Abstract
Purpose
The aim of this study was to assess clinical features and therapeutic outcomes in patients with clinically non-functioning pituitary macroadenomas (NFPMAs).
Method
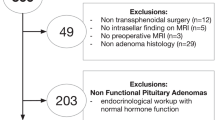
This is a retrospective cohort study of NFPMA patients treated surgically and followed periodically between 2015 and 2017 in a tertiary care center in Iran. Descriptive analysis was performed applying appropriate tests. Binary logistic regression models were used to determine the predictive factors for subtotal tumor resection (STR) and hormonal recovery. Data were analyzed by Stata software.
Result
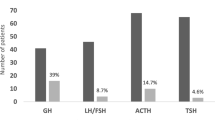
A total of 71 patients with a mean age of 50.6 ± 1.4 years were studied. The mean diameter of the adenoma was 26.8 ± 1.1 mm. The most frequent symptoms were headache (85.75%), visual field defect (VFD) (78.3%), and hypogonadal symptoms (40.3%). Gross total resection (GTR) was achieved in 45.1%. Preoperative hypopituitarism was observed in 50.7% of patients. Recovery of at least one axis occurred in 36.1% of the patients suffering from hypopituitarism preoperatively, while new-onset postoperative hormonal deficiency appeared in 14.3% of patients. Multivariate analyses showing preoperative tumor size (OR = 38.2; P = 0.008) and cavernous sinus extension (OR = 13.4; P = 0.020) were predictors of STR. Moreover, hormonal recovery was observed not to be related to age, gender, tumor size, or the extent of tumor resection.
Conclusions
Tumor size and cavernous sinus extension are the main predictors for STR. Notably, recovery of the gonadal axis in a large proportion of patients supports the surgical resection of NFPAM in patients suffering from gonadal deficiency, even in the absence of VFD.

Similar content being viewed by others
References
Losa M, Mortini P, Barzaghi R et al (2008) Early results of surgery in patients with nonfunctioning pituitary adenoma and analysis of the risk of tumor recurrence. J Neurosurg 108:525–532. https://doi.org/10.3171/JNS/2008/108/3/0525
Woollons AC, Hunn MK, Rajapakse YR et al (2000) Non-functioning pituitary adenomas: indications for postoperative radiotherapy. Clin Endocrinol 53:713–717. https://doi.org/10.1046/j.1365-2265.2000.01153.x
Greenman Y, Ouaknine G, Veshchev I, Reider-Groswasser II, Segev Y, Stern N (2003) Postoperative surveillance of clinically nonfunctioning pituitary macroadenomas: markers of tumour quiescence and regrowth. Clin Endocrinol 58:763–769. https://doi.org/10.1046/j.1365-2265.2003.01784.x
Littley MD, Shalet SM, Beardwell CG, Ahmed SR, Applegate G, Sutton ML (1989) Hypopituitarism following external radiotherapy for pituitary tumors in adults. Q J Med 70:145–160. https://doi.org/10.1093/oxfordjournals.qjmed.a068308
Minniti G, Traish D, Ashley S, Gonsalves A, Brada M (2005) Risk of second brain tumor after conservative surgery and radiotherapy for pituitary adenoma: update after an additional 10 years. J Clin Endocrinol Metab 90:800–804. https://doi.org/10.1210/jc.2004-1152
McDowell BD, Wallace RB, Carnahan RM, Chrischilles EA, Lynch CF, Schlechte JA (2011) Demographic differences in incidence for pituitary adenoma. Pituitary 14:23–30. https://doi.org/10.1007/s11102-010-0253-4
Maile EJ, Barnes I, Finlayson AE, Sayeed S, Ali R (2016) Nervous system and intracranial tumour incidence by ethnicity in England 2001–2007: a descriptive epidemiological study. PLoS One 11:e0154347. https://doi.org/10.1371/journal.pone.0154347
Cimpean AM, Melnic E, Bălinişteanu B et al (2015) Geographic-related differences of pituitary adenomas hormone profile: analysis of two groups coming from Southeastern and Eastern Europe. Int J Endocrinol:192094. https://doi.org/10.1155/2015/192094
Khamseh ME, Mohajeri Tehrani MR, Mousavi Z et al (2017) Iran pituitary tumor registry: description of the program and initial results. Arch Iran Med 20:746–751
Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD et al (2016) Diagnosis and treatment of primary adrenal insufficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 101(2):364–389. https://doi.org/10.1210/jc.2015-1710
Ferrante E, Ferraroni M, Castrignano T et al (2006) Non-functioning pituitary adenoma database: a useful resource to improve the clinical management of pituitary tumors. Eur J Endocrinol 155:823–829. https://doi.org/10.1530/eje.1.02298
Erdem Yildirim A, Sahinoglu M, Ekici I et al (2016) Nonfunctioning pituitary adenomas are really clinically nonfunctioning? Clinical and Endocrinological symptoms and outcomes with endoscopic endonasal treatment. World Neurosurg 85:185–192. https://doi.org/10.1016/j.wneu.2015.08.073
Ramakrishnan VR, Suh JD, Lee JY, O'Malley BW Jr, Grady MS, Palmer JN (2013) Sphenoid sinus anatomy and suprasellar extension of pituitary tumors. J Neurosurg 119:669–674. https://doi.org/10.3171/2013.3.JNS122113
Molitch ME (2017) Diagnosis and treatment of pituitary adenomas a review. JAMA 317:516–524. https://doi.org/10.1001/jama.2016.19699
Schaller B (2003) Gender-related differences in non-functioning pituitary adenoma. Neuro Endocrinol Lett 24:425–430. https://doi.org/10.1023/A:1025329900839
Caputo C, Sutherland T, Farish S, McNeill P, Ng KW, Inder WJ (2012) Gender differences in presentation and outcome of nonfunctioning pituitary macroadenomas. Clin Endocrinol 78:564–570. https://doi.org/10.1111/cen.12009
Iglesias P, Arcano K, Triviño V et al (2017) Non-functioning pituitary adenoma underwent surgery: a multicenter retrospective study over the last four decades (1977–2015). Eur J Intern Med 41:62–67. https://doi.org/10.1016/j.ejim.2017.03.023
Gondim JA, Schops M, de Almeida JP et al (2010) Endoscopic endonasal transsphenoidal surgery: surgical results of 228 pituitary adenomas treated in a pituitary center. Pituitary 13:68–77. https://doi.org/10.1007/s11102-009-0195-x
Kim JH, Lee JH, Hong AR, Kim YJ, Kim YH (2018) Endoscopic transsphenoidal surgery outcomes in 331 nonfunctioning pituitary adenoma cases after a single surgeon learning curve. World Neurosurg 109:e409–e416. https://doi.org/10.1016/j.wneu.2017.09.194
Almutairi R, Zaidi HA, Cote DJ et al (2017) Comparison of gross tumor resection rate between endoscopic transsphenoidal surgery versus microscopic transsphenoidal surgery for patients with pituitary adenomas: a meta-analysis. J Neurol Surg B 78:S1–S156. https://doi.org/10.1055/s-0037-1600713
Tampourlou M, Ntali G, Ahmed S et al (2017) Outcome of non-functioning pituitary adenomas that regrow after primary treatment: a study from two large UK centers. J Clin Endocrinol Metab 102:1889–1897. https://doi.org/10.1210/jc.2016-4061
O’Sullivan EP, Woods C, Glynn N et al (2009) The natural history of surgically treated but radiotherapy-naïve nonfunctioning pituitary adenomas. Clin Endocrinol (Oxf) 71:709–714. https://doi.org/10.1111/j.1365-2265.2009.03583.x
Watts AK, Easwaran A, McNeill P, Wang YY, Inder WJ, Caputo C (2017) Younger age is a risk factor for regrowth and recurrence of nonfunctioning pituitary macroadenomas: results from a single Australian Centre. Clin Endocrinol (Oxf) 87:264–271. https://doi.org/10.1111/cen.13365
Langlois F, Lim DST, Yedinak CG et al (2018) Predictors of silent corticotroph adenoma recurrence; a large retrospective single center study and systematic literature review. Pituitary 21:32–40. https://doi.org/10.1007/s11102-017-0844-4
Sadik ZHA, Voormolen EHJ, Depauw PRAM et al (2017) Treatment of nonfunctional pituitary adenoma postoperative remnants: adjuvant or delayed gamma knife radiosurgery? World Neurosurg 100:361–368. https://doi.org/10.1016/j.wneu.2017.01.028
Ammirati M, WeiIvan L, Ciric I (2013) Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 84:843–849. https://doi.org/10.1136/jnnp-2012-303194
Karppinen A, Kivipelto L, Vehkavaara S et al (2015) Transition from microscopic to endoscopic transsphenoidal surgery for nonfunctional pituitary adenomas. World Neurosurg 84:48–57. https://doi.org/10.1016/j.wneu.2015.02.024
Singh H, Essayed WI, Cohen-Gadol A, Zada G, Schwartz TH (2016) Resection of pituitary tumors: endoscopic versus microscopic. J Neuro-Oncol 130:309–317. https://doi.org/10.1007/s11060-016-2124-y
Vargas G, Gonzalez B, Ramirez C et al (2015) Clinical characteristics and treatment outcome of 485 patients with nonfunctioning pituitary macroadenomas. Int J Endocrinol 756069:7. https://doi.org/10.1155/2015/756069
Nomikos P, Ladar C, Fahlbusch R, Buchfelder M (2004) Impact of primary surgery on pituitary function in patients with non-functioning pituitary adenomas – a study on 721 patients. Acta Neurochir (Wien) 146:27–35. https://doi.org/10.1007/s00701-003-0174-3
Fleseriu M, Bodach ME, Tumialan LM et al (2016) Pretreatment endocrine evaluation of patients with nonfunctioning pituitary adenomas. Neurosurgery 79:E527–E529. https://doi.org/10.1227/NEU.0000000000001387
Laws ER Jr, Iuliano SL, Cote DJ, Woodmansee W, Hsu L, Cho CH (2016) A benchmark for preservation of normal pituitary function after endoscopic transsphenoidal surgery for pituitary macroadenomas. World Neurosurg 91:371–375. https://doi.org/10.1016/j.wneu.2016.04.059
Arafah BM (1986) Reversible hypopituitarism in patients with large nonfunctioning pituitary adenomas. J Clin Endocrinol Metab 62:1173–1179. https://doi.org/10.1210/jcem-62-6-1173
Jahangiri A, Wagner JR, Han SW et al (2015) Improved versus worsened endocrine function after transsphenoidal surgery for nonfunctional pituitary adenomas: rate time course and radiological analysis. J Neurosurg 124:589–595. https://doi.org/10.3171/2015.1.JNS141543
Mercado M, Melgar V, Salame L, Cuenca D (2017) Clinically non-functioning pituitary adenomas: pathogenic diagnostic and therapeutic aspects. Endocrinol Diab Nutr 64:384–395. https://doi.org/10.1016/j.endinu.201705.009
Fatemi N, Dusick JR, Mattozo C et al (2008) Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63:709–718. https://doi.org/10.1227/01.NEU.0000325725.77132.90
Freda PU, Beckers AM, Katznelson L et al (2011) Pituitary incidentaloma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96:894–904. https://doi.org/10.1210/jc.2010-1048
Acknowledgements
We greatly appreciate the contribution of the staff of the Endocrine Research Center at Iran University of Medical Sciences (IUMS).
Funding
This study was funded and supported by Iran University of Medical Sciences (grant number 9511330002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the ethics committee of Iran University of Medical Sciences (approval number: IR.IUMS.FMD.REC 1396.9511330002).
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
We extracted data from a registry anonymously. Thus, inform consent was not necessary.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Najmaldin, A., Malek, M., Madani, N.H. et al. Non-functioning pituitary macroadenoma: surgical outcomes, tumor regrowth, and alterations in pituitary function—3-year experience from the Iranian Pituitary Tumor Registry. Hormones 18, 197–205 (2019). https://doi.org/10.1007/s42000-019-00109-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-019-00109-5