease. Gastroenterology 109:1344-1367 (1995).
L. Manil, J. C. Davin, C. Duchenne, C. Kubiak, J. Foidart, P. Couvreur, and P. Mahieu. Uptake of nanoparticles by rat glomerular mesangial cells in vivo and in vitro. Pharm. Res. 11:1160-1165 (1994).
R. Nagashima. Mechanisms of action of sulcrafate. J. Clin. Gastroenterol. 3:117-127 (1981).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lamprecht, A., Schäfer, U. & Lehr, CM. Size-Dependent Bioadhesion of Micro- and Nanoparticulate Carriers to the Inflamed Colonic Mucosa. Pharm Res 18, 788–793 (2001). https://doi.org/10.1023/A:1011032328064
Issue Date:
DOI: https://doi.org/10.1023/A:1011032328064