Abstract
Purpose of review
To review the current evidence for the management of mental disorders for youth with rheumatologic diseases, and elucidate gaps in knowledge requiring further investigation to improve management of mental health conditions for these patients.
Recent findings
Depression and anxiety are common in youth with pediatric rheumatologic diseases and are associated with poor adherence, quality of life, and long-term outcomes. They have a complex etiology and require consideration of overall disease management as well as contributing psychosocial factors. Increasing evidence indicates that current screening strategies fail to fully support this patient population and that many patients with mental health problems go untreated.
Summary
Effective strategies to approach mental health in pediatric rheumatology patients are likely those that incorporate both behavioral and pharmacological therapies, and include families and social support. Preliminary evidence shows that adopting screening practices in pediatric rheumatology clinics will improve detection of mental disorders and is acceptable to patients and families. Broad mental health screening strategies should be considered for youth with rheumatologic diseases. Further research is necessary to better understand which treatments are most effective for depression, anxiety, and other forms of mental disorders observed in pediatric rheumatology.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bernstein CM, Stockwell MS, Gallagher MP, Rosenthal SL, Soren K. Mental health issues in adolescents and young adults with type 1 diabetes: prevalence and impact on glycemic control. Clin Pediatr (Phila). 2013;52(1):10–5. https://doi.org/10.1177/0009922812459950.
Bitsko MJ, Everhart RS, Rubin BK. The adolescent with asthma. Paediatr Respir Rev. 2014;15(2):146–53. https://doi.org/10.1016/j.prrv.2013.07.003.
Calsbeek H, Rijken M, Bekkers MJ, Dekker J, van Berge Henegouwen GP. School and leisure activities in adolescents and young adults with chronic digestive disorders: impact of burden of disease. Int J Behav Med. 2006;13(2):121–30. https://doi.org/10.1207/s15327558ijbm1302_3.
Harrington R, Fudge H, Rutter M, Pickles A, Hill J. Adult outcomes of childhood and adolescent depression I. Psychiatric status. Arch Gen Psychiatry. 1990;47(5):465–73.
Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60(7):709–17. https://doi.org/10.1001/archpsyc.60.7.709.
Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M. The Maudsley long-term follow-up of child and adolescent depression. 2. Suicidality, criminality and social dysfunction in adulthood. Br J Psychiatry J Ment Sci. 2001;179:218–23.
Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59(3):225–31.
Currie J. Health disparities and gaps in school readiness. Future Child. 2005;15(1):117–38.
Currie J, Stabile M. Child mental health and human capital accumulation: the case of ADHD. J Health Econ. 2006;25(6):1094–118. https://doi.org/10.1016/j.jhealeco.2006.03.001.
Knight A, Weiss P, Morales K, Gerdes M, Gutstein A, Vickery M, et al. Depression and anxiety and their association with healthcare utilization in pediatric lupus and mixed connective tissue disease patients: a cross-sectional study. Pediatric Rheumatol Online J. 2014;12:42. https://doi.org/10.1186/1546-0096-12-42.
• Krause ML, Zamora-Legoff JA, Crowson CS, Muskardin TW, Mason T, Matteson EL. Population-based study of outcomes of patients with juvenile idiopathic arthritis (JIA) compared to non-JIA subjects. Semin Arthritis Rheum. 2017;46(4):439–43. https://doi.org/10.1016/j.semarthrit.2016.07.003. Analysis of medical records of age and sex-matched children with and without JIA showed that the incident depression in children with was higher than in controls.
Duzceker Y, Kanbur NO, Demirkaya E, Derman O, Moorthy LN, Ozen S. Quality of life measures and psychiatric symptoms in adolescents with systemic lupus erythematosus and familial Mediterranean fever. Int J Adolesc Med Health. 2014;26(4):541–9. https://doi.org/10.1515/ijamh-2013-0332.
Apaz MT, Saad-Magalhaes C, Pistorio A, Ravelli A, de Oliveira SJ, Marcantoni MB, et al. Health-related quality of life of patients with juvenile dermatomyositis: results from the Pediatric Rheumatology International Trials Organisation multinational quality of life cohort study. Arthritis Rheum. 2009;61(4):509–17. https://doi.org/10.1002/art.24343.
Sanner H, Gran JT, Sjaastad I, Flato B. Cumulative organ damage and prognostic factors in juvenile dermatomyositis: a cross-sectional study median 16.8 years after symptom onset. Rheumatology (Oxford). 2009;48(12):1541–7. https://doi.org/10.1093/rheumatology/kep302.
Ruperto N, Buratti S, Duarte-Salazar C, Pistorio A, Reiff A, Bernstein B, et al. Health-related quality of life in juvenile-onset systemic lupus erythematosus and its relationship to disease activity and damage. Arthritis Rheum. 2004;51(3):458–64. https://doi.org/10.1002/art.20412.
Lim LS, Lefebvre A, Benseler S, Peralta M, Silverman ED. Psychiatric illness of systemic lupus erythematosus in childhood: spectrum of clinically important manifestations. J Rheumatol. 2013;40(4):506–12. https://doi.org/10.3899/jrheum.120675.
Knight A, Weiss P, Morales K, Gerdes M, Rearson M, Vickery M, et al. Identifying differences in risk factors for depression and anxiety in pediatric chronic disease: a matched cross-sectional study of youth with lupus/mixed connective tissue disease and their peers with diabetes. J Pediatr. 2015;167(6):1397–403.e1. https://doi.org/10.1016/j.jpeds.2015.07.048.
•• Knight AM, Trupin L, Katz P, Yelin E, Lawson EF. Depression risk in young adults with childhood- and adult-onset lupus: 12 years of follow-up. Arthritis Care Res (Hoboken). 2017; https://doi.org/10.1002/acr.23290. Findings indicate that among young adult patients, those with childhood-onset SLE are more likely to have repeated depressive episodes than those with adult-onset.
Force USPST. Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2009;123(4):1223–8. https://doi.org/10.1542/peds.2008-2381.
Committee On P, Ambulatory M, Bright Futures Periodicity Schedule W. 2017 Recommendations for preventive pediatric health care. Pediatrics. 139(4). https://doi.org/10.1542/peds.2017-0254.
Gortmaker SL, Walker DK, Weitzman M, Sobol AM. Chronic conditions, socioeconomic risks, and behavioral problems in children and adolescents. Pediatrics. 1990;85(3):267–76.
Newacheck PW, McManus MA, Fox HB. Prevalence and impact of chronic illness among adolescents. Am J Dis Child. 1991;145(12):1367–73.
Abou Abbas O, AlBuhairan F. Predictors of adolescents’ mental health problems in Saudi Arabia: findings from the Jeeluna(R) national study. Child Adolesc Psychiatry Ment Health. 2017;11:52. https://doi.org/10.1186/s13034-017-0188-x.
Pinquart M, Shen Y. Depressive symptoms in children and adolescents with chronic physical illness: an updated meta-analysis. J Pediatr Psychol. 2011;36(4):375–84. https://doi.org/10.1093/jpepsy/jsq104.
Louthrenoo O, Krairojananan J, Chartapisak W, Opastirakul S. Psychosocial functioning of children with systemic lupus erythematosus. J Paediatr Child Health. 2012;48(12):1091–4. https://doi.org/10.1111/j.1440-1754.2012.02499.x.
Tarakci E, Yeldan I, Kaya Mutlu E, Baydogan SN, Kasapcopur O. The relationship between physical activity level, anxiety, depression, and functional ability in children and adolescents with juvenile idiopathic arthritis. Clin Rheumatol. 2011;30(11):1415–20. https://doi.org/10.1007/s10067-011-1832-0.
Noll RB, Kozlowski K, Gerhardt C, Vannatta K, Taylor J, Passo M. Social, emotional, and behavioral functioning of children with juvenile rheumatoid arthritis. Arthritis Rheum. 2000;43(6):1387–96. https://doi.org/10.1002/1529-0131(200006)43:6 < 1387::AID-ANR24 > 3.0.CO;2-C.
Postal M, Pelicari KO, Sinicato NA, Marini R, Costallat LT, Appenzeller S. Th1/Th2 cytokine profile in childhood-onset systemic lupus erythematosus. Cytokine. 2013;61(3):785–91. https://doi.org/10.1016/j.cyto.2012.11.023.
Ji L, Lili S, Jing W, Yanyan H, Min W, Juan X, et al. Appearance concern and depression in adolescent girls with systemic lupus erythematous. Clin Rheumatol. 2012;31(12):1671–5. https://doi.org/10.1007/s10067-012-2071-8.
Hoff AL, Palermo TM, Schluchter M, Zebracki K, Drotar D. Longitudinal relationships of depressive symptoms to pain intensity and functional disability among children with disease-related pain. J Pediatr Psychol. 2006;31(10):1046–56. https://doi.org/10.1093/jpepsy/jsj076.
Mullick MS, Nahar JS, Haq SA. Psychiatric morbidity, stressors, impact, and burden in juvenile idiopathic arthritis. J Health Popul Nutr. 2005;23(2):142–9.
• Jones JT, Cunningham N, Kashikar-Zuck S, Brunner HI. Pain, fatigue, and psychological impact on health-related quality of life in childhood-onset lupus. Arthritis Care Res (Hoboken). 2016;68(1):73–80. https://doi.org/10.1002/acr.22650. Anxiety and depression correlate with overall health-related quality of life. Anxiety, along with pain, and fatigue impact health-related quality of life more than disease activity.
•• Knight AM, Xie M, Mandell DS. Disparities in psychiatric diagnosis and treatment for youth with systemic lupus erythematosus: analysis of a National US Medicaid Sample. J Rheumatol. 2016;43(7):1427–33. https://doi.org/10.3899/jrheum.150967. The largest study to date of youth with SLE regarding mental health outcomes: 19% of Medicaid enrolled youth with lupus diagnosed with depression. Compared to white youth, African Americans are less likely to be diagnosed with depression or anxiety, or to be prescribed anxiolytics.
Yorgin P, Lazarow E, Sheets R. Patient health questionnaire-9 utilization for the detection of depression in adolescents and young adults with lupus nephritis. Arthritis Rheum. 2017;69.
Schanberg LE, Anthony KK, Gil KM, Maurin EC. Daily pain and symptoms in children with polyarticular arthritis. Arthritis Rheum. 2003;48(5):1390–7. https://doi.org/10.1002/art.10986.
Packham JC, Hall MA, Pimm TJ. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: predictive factors for mood and pain. Rheum (Oxford, England). 2002;41(12):1444–9.
Donnelly C, Cunningham N, Jones JT, Ji L, Brunner HI, Kashikar-Zuck S. Fatigue and depression predict reduced health-related quality of life in childhood-onset lupus. Lupus. 2017;961203317716317. https://doi.org/10.1177/0961203317716317.
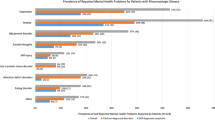
•• Knight AM, Vickery ME, Muscal E, Davis AM, Harris JG, Soybilgic A, et al. Identifying targets for improving mental healthcare of adolescents with systemic lupus erythematosus: perspectives from Pediatric Rheumatology Clinicians in the United States and Canada. J Rheumatol. 2016;43(6):1136–45. https://doi.org/10.3899/jrheum.151228. Survey that described practice behaviors of pediatric rheumatologist regarding addressing mental health in patients, showing that few routinely screen for depression and anxiety, though the majority believe it is important.
Andermann A, Blancquaert I, Beauchamp S, Dery V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull World Health Organ. 2008;86(4):317–9.
Davis AM, Graham TB, Zhu Y, McPheeters ML. Cross-sectional analysis of depression and medication non-adherence in childhood-onset systemic lupus erythematosus. Arthritis Rheum. 2017;69:44–6. https://doi.org/10.1002/art.v69.S4.
Knight AM, Davis AM, Klein-Gitelman MS, Cidav Z, Mandell D. The impact of psychiatric comorbidity on health care utilization for youth with systemic lupus erythematosus. Arthritis Rheum. 2017;69
Aasland A, Flato B, Vandvik IH. Psychosocial outcome in juvenile chronic arthritis: a nine-year follow-up. Clin Exp Rheum. 1997;15(5):561–8.
David J, Cooper C, Hickey L, Lloyd J, Dore C, McCullough C, et al. The functional and psychological outcomes of juvenile chronic arthritis in young adulthood. Br J Rheum. 1994;33(9):876–81.
Foster HE, Marshall N, Myers A, Dunkley P, Griffiths ID. Outcome in adults with juvenile idiopathic arthritis: a quality of life study. Arthritis Rheum. 2003;48(3):767–75. https://doi.org/10.1002/art.10863.
Tollisen A, Selvaag AM, Aulie HA, Lilleby V, Aasland A, Lerdal A et al. Physical functioning, pain and health-related quality of life in adults with juvenile idiopathic arthritis: a longitudinal 30-year follow-up study. Arthritis Care Res (Hoboken). 2017. https://doi.org/10.1002/acr.23327.
Ramnath RAS, Groot N, Kaynak A, Bijl M, Dolhain RJEM, Teng YKO, et al. Adult outcomes in a large cohort of childhood-onset SLE patients: coping and resilience in relation to health-related quality of life-the CHILL-NL study. Pediatric Rheum. 2017;15:77. https://doi.org/10.1186/s12969-017-0185-x.
Tollisen A, Sanner H, Flato B, Wahl AK. Quality of life in adults with juvenile-onset dermatomyositis: a case-control study. Arthritis Care Res (Hoboken). 2012;64(7):1020–7. https://doi.org/10.1002/acr.21637.
Arkela-Kautiainen M, Haapasaari J, Kautiainen H, Vilkkumaa I, Malkia E, Leirisalo-Repo M. Favourable social functioning and health related quality of life of patients with JIA in early adulthood. Ann Rheum Dis. 2005;64(6):875–80. https://doi.org/10.1136/ard.2004.026591.
Peterson LS, Mason T, Nelson AM, O’Fallon WM, Gabriel SE. Psychosocial outcomes and health status of adults who have had juvenile rheumatoid arthritis: a controlled, population-based study. Arthritis Rheum. 1997;40(12):2235–40. https://doi.org/10.1002/1529-0131(199712)40:12<2235::AID-ART18>3.0.CO;2-F.
Yu HH, Lee JH, Wang LC, Yang YH, Chiang BL. Neuropsychiatric manifestations in pediatric systemic lupus erythematosus: a 20-year study. Lupus. 2006;15(10):651–7. https://doi.org/10.1177/0961203306070990.
Steinlin MI, Blaser SI, Gilday DL, Eddy AA, Logan WJ, Laxer RM, et al. Neurologic manifestations of pediatric systemic lupus erythematosus. Pediatr Neurol. 1995;13(3):191–7.
Beale IL. Scholarly literature review: efficacy of psychological interventions for pediatric chronic illnesses. J Pediatr Psychol. 2006;31(5):437–51. https://doi.org/10.1093/jpepsy/jsj079.
Wesselhoeft R, Sorensen MJ, Heiervang ER, Bilenberg N. Subthreshold depression in children and adolescents—a systematic review. J Affect Disord. 2013;151(1):7–22. https://doi.org/10.1016/j.jad.2013.06.010.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Kovacs M. The Children’s Depression, Inventory (CDI). Psychopharmacol Bull. 1985;21(4):995–8.
Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38(10):1230–6. https://doi.org/10.1097/00004583-199,910,000-00011.
March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(4):554–65. https://doi.org/10.1097/00004583-199,704,000-00019.
Achenbach TM, Verhulst FC, Baron GD, Althaus M. A comparison of syndromes derived from the Child Behavior Checklist for American and Dutch boys aged 6–11 and 12–16. J Child Psychol Psychiatry. 1987;28(3):437–53.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. https://doi.org/10.1001/archinte.166.10.1092.
Jellinek MS, Murphy JM, Robinson J, Feins A, Lamb S, Fenton T. Pediatric symptom checklist: screening school-age children for psychosocial dysfunction. J Pediatr. 1988;112(2):201–9.
Faulstich ME, Carey MP, Ruggiero L, Enyart P, Gresham F. Assessment of depression in childhood and adolescence: an evaluation of the Center for Epidemiological Studies Depression Scale for Children (CES-DC). Am J Psychiatr. 1986;143(8):1024–7. https://doi.org/10.1176/ajp.143.8.1024.
Brandon TG, Becker BD, Bevans KB, Weiss PF. Patient-reported outcomes measurement information system tools for collecting patient-reported outcomes in children with juvenile arthritis. Arthritis Care Res. 2017;69(3):393–402. https://doi.org/10.1002/acr.22937.
Choi SW, Schalet B, Cook KF, Cella D. Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychol Assess. 2014;26(2):513–27. https://doi.org/10.1037/a0035768.
Kim J, Chung H, Askew RL, Park R, Jones SM, Cook KF, et al. Translating CESD-20 and PHQ-9 Scores to PROMIS Depression. Assessment. 2017;24(3):300–7. https://doi.org/10.1177/1073191115607042.
Julian LJ, Gregorich SE, Tonner C, Yazdany J, Trupin L, Criswell LA, et al. Using the Center for Epidemiologic Studies Depression Scale to screen for depression in systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2011;63(6):884–90. https://doi.org/10.1002/acr.20447.
Covic T, Pallant JF, Conaghan PG, Tennant A. A longitudinal evaluation of the Center for Epidemiologic Studies-Depression scale (CES-D) in a rheumatoid arthritis population using Rasch analysis. Health Qual Life Outcomes. 2007;5:41. https://doi.org/10.1186/1477-7525-5-41.
Kohut SA, Williams TS, Jayanthikumar J, Landolt-Marticorena C, Lefebvre A, Silverman E, et al. Depressive symptoms are prevalent in childhood-onset systemic lupus erythematosus (cSLE). Lupus. 2013;22(7):712–20. https://doi.org/10.1177/0961203313488840.
Shaw KL, Southwood TR, McDonagh JE. Growing up and moving on in rheumatology: parents as proxies of adolescents with juvenile idiopathic arthritis. Arthritis Rheumatol. 2006;55(2):189–98. https://doi.org/10.1002/art.21834.
• Tunnicliffe DJ, Singh-Grewal D, Craig JC, Howell M, Tugwell P, Mackie F, et al. Healthcare and research priorities of adolescents and young adults with systemic lupus erythematosus: a mixed-methods study. J Rheumatol. 2017;44(4):444–51. https://doi.org/10.3899/jrheum.160720. Quantitative and qualitative analysis of response from interviews of Australian youth with childhood-onset SLE, indicating that mental health is viewed as an area of high priority for both research and healthcare for youth with SLE.
Tennermann N, Hazen M. Patient and family reported psychosocial areas of concern within pediatric rheumatology: quality improvement data and implications for practice. Arthritis Rheum. 2017;69.
• Knight AM, Vickery ME, Fiks AG, Barg FK. Barriers and facilitators for mental healthcare in pediatric lupus and mixed connective tissue disease: a qualitative study of youth and parent perspectives. Pediatr Rheumatol Online J. 2015;13:52. https://doi.org/10.1186/s12969-015-0049-1. Qualitative study that showed SLE/MCTD youth viewed pediatric rheumatologists as primary physicians and preferred screening and addressing mental health issues in the rheumatology setting.
Knight A, Vickery M, Fiks AG, Barg FK. The illness experience of youth with lupus/mixed connective tissue disease: a mixed methods analysis of patient and parent perspectives. Lupus. 2016;25(9):1028–39. https://doi.org/10.1177/0961203316646460.
Makay B, Emiroglu N, Unsal E. Depression and anxiety in children and adolescents with familial Mediterranean fever. Clin Rheumatol. 2010;29(4):375–9. https://doi.org/10.1007/s10067-009-1330-9.
Daltroy LH, Larson MG, Eaton HM, Partridge AJ, Pless IB, Rogers MP, et al. Psychosocial adjustment in juvenile arthritis. J Pediatr Psychol. 1992;17(3):277–89.
Knight A, Vickery M, Muscal E, Davis A, Harris J, Hersh AO, et al. Mental health care for adolescents with rheumatologic conditions: perspectives from pediatric behavioral health providers in North America. Arthritis Rheumatol. 2016;68:3153–6. https://doi.org/10.1002/art.39977.
Sibbitt WL Jr, Brandt JR, Johnson CR, Maldonado ME, Patel SR, Ford CC, et al. The incidence and prevalence of neuropsychiatric syndromes in pediatric onset systemic lupus erythematosus. J Rheumatol. 2002;29(7):1536–42.
Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. https://doi.org/10.1016/j.socscimed.2013.04.026.
Rubinstein T, Schwartz N, Jordan N, Lois R, Wahezi D, Stein REK, et al. Depression symptoms throughout the lifespan in a low-income, minority cohort of lupus patients: who is at risk? Arthritis Rheumatol. 2016;68:4331–3. https://doi.org/10.1002/art.39977.
Son MB, Sergeyenko Y, Guan H, Costenbader KH. Disease activity and transition outcomes in a childhood-onset systemic lupus erythematosus cohort. Lupus. 2016;25(13):1431–9. https://doi.org/10.1177/0961203316640913.
Julian LJ, Tonner C, Yelin E, Yazdany J, Trupin L, Criswell LA, et al. Cardiovascular and disease-related predictors of depression in systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2011;63(4):542–9. https://doi.org/10.1002/acr.20426.
• Spiegel LR, Stinson J, Campillo S, Cellucci T, Dancey P, Duffy C, et al. An internet-based self-management program for adolescents with juvenile idiopathic arthritis (JIA): A randomized controlled trial (RCT). Pediatric Rheumatol. 2017;15:133. https://doi.org/10.1186/s12969-017-0186-9. Large randomized control trial of an online behavioral intervention in JIA. Preliminary data does not show efficacy in improving outcomes regarding depression or anxiety.
Luca N, Daengsuwan T, Dalmau J, Jones K, deVeber G, Kobayashi J, et al. Anti-N-methyl-D-aspartate receptor encephalitis: a newly recognized inflammatory brain disease in children. Arthritis Rheumatol. 2011;63(8):2516–22. https://doi.org/10.1002/art.30437.
Florance NR, Davis RL, Lam C, Szperka C, Zhou L, Ahmad S, et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol. 2009;66(1):11–8. https://doi.org/10.1002/ana.21756.
Ramanan AV, Sawhney S, Murray KJ. Central nervous system complications in two cases of juvenile onset dermatomyositis. Rheumatology (Oxford). 2001;40(11):1293–8.
Deniz O, Caykoylu A, Vural G, Albayrak Y, Temel S, Aydin I, et al. A case study of neuro-psycho-Behcet’s syndrome presenting with psychotic attack. Clin Neurol Neurosurg. 2009;111(10):877–9. https://doi.org/10.1016/j.clineuro.2009.07.009.
Muscal E, Brey RL. Neurologic manifestations of systemic lupus erythematosus in children and adults. Neurol Clin. 2010;28(1):61–73. https://doi.org/10.1016/j.ncl.2009.09.004.
Parikh S, Swaiman KF, Kim Y. Neurologic characteristics of childhood lupus erythematosus. Pediatr Neurol. 1995;13(3):198–201.
Muscal E, Nadeem T, Li X, Mian A, Harris TB. Evaluation and treatment of acute psychosis in children with systemic lupus erythematosus (SLE): consultation-liaison service experiences at a tertiary-care pediatric institution. Psychosomatics. 2010;51(6):508–14. https://doi.org/10.1176/appi.psy.51.6.508.
ClinicalTrials.gov. National Library of Medicine, Bethesda, MD. Accessed 2017 Oct 30.
Soczynska JK, Kennedy SH, Goldstein BI, Lachowski A, Woldeyohannes HO, McIntyre RS. The effect of tumor necrosis factor antagonists on mood and mental health-associated quality of life: novel hypothesis-driven treatments for bipolar depression? Neurotoxicol. 2009;30(4):497–521. https://doi.org/10.1016/j.neuro.2009.03.004.
Gedik KC, Papaioannou H, Marcus M, Deutschman C, Gottlieb B. A prospective study to assess for changes in mood with initiation of anti-TNF therapy: a pilot study. Arthritis Rheumatol. 2017;69(Supp 4):82–5.
Hedayati SS, Gregg LP, Carmody T, Jain N, Toups M, Rush AJ, et al. Effect of sertraline on depressive symptoms in patients with chronic kidney disease without dialysis dependence: the cast randomized clinical trial. JAMA. 2017; https://doi.org/10.1001/jama.2017.17131.
• Lomholt JJ, Thastum M, Christensen AE, Leegaard A, Herlin T. Cognitive behavioral group intervention for pain and well-being in children with juvenile idiopathic arthritis: a study of feasibility and preliminary efficacy. Pediatr Rheumatol Online J. 2015;13:35. https://doi.org/10.1186/s12969-015-0032-x. A pilot study of cognitive behavioral therapy for JIA patients and parents that showed a high rate of completion of therapy, but low participation rate among patients who eligible for the study.
Wagner JL, Chaney JM, Hommel KA, Page MC, Mullins LL, White MM, et al. The influence of parental distress on child depressive symptoms in juvenile rheumatic diseases: the moderating effect of illness intrusiveness. J Pediatr Psychol. 2003;28(7):453–62.
Gomez-Ramirez O, Gibbon M, Berard R, Jurencak R, Green J, Tucker L, et al. A recurring rollercoaster ride: a qualitative study of the emotional experiences of parents of children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2016;14(1):13. https://doi.org/10.1186/s12969-016-0073-9.
Walco GA, Varni JW, Ilowite NT. Cognitive-behavioral pain management in children with juvenile rheumatoid arthritis. Pediatrics. 1992;89(6 Pt 1):1075–9.
Degotardi PJ, Klass ES, Rosenberg BS, Fox DG, Gallelli KA, Gottlieb BS. Development and evaluation of a cognitive-behavioral intervention for juvenile fibromyalgia. J Pediatr Psychol. 2006;31(7):714–23. https://doi.org/10.1093/jpepsy/jsj064.
Warner J, Moorman E, Cunningham N, Wiley K, Watts A, Kashikar-Zuck S, et al. Development of cognitive behavioral therapy (CBT) for childhood-onset systemic lupus erythematosus (cSLE) treatment. Arthritis Rheumatol. 2017;69:144–5. https://doi.org/10.1002/art.v69.S4.
Sansom-Daly UM, Peate M, Wakefield CE, Bryant RA, Cohn RJ. A systematic review of psychological interventions for adolescents and young adults living with chronic illness. Health Psychol. 2012;31(3):380–93. https://doi.org/10.1037/a0025977.
Zhou X, Hetrick SE, Cuijpers P, Qin B, Barth J, Whittington CJ, et al. Comparative efficacy and acceptability of psychotherapies for depression in children and adolescents: a systematic review and network meta-analysis. World Psychiatry. 2015;14(2):207–22. https://doi.org/10.1002/wps.20217.
Sharpe L, Sensky T, Timberlake N, Ryan B, Allard S. Long-term efficacy of a cognitive behavioural treatment from a randomized controlled trial for patients recently diagnosed with rheumatoid arthritis. Rheumatol (Oxford). 2003;42(3):435–41.
Navarrete-Navarrete N, Peralta-Ramirez MI, Sabio-Sanchez JM, Coin MA, Robles-Ortega H, Hidalgo-Tenorio C, et al. Efficacy of cognitive behavioural therapy for the treatment of chronic stress in patients with lupus erythematosus: a randomized controlled trial. Psychother Psychosom. 2010;79(2):107–15. https://doi.org/10.1159/000276370.
von Weiss RT, Rapoff MA, Varni JW, Lindsley CB, Olson NY, Madson KL, et al. Daily hassles and social support as predictors of adjustment in children with pediatric rheumatic disease. J Pediatr Psychol. 2002;27(2):155–65.
Timko C, Stovel KW, Moos RH. Functioning among mothers and fathers of children with juvenile rheumatic disease: a longitudinal study. J Pediatr Psychol. 1992;17(6):705–24.
White MM, Chaney JM, Wagner JL, Andrews NR, Mullins LL, Hommel KA, et al. Children’s perceived illness uncertainty as a moderator in the parent-child distress relation in juvenile rheumatic diseases. Rehabil Psychol. 2005;50(3):224–31. https://doi.org/10.1037/0090-5550.50.3.224.
• Chaney JM, Gamwell KL, Baraldi AN, Ramsey RR, Cushing CC, Mullins AJ, et al. Parent perceptions of illness uncertainty and child depressive symptoms in juvenile rheumatic diseases: examining caregiver demand and parent distress as mediators. J Pediatr Psychol. 2016;41(9):941–51. https://doi.org/10.1093/jpepsy/jsw004. Indicates that distress experienced by parents from perceptions about disease uncertainty can lead to depressive symptoms in patients with rheumatologic diseases in a moderately large, diverse group of patients.
Ireys HT, Sills EM, Kolodner KB, Walsh BB. A social support intervention for parents of children with juvenile rheumatoid arthritis: results of a randomized trial. J Pediatr Psychol. 1996;21(5):633–41.
Haupt M, Millen S, Janner M, Falagan D, Fischer-Betz R, Schneider M. Improvement of coping abilities in patients with systemic lupus erythematosus: a prospective study. Ann Rheum Dis. 2005;64(11):1618–23. https://doi.org/10.1136/ard.2004.029926.
Karlson EW, Liang MH, Eaton H, Huang J, Fitzgerald L, Rogers MP, et al. A randomized clinical trial of a psychoeducational intervention to improve outcomes in systemic lupus erythematosus. Arthritis Rheum. 2004;50(6):1832–41. https://doi.org/10.1002/art.20279.
Stinson J, Ahola Kohut S, Forgeron P, Amaria K, Bell M, Kaufman M, et al. The iPeer2Peer Program: a pilot randomized controlled trial in adolescents with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2016;14(1):48. https://doi.org/10.1186/s12969-016-0108-2.
Shilling V, Morris C, Thompson-Coon J, Ukoumunne O, Rogers M, Logan S. Peer support for parents of children with chronic disabling conditions: a systematic review of quantitative and qualitative studies. Dev Med Child Neurol. 2013;55(7):602–9. https://doi.org/10.1111/dmcn.12091.
Williams EM, Egede L, Oates J, Voronca D, Gebregziabher M. Peer approaches to lupus self-management (pals): a novel lupus peer mentorship Intervention. Arthritis Rheumatol. 2016. 68 (suppl 10).
Williams EM, Egede L, Faith T, Oates J. Effective self-management Interventions for patients with lupus: potential impact of peer mentoring. Am J Med Sci. 2017;353(6):580–92. https://doi.org/10.1016/j.amjms.2017.01.011.
Cohen EM, Dossett ML, Mehta DH, Davis RB, Lee YC. Factors associated with complementary medicine use in pediatric musculoskeletal conditions: Results from a national survey. Complement Ther Med. 2017;31:53–8. https://doi.org/10.1016/j.ctim.2017.02.001.
Feldman DE, Duffy C, De Civita M, Malleson P, Philibert L, Gibbon M, et al. Factors associated with the use of complementary and alternative medicine in juvenile idiopathic arthritis. Arthritis Rheum. 2004;51(4):527–32. https://doi.org/10.1002/art.20536.
Field T, Hernandez-Reif M, Seligman S, Krasnegor J, Sunshine W, Rivas-Chacon R, et al. Juvenile rheumatoid arthritis: benefits from massage therapy. J Pediatr Psychol. 1997;22(5):607–17.
Zebracki K, Holzman K, Bitter KJ, Feehan K, Miller ML. Brief report: use of complementary and alternative medicine and psychological functioning in Latino children with juvenile idiopathic arthritis or arthralgia. J Pediatr Psychol. 2007;32(8):1006–10. https://doi.org/10.1093/jpepsy/jsm033.
Ahola Kohut S, Stinson J, Davies-Chalmers C, Ruskin D, van Wyk M. Mindfulness-based interventions in clinical samples of adolescents with chronic illness: a systematic review. J Altern Complement Med. 2017;23(8):581–9. https://doi.org/10.1089/acm.2016.0316.
Carvalho MR, Sato EI, Tebexreni AS, Heidecher RT, Schenkman S, Neto TL. Effects of supervised cardiovascular training program on exercise tolerance, aerobic capacity, and quality of life in patients with systemic lupus erythematosus. Arthritis Rheum. 2005;53(6):838–44. https://doi.org/10.1002/art.21605.
Zautra AJ, Davis MC, Reich JW, Nicassario P, Tennen H, Finan P, et al. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J Consult Clin Psychol. 2008;76(3):408–21. https://doi.org/10.1037/0022-006X.76.3.408.
Stinson JN, McGrath PJ, Hodnett ED, Feldman BM, Duffy CM, Huber AM, et al. An internet-based self-management program with telephone support for adolescents with arthritis: a pilot randomized controlled trial. J Rheumatol. 2010;37(9):1944–52. https://doi.org/10.3899/jrheum.091327.
Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of internet-based self-management interventions for youth with health conditions. J Pediatr Psychol. 2009;34(5):495–510. https://doi.org/10.1093/jpepsy/jsn115.
Acknowledgements
The authors would like to thank the generous assistance of Aurelia Minuti, head reference librarian from Albert Einstein College of Medicine, for her guidance regarding searching algorithms used for this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tamar Rubinstein declares that she has no conflict of interest.
Alaina Davis declares that she has no conflict of interest.
Martha Rodriguez declares that she has no conflict of interest.
Andrea Knight declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Rheumatology
Rights and permissions
About this article
Cite this article
Rubinstein, T.B., Davis, A.M., Rodriguez, M. et al. Addressing Mental Health in Pediatric Rheumatology. Curr Treat Options in Rheum 4, 55–72 (2018). https://doi.org/10.1007/s40674-018-0092-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-018-0092-4