Abstract
Purpose of Review
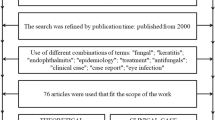
World-wide, ocular fungal infections (ophthalmic mycoses) are important causes of morbidity and blindness (or even life-threatening infections). There is a need to bring together a concise review covering the many recent advances and reports, as well as data from excellent studies carried out during the last decade.
Recent Findings
This report also provides new data from the latest understanding of the pathogenesis of both keratitis and endophthalmitis. The latest diagnostic modalities of fungal infections as well as fungal species identification have been reviewed. Information from the latest multi-centric drug trials has been reviewed.
Summary
This report provides a synopsis of literature published within the last couple of decades, but specifically, noteworthy reviews and important studies. Emphasis is on mycotic keratitis (a significant public health problem in many countries and accounting for the majority of microbial keratitis—the second most common cause of blindness), as well as on endophthalmitis. Recent information on other ocular mycotic infections is also collated.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ozkan J, Willcox MD. The ocular microbiome: molecular characterisation of a unique and low microbial environment. Curr Eye Res. 2019;44:685–94. https://doi.org/10.1080/02713683.2019.1570526.
Wen X, Miao L, Deng Y, Bible PW, Hu X, Zou Y, et al. The influence of age and sex on ocular surface microbiota in healthy adults. Invest Ophthalmol Vis Sci. 2017;58:6030–7. https://doi.org/10.1167/iovs.17-22957.
Gonzales CA, Srinivasan M, Whitcher JP, Smolin G. Incidence of corneal ulceration in Madurai district, South India. Ophthalmic Epidemiol. 1996;3:159–66. https://doi.org/10.3109/09286589609080122.
Tanure MA, Cohen EJ, Sudesh S, Rapuano CJ, Laibson PR. Spectrum of fungal keratitis at Wills Eye Hospital, Philadelphia, Pennsylvania. Cornea. 2000;19:307–12. https://doi.org/10.1097/00003226-200005000-00010.
Laspina F, Samudio M, Cibils D, Ta CN, Fariña N, Sanabria R, et al. Epidemiological characteristics of microbiological results on patients with infectious corneal ulcers: a 13-year survey in Paraguay. Graefes Arch ClinExp Ophthalmol. 2004;242:204–9. https://doi.org/10.1007/s00417-003-0808-4.
Rautaraya B, Sharma S, Kar S, Das S, Sahu SK. Diagnosis and treatment outcome of mycotic keratitis at a tertiary eye care center in eastern India. BMC Ophthalmol. 2011;11:39. https://doi.org/10.1186/1471-2415-11-39.
Lalitha P, Prajna NV, Manoharan G, Srinivasan M, Mascarenhas J, Das M, et al. Trends in bacterial and fungal keratitis in South India, 2002-2012. Br J Ophthalmol. 2015;99:192–4. https://doi.org/10.1136/bjophthalmol-2014-305000.
Bharathi MJ, Ramakrishnan R, Meenakshi R, Padmavathy S, Shivakumar C, Srinivasan M. Microbial keratitis in South India: influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol. 2007;14:61–9. https://doi.org/10.1080/09286580601001347.
• Satpathy G, Ahmed NH, Nayak N, Tandon R, Sharma N, Agarwal T, et al. Spectrum of mycotic keratitis in north India: Sixteen years study from a tertiary care ophthalmic centre. J Infect Public Health. 12:367–71. https://doi.org/10.1016/j.jiph.2018.12.005The largest compilation of clinico-epidemiological and microbiological features of fungal keratitis—a retrospective analysis covering 16 years.
•• Prajna VN, Prajna L, Muthiah S. Fungal keratitis: the Aravind experience. Indian J Ophthalmol. 2017;65:912–9. https://doi.org/10.4103/ijo.IJO_821_17A comprehensive synopsis of the over two-decade experience of the largest eye hospital network in India—straddling public health issues, collaborations, and clinical studies.
Gower EW, Keay LJ, Oechsler RA, Iovieno A, Alfonso EC, Jones DB, et al. Trends in fungal keratitis in the United States, 2001 to 2007. Ophthalmology. 2010;117:2263–7. https://doi.org/10.1016/j.ophtha.2010.03.048.
Ansari Z, Miller D, Galor A. Current thoughts in fungal keratitis: diagnosis and treatment. Curr Fungal Infect Rep. 2013;7:209–218. https://doi.org/10.1007/s12281-013-0150-110.1007/s12281-013-0150-1.
Keay LJ, Gower EW, Iovieno A, Oechsler RA, Alfonso EC, Matoba A, et al. Clinical and microbiological characteristics of fungal keratitis in the United States, 2001–2007: a multicenter study. Ophthalmology. 2011;118:920–6. https://doi.org/10.1016/j.ophtha.2010.09.011.
Gopinathan U, Garg P, Fernandes M, Sharma S, Athmanathan S, Rao GN. The epidemiological features and laboratory results of fungal keratitis: a 10-year review at a referral eye care center in South India. Cornea. 2002;21:555–9. https://doi.org/10.1097/00003226-200208000-00004.
•• Thomas PA. Current perspectives on ophthalmic mycoses. Clin Microbiol Rev. 2003;16:730–97. https://doi.org/10.1128/cmr.16.4.730-797.2003An extensive review of literature on all fungal infections and diseases of the eye—with detailed descriptive and referenced tables on all reported ocular fungi, specimens, diagnostic methods, pathogenesis, antifungal agents, and medical management.
Thomas P. Tropicalophthalmomycoses. In: Seal D, Pleyer U, editors. Ocular infection. 2nded. New York: Informa Healthcare; 2007:271–305.
Xie L, Zhong W, Shi W, Sun S. Spectrum of fungal keratitis in north China. Ophthalmology. 2006;113:1943–8. https://doi.org/10.1016/j.ophtha.2006.05.035.
Nath R, Baruah S, Saikia L, Devi B, Borthakur AK, Mahanta J. Mycotic corneal ulcers in upper Assam. Indian J Ophthalmol. 2011;59:367–71. https://doi.org/10.4103/0301-4738.83613.
Sangwan J, Lathwal S, Juyal D, Sharma N. Fonsecaeapedrosoi: a rare etiology in fungal keratitis. J ClinDiagnRes. 2013;7:2272–3. https://doi.org/10.7860/JCDR/2013/6627.3491.
Lekhanont K, Nonpassopon M, Nimvorapun N, Santanirand P. Treatment with intrastromal and intracameralvoriconazole in 2 eyes with Lasiodiplodiatheobromae keratitis: case reports. Medicine. 2015;94:e541. https://doi.org/10.1097/MD.0000000000000541.
Gaujoux T, Borsali E, Gavrilov J-C, Touzeau O, Goldschmidt P, Despiau MC,et al. [Fungal keratitis caused by Cylindrocarponlichenicola]. J Fr Ophthalmol 2012;35:356.e1–5. https://doi.org/10.1016/j.jfo.2011.06.005.
Jhanji V, Yohendran J, Constantinou M, Sheorey H, Vajpayee RB. Scedosporiumscleritis or keratitis or both: case series. Eye Contact Lens. 2009;35:312–5. https://doi.org/10.1097/ICL.0b013e3181be722e.
Motley WW, Melson AT, Mortensen JE. Pediatric Metarrhiziumanisopliae keratitis. JAAPOS. 2011;15:101–3. https://doi.org/10.1016/j.jaapos.2010.12.003.
Bhartiya P, Daniell M, Constantinou M, Islam FM, Taylor HR. Fungal keratitis in Melbourne. ClinExp Ophthalmol. 2007;35:124–30. https://doi.org/10.1111/j.1442-9071.2006.01405.x.
Sun RL, Jones DB, Wilhelmus KR. Clinical characteristics and outcome of Candida keratitis. Am J Ophthalmol. 2007;143:1043–5. https://doi.org/10.1016/j.ajo.2007.02.016.
Bharathi MJ, Ramakrishnan R, Vasu S, Meenakshi R, Palaniappan R. Epidemiological characteristics and laboratory diagnosis of fungal keratitis. A three-year study. Indian J Ophthalmol. 2003;51:315–21.
• Raghavan A, Baidwal S, Venkatapathy N, Rammohan R. The Acanthamoeba-fungal keratitis study. Am J Ophthalmol. 2019;201:31–6. https://doi.org/10.1016/j.ajo.2019.01.024A 17-month prospective study which showed that Acanthamoeba-fungal co-infections are more prevalent than currently known.
Mendoza L, Vilela R. The mammalian pathogenic oomycetes. Curr Fungal Infect Rep. 2013;7:198–208. https://doi.org/10.1007/s12281-013-0144-z.
Thanathanee O, Enkvetchakul O, Rangsin R, Waraasawapati S, Samerpitak K, Suwan-apichon O. Outbreak of Pythium keratitis during rainy season: a case series. Cornea. 2013;32:199–204. https://doi.org/10.1097/ICO.0b013e3182535841.
Agarwal S, Iyer G, Srinivasan B, Benurwar S, Agarwal M, Narayanan N, et al. Clinical profile, risk factors and outcome of medical, surgical and adjunct interventions in patients with Pythiuminsidiosum keratitis. Br J Ophthalmol. 2019;103:296–300. https://doi.org/10.1136/bjophthalmol-2017-311804.
• Hasika R, Lalitha P, Radhakrishnan N, Rameshkumar G, Prajna NV, Srinivasan M. Pythium keratitis in South India: incidence, clinical profile, management, and treatment recommendation. Indian J Ophthalmol. 2019;67:42–7. https://doi.org/10.4103/ijo.IJO_445_18Describes the South Indian experience with Pythium keratitis.
Brown GD, Gordon S. Immune recognition of fungal beta-glucans. Cell Microbiol. 2005;7:471–9. https://doi.org/10.1111/j.1462-5822.2005.00505.x.
Wu J, Zhang W-S, Zhao J, Zhou H-Y. Review of clinical and basic approaches of fungal keratitis. Int J Ophthalmol. 2016;9:1676–83. https://doi.org/10.18240/ijo.2016.11.23.
Taube M-A, del Mar CM, Elsahn A, Christodoulides M, Hossain P. Pattern recognition receptors in microbial keratitis. Eye (Lond). 2015;29:1399–415. https://doi.org/10.1038/eye.2015.118.
Ananthi S, Chitra T, Bini R, Prajna NV, Lalitha P, Dharmalingam K. Comparative analysis of the tear protein profile in mycotic keratitis patients. Mol Vis. 2008;14:500–7.
Ananthi S, VenkateshPrajna N, Lalitha P, Valarnila M, Dharmalingam K. Pathogen induced changes in the protein profile of human tears from Fusarium keratitis patients. PLoS One. 2013;8:e53018. https://doi.org/10.1371/journal.pone.0053018.
Parthiban N, Sampath NL, JeyaMaheshwari J, Prajna NV, Lalitha P, Dharmalingam K. Quantitative profiling of tear proteome reveals down regulation of zinc alpha-2 glycoprotein in Aspergillus flavus keratitis patients. Exp Eye Res. 2019;186:107700. https://doi.org/10.1016/j.exer.2019.107700.
Selvam RM, Nithya R, Devi PN, Shree RSB, Nila MV, Demonte NL, et al. Exoproteome of Aspergillus flavus corneal isolates and saprophytes: identification of proteoforms of an oversecreted alkaline protease. J Proteome. 2015;115:23–35. https://doi.org/10.1016/j.jprot.2014.11.017.
Kandhavelu J, Demonte NL, Namperumalsamy VP, Prajna L, Thangavel C, Jayapal JM, et al. Data set of Aspergillus flavus induced alterations in tear proteome: understanding the pathogen-induced host response to fungal infection. Data Brief. 2016;9:888–94. https://doi.org/10.1016/j.dib.2016.11.003.
Gopinathan U, Ramakrishna T, Willcox M, Rao CM, Balasubramanian D, Kulkarni A, et al. Enzymatic, clinical and histologic evaluation of corneal tissues in experimental fungal keratitis in rabbits. Exp Eye Res. 2001;72:433–42. https://doi.org/10.1006/exer.2000.0971.
Leema G, Kaliamurthy J, Geraldine P, Thomas PA. Keratitis due to Aspergillus flavus: clinical profile, molecular identification of fungal strains and detection of aflatoxin production. Mol Vis. 2010;16:843–54.
Chinnery HR, Humphries T, Clare A, Dixon AE, Howes K, Moran CB, et al. Turnover of bone marrow-derived cells in the irradiated mouse cornea. Immunology. 2008;125:541–8. https://doi.org/10.1111/j.1365-2567.2008.02868.x.
Hamrah P, Dana MR. Corneal antigen-presenting cells. ChemImmunol Allergy. 2007;92:58–70. https://doi.org/10.1159/000099254.
Pearlman E, Johnson A, Adhikary G, Sun Y, Chinnery HR, Fox T, et al. Toll-like receptors at the ocular surface. Ocul Surf. 2008;6:108–16. https://doi.org/10.1016/s1542-0124(12)70279-3.
Leal SM, Cowden S, Hsia Y-C, Ghannoum MA, Momany M, Pearlman E. Distinct roles for Dectin-1 and TLR4 in the pathogenesis of Aspergillus fumigatus keratitis. PLoS Pathog. 2010;6:e1000976. https://doi.org/10.1371/journal.ppat.1000976.
Sun Y, Chandra J, Mukherjee P, Szczotka-Flynn L, Ghannoum MA, Pearlman E. A murine model of contact lens-associated fusarium keratitis. Invest Ophthalmol Vis Sci. 2010;51:1511–6. https://doi.org/10.1167/iovs.09-4237.
Karthikeyan RS, Vareechon C, Prajna NV, Dharmalingam K, Pearlman E, Lalitha P. Interleukin 17 expression in peripheral blood neutrophils from fungal keratitis patients and healthy cohorts in southern India. J Infect Dis. 2015;211:130–4. https://doi.org/10.1093/infdis/jiu381.
Karthikeyan RS, Leal SM, Prajna NV, Dharmalingam K, Geiser DM, Pearlman E, et al. Expression of innate and adaptive immune mediators in human corneal tissue infected with Aspergillus or fusarium. J Infect Dis. 2011;204:942–50. https://doi.org/10.1093/infdis/jir426.
Mascarenhas J, Lalitha P, Prajna NV, Srinivasan M, Das M, D’Silva SS, et al. Acanthamoeba, fungal, and bacterial keratitis: a comparison of risk factors and clinical features. Am J Ophthalmol. 2014;157:56–62. https://doi.org/10.1016/j.ajo.2013.08.032.
Dahlgren MA, Lingappan A, Wilhelmus KR. The clinical diagnosis of microbial keratitis. Am J Ophthalmol. 2007;143:940–4. https://doi.org/10.1016/j.ajo.2007.02.030.
Dalmon C, Porco TC, Lietman TM, Prajna NV, Prajna L, Das MR, et al. The clinical differentiation of bacterial and fungal keratitis: a photographic survey. Invest Ophthalmol Vis Sci. 2012;53:1787–91. https://doi.org/10.1167/iovs.11-8478.
Vanzzini Zago V, Alcantara Castro M, Naranjo TR. Support of the laboratory in the diagnosis of fungal ocular infections. Int J Inflam. 2012;643104:1–8. https://doi.org/10.1155/2012/643104.
Sharma S, Kunimoto DY, Gopinathan U, Athmanathan S, Garg P, Rao GN. Evaluation of corneal scraping smear examination methods in the diagnosis of bacterial and fungal keratitis: a survey of eight years of laboratory experience. Cornea. 2002;21:643–7. https://doi.org/10.1097/00003226-200210000-00002.
Leck AK, Thomas PA, Hagan M, Kaliamurthy J, Ackuaku E, John M, et al. Aetiology of suppurative corneal ulcers in Ghana and south India, and epidemiology of fungal keratitis. Br J Ophthalmol. 2002;86:1211–5. https://doi.org/10.1136/bjo.86.11.1211.
Brasnu E, Bourcier T, Dupas B, Degorge S, Rodallec T, Laroche L, et al. In vivo confocal microscopy in fungal keratitis. Br J Ophthalmol. 2007;91:588–91. https://doi.org/10.1136/bjo.2006.107243.
Chidambaram JD, Prajna NV, Larke NL, Palepu S, Lanjewar S, Shah M, et al. Prospective study of the diagnostic accuracy of the in vivo laser scanning confocal microscope for severe microbial keratitis. Ophthalmology. 2016;123:2285–93. https://doi.org/10.1016/j.ophtha.2016.07.009.
Chidambaram JD, Prajna NV, Larke N, Macleod D, Srikanthi P, Lanjewar S, et al. In vivo confocal microscopy appearance of Fusarium and Aspergillus species in fungal keratitis. Br J Ophthalmol. 2017;101:1119–23. https://doi.org/10.1136/bjophthalmol-2016-309656.
Labbé A, Khammari C, Dupas B, Gabison E, Brasnu E, Labetoulle M, et al. Contribution of in vivo confocal microscopy to the diagnosis and management of infectious keratitis. Ocul Surf. 2009;7:41–52. https://doi.org/10.1016/s1542-0124(12)70291-4.
Das S, Samant M, Garg P, Vaddavalli PK, Vemuganti GK. Role of confocal microscopy in deep fungal keratitis. Cornea. 2009;28:11–3. https://doi.org/10.1097/ICO.0b013e318181cff7.
Kumar RL, Cruzat A, Hamrah P. Current state of in vivo confocal microscopy in management of microbial keratitis. Semin Ophthalmol. 2010;25:166–70. https://doi.org/10.3109/08820538.2010.518516.
Takezawa Y, Shiraishi A, Noda E, Hara Y, Yamaguchi M, Uno T, et al. Effectiveness of in vivo confocal microscopy in detecting filamentous fungi during clinical course of fungal keratitis. Cornea. 2010;29:1346–52. https://doi.org/10.1097/ICO.0b013e3181cd3c84.
Vaddavalli PK, Garg P, Sharma S, Sangwan VS, Rao GN, Thomas R. Role of confocal microscopy in the diagnosis of fungal and acanthamoeba keratitis. Ophthalmology. 2011;118:29–35. https://doi.org/10.1016/j.ophtha.2010.05.018.
Martone G, Pichierri P, Franceschini R, Moramarco A, Ciompi L, Tosi GM, et al. In vivo confocal microscopy and anterior segment optical coherence tomography in a case of alternaria keratitis. Cornea. 2011;30:449–53. https://doi.org/10.1097/ICO.0b013e3181dae1f3.
Ghosh A, Basu S, Datta H, Chattopadhyay D. Evaluation of polymerase chain reaction-based ribosomal DNA sequencing technique for the diagnosis of mycotic keratitis. Am J Ophthalmol. 2007;144:396–403. https://doi.org/10.1016/j.ajo.2007.05.017.
Kim E, Chidambaram JD, Srinivasan M, Lalitha P, Wee D, Lietman TM, et al. Prospective comparison of microbial culture and polymerase chain reaction in the diagnosis of corneal ulcer. Am J Ophthalmol 2008;146:714–723,723.e1. https://doi.org/10.1016/j.ajo.2008.06.009.
Vengayil S, Panda A, Satpathy G, Nayak N, Ghose S, Patanaik D, et al. Polymerase chain reaction-guided diagnosis of mycotic keratitis: a prospective evaluation of its efficacy and limitations. Invest Ophthalmol Vis Sci. 2009;50:152–6. https://doi.org/10.1167/iovs.07-1283.
Thomas PA, Teresa AP, Theodore J, Geraldine P. PCR for the molecular diagnosis of mycotic keratitis. Expert Rev Mol Diagn. 2012;12:703–18. https://doi.org/10.1586/erm.12.65.
Tananuvat N, Salakthuantee K, Vanittanakom N, Pongpom M, Ausayakhun S. Prospective comparison between conventional microbial work-up vs PCR in the diagnosis of fungal keratitis. Eye (Lond). 2012;26:1337–43. https://doi.org/10.1038/eye.2012.162.
Manikandan P, Abdel-Hadi A, Randhir Babu Singh Y, Revathi R, Anita R, Banawas S, et al. Fungal keratitis: epidemiology, rapid detection, and antifungal susceptibilities of Fusarium and Aspergillus isolates from corneal scrapings. Biomed Res Int 2019:6395840. https://doi.org/10.1155/2019/6395840, 2019, 9.
• Ferrer C, Alió JL. Evaluation of molecular diagnosis in fungal keratitis. Ten years of experience. J Ophthalmic Inflamm Infect. 2011;1:15–22. https://doi.org/10.1007/s12348-011-0019-9A ten-year review of molecular diagnostics in fungal keratitis.
Homa M, Shobana CS, Singh YRB, Manikandan P, Selvam KP, Kredics L, et al. Fusarium keratitis in South India: causative agents, their antifungal susceptibilities and a rapid identification method for the Fusarium solani species complex. Mycoses. 2013;56:501–11. https://doi.org/10.1111/myc.12062.
Oechsler RA, Feilmeier MR, Miller D, Shi W, Hofling-Lima AL, Alfonso EC. Fusarium keratitis: genotyping, in vitro susceptibility and clinical outcomes. Cornea. 2013;32:667–73. https://doi.org/10.1097/ICO.0b013e318277ac74.
•• Flor Cruz NV, Evans JR. Medical interventions for fungal keratitis. Cochrane Database Syst Rev 2015;CD004241. https://doi.org/10.1002/14651858.CD004241.pub4A systematic Cochrane Database review of 12 large-scale clinical trials in mycotic ulcers.
Prajna NV, Krishnan T, Mascarenhas J, Rajaraman R, Prajna L, Srinivasan M, et al. The mycotic ulcer treatment trial: a randomized trial comparing natamycin vs voriconazole. JAMA Ophthalmol. 2013;131:422–9. https://doi.org/10.1001/jamaophthalmol.2013.1497.
•• Prajna NV, Krishnan T, Rajaraman R, Patel S, Srinivasan M, Das M, et al. Effect of oral voriconazole on fungal keratitis in the Mycotic Ulcer Treatment Trial II (MUTT II): a randomized clinical trial. JAMA Ophthalmol. 2016;134:1365–72. https://doi.org/10.1001/jamaophthalmol.2016.4096The first and conclusive clinical trial to conclude that natamycin was better than voriconazole; and the first to describe genus-specific differential drug sensitivities.
Das T, Hussain A, Naduvilath T, Sharma S, Jalali S, Majji AB. Case control analyses of acute endophthalmitis after cataract surgery in South India associated with technique, patient care, and socioeconomic status. J Ophthalmol. 2012;298459:1–6. https://doi.org/10.1155/2012/298459.
Chakrabarti A, Shivaprakash MR, Singh R, Tarai B, George VK, Fomda BA, et al. Fungal endophthalmitis: fourteen years’ experience from a center in India. Retina (Philadelphia, Pa) 2008;28:1400–1407. https://doi.org/10.1097/iae.0b013e318185e943.
Lalitha P, Sengupta S, Ravindran RD, Sharma S, Joseph J, Ambiya V, et al. A literature review and update on the incidence and microbiology spectrum of postcataract surgery endophthalmitis over past two decades in India. Indian J Ophthalmol. 2017;65:673–7. https://doi.org/10.4103/ijo.IJO_509_17.
Behera UC, Budhwani M, Das T, Basu S, Padhi TR, Barik MR, et al. Role of early vitrectomy in the treatment of fungal endophthalmitis. Retina (Philadelphia, Pa) 2018;38:1385–1392. https://doi.org/10.1097/IAE.0000000000001727.
Gupta A, Gupta V, Gupta A, Dogra MR, Pandav SS, Ray P, et al. Spectrum and clinical profile of post cataract surgery endophthalmitis in north India. Indian J Ophthalmol. 2003;51:139–45.
Anand AR, Therese KL, Madhavan HN. Spectrum of aetiological agents of postoperative endophthalmitis and antibiotic susceptibility of bacterial isolates. Indian J Ophthalmol. 2000;48:123–8.
Benz MS, Scott IU, Flynn HW, Unonius N, Miller D. Endophthalmitis isolates and antibiotic sensitivities: a 6-year review of culture-proven cases. Am J Ophthalmol. 2004;137:38–42. https://doi.org/10.1016/s0002-9394(03)00896-1.
Wykoff CC, Flynn HW, Miller D, Scott IU, Alfonso EC. Exogenous fungal endophthalmitis: microbiology and clinical outcomes. Ophthalmology 2008;115:1501–1507, 1507.e1–2. https://doi.org/10.1016/j.ophtha.2008.02.027.
Modjtahedi BS, Finn AP, Barb SM, MacLachlan MJ, van Zyl T, Papakostas TD, et al. Characteristics and outcomes of endogenous endophthalmitis: eight-year experience at a tertiary care center. Ophthalmol Retina. 2019;3:61–72. https://doi.org/10.1016/j.oret.2018.08.009.
Durand ML. Endophthalmitis. In: Mandell GL, Bennett JE, Dolin R, editors.Principles and practice of infectious diseases, Vol. 1. 8th ed. Philadelphia, PA: Churchill Livingstone/Elsevier; 2015.
Mayer C, Loos D, Feucht N, Zapp D, Prahs PM, Tandogan T, et al. [Endogenous endophthalmitis: epidemiology, clinic, therapy and visual outcome]. KlinMonblAugenheilkd 2019;236:1208–1214. https://doi.org/10.1055/s-0044-101152.
Cho H, Shin YU, Siegel NH, Yu HG, Sobrin L, Patel A, et al. Endogenous endophthalmitis in the American and Korean population: an 8-year retrospective study. Ocul Immunol Inflamm. 2018;26:496–503. https://doi.org/10.1080/09273948.2016.1195000.
Modjtahedi BS, Finn AP, Papakostas TD, Durand M, Husain D, Eliott D. Intravenous drug use-associated endophthalmitis. Ophthalmol Retina. 2017;1:192–9. https://doi.org/10.1016/j.oret.2016.10.013.
Gupta N, Singh PK, Revankar SG, Chandrasekar PH, Kumar A. Pathobiology of Aspergillus fumigatus endophthalmitis in immunocompetent and immunocompromised mice. Microorganisms. 2019;7. https://doi.org/10.3390/microorganisms7090297.
Ramadan RT, Moyer AL, Callegan MC. A role for tumor necrosis factor-alpha in experimental Bacillus cereus endophthalmitis pathogenesis. Invest Ophthalmol Vis Sci. 2008;49:4482–9. https://doi.org/10.1167/iovs.08-2085.
Clark HL, Abbondante S, Minns MS, Greenberg EN, Sun Y, Pearlman E. Protein deiminase 4 and CR3 regulate Aspergillus fumigatus and β-glucan-induced neutrophil extracellular trap formation, but hyphal killing is dependent only on CR3. Front Immunol. 2018;9:1182. https://doi.org/10.3389/fimmu.2018.01182.
Stern WH, Tamura E, Jacobs RA, Pons VG, Stone RD, O’Day DM, et al. Epidemic postsurgical Candida parapsilosis endophthalmitis. Clinical findings and management of 15 consecutive cases. Ophthalmology. 1985;92:1701–9. https://doi.org/10.1016/s0161-6420(85)34095-2.
Essman TF, Flynn HW, Smiddy WE, Brod RD, Murray TG, Davis JL, et al. Treatment outcomes in a 10-year study of endogenous fungal endophthalmitis. Ophthalmic Surg Lasers. 1997;28:185–94.
Hunt KE, Glasgow BJ. Aspergillus endophthalmitis. An unrecognized endemic disease in orthotopic liver transplantation. Ophthalmology. 1996;103:757–67. https://doi.org/10.1016/s0161-6420(96)30619-2.
Deshmukh D, Chakrabarti M, Jayasudha R, Hasnat Ali M, Tyagi M, Sharma S, et al. Elevated cytokine levels in vitreous as biomarkers of disease severity in infectious endophthalmitis. PLoS One. 2018;13(10):e0205292. https://doi.org/10.1371/journal.pone.0205292.
Silva RA, Sridhar J, Miller D, Wykoff CC, Flynn HW. Exogenous fungal endophthalmitis: an analysis of isolates and susceptibilities to antifungal agents over a 20-year period (1990–2010). Am J Ophthalmol 2015;159:257–264.e1. https://doi.org/10.1016/j.ajo.2014.10.027.
Kim DY, Moon HI, Joe SG, Kim J-G, Yoon YH, Lee JY. Recent clinical manifestation and prognosis of fungal endophthalmitis: a 7-year experience at a tertiary referral center in Korea. J Korean Med Sci. 2015;30:960–4. https://doi.org/10.3346/jkms.2015.30.7.960.
Coats ML, Peyman GA. Intravitreal corticosteroids in the treatment of exogenous fungal endophthalmitis. Retina (Philadelphia, Pa) 1992;12:46–51. https://doi.org/10.1097/00006982-199212010-00010.
Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocul Surf. 2009;7:S1–S14. https://doi.org/10.1016/s1542-0124(12)70620-1.
Anane S, AnaneTouzri R, Malouche N, El Aich F, Beltaief O, Zhioua R, et al. [Which is the role of parasites and yeasts in the genesis of chronic blepharitis?]. PatholBiol 2007;55:323–327. https://doi.org/10.1016/j.patbio.2007.03.005.
•• Dadaci Z, Kılınç F, Ozer TT, Sahin GO, Acir NO, Borazan M. Periodic acid-Schiff staining demonstrates fungi in chronic anterior blepharitis. Eye (Lond). 2015;29:1522–7. https://doi.org/10.1038/eye.2015.144Rapid detection of fungal blepharitis using PAS stain.
Sahin GO, Dadaci Z, Ozer TT. Two cases of tinea ciliaris with blepharitis due to Microsporumaudouinii and Trichophyton verrucosum and review of the literature. Mycoses. 2014;57:577–80. https://doi.org/10.1111/myc.12201.
Lee C-Y, Ho Y-J, Sun C-C, Lin H-C, Hsiao C-H, Ma DH-K, et al. Recurrent fungal keratitis and blepharitis caused by Aspergillus flavus. Am J Trop Med Hyg. 2016;95:1216–8. https://doi.org/10.4269/ajtmh.16-0453.
Kashima T, Honma R, Kishi S, Hirato J. Bulbar conjunctival sporotrichosis presenting as a salmon-pink tumor. Cornea. 2010;29:573–6. https://doi.org/10.1097/ICO.0b013e3181ba7039.
Nair AG, Ali MJ, Kaliki S, Naik MN. Rhinosporidiosis of the tarsal conjunctiva. Indian J Ophthalmol. 2015;63:462–3. https://doi.org/10.4103/0301-4738.159897.
Usha K, Smitha S, Shah N, Lalitha P, Kelkar R. Spectrum and the susceptibilities of microbial isolates in cases of congenital nasolacrimal duct obstruction. J AAPOS. 2006;10:469–72. https://doi.org/10.1016/j.jaapos.2006.04.009.
Obi E, Roy A, Bates V, Sandy C. Bilateral chronic fungal dacryocystitis caused by Candida dubliniensis in a neutropenic patient. J ClinPathol. 2006;59:1194–5. https://doi.org/10.1136/jcp.2005.027540.
Jeang LJ, Davis A, Madow B, Espana EM, Margo CE. Occult fungal scleritis. Ocul Oncol Pathol. 2017;3:41–4. https://doi.org/10.1159/000449103.
Todokoro D, Hoshino J, Yo A, Makimura K, Hirato J, Akiyama H. Scedosporiumapiospermum infectious scleritis following posterior subtenon triamcinolone acetonide injection: a case report and literature review. BMC Ophthalmol. 2018;18:40. https://doi.org/10.1186/s12886-018-0707-4.
Lu C-W, Tao Y, Li X-H, Dong Y, Zhou D-D. Fungal chorioretinitis with systemic candidiasis in an infant following treatment with broad spectrum antibiotics: a case report. ExpTher Med. 2017;14:286–8. https://doi.org/10.3892/etm.2017.4507.
• Pappas PG, Kauffman CA, Andes D, Benjamin DK, Calandra TF, Edwards JE, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 2009;48:503–535. https://doi.org/10.1086/596757Importance of dilated fundus examination in fungemia patients.
Toomey C, Gross A, Lee J, Spencer DB. A case of unilateral CoccidioidalChorioretinitis in a patient with HIV-associated meningoencephalitis. Case Rep Ophthalmol Med. 2019;1475628:1–3. https://doi.org/10.1155/2019/1475628.
Fowler B, Shen C, Mastellone J, Chaum E. Acute systemic histoplasmosis associated with chorioretinitis in an immunocompetent adolescent. Digit J Ophthalmol. 2011;17:31–5. https://doi.org/10.5693/djo.02.2011.07.002.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mycology
Rights and permissions
About this article
Cite this article
Rammohan, R., Suneetha, V., Sen, S. et al. Fungal Infections of the Eye. Curr Clin Micro Rpt 7, 39–50 (2020). https://doi.org/10.1007/s40588-020-00142-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40588-020-00142-8