Abstract
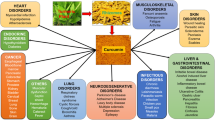
Curcumin is a natural product with many interesting pharmacological properties. However, these are offset by the particularly poor biopharmaceutical properties. The oral bioavailability of curcumin in humans is very low, mainly due to low solubility, poor stability, and extensive metabolism. This has led to multiple approaches to improve bioavailability, including administration of curcumin with metabolism inhibitors, formulation into nanoparticles, modification of the curcumin structure, and development of curcumin prodrugs. In this paper, we focus on the pharmacokinetic outcomes of these approaches. Pharmacokinetic parameters of curcumin after release from prodrugs are dependent on the linker between curcumin and the promoiety, and the release itself may depend on the physiological and enzymatic environment at the site of cleavage. This is an area in which more data are required for rational design of improved linkers. Cytotoxicity of curcumin prodrugs seems to correlate well with cellular uptake in vitro, but the in vivo relevance is uncertain. We conclude that improved experimental and theoretical models of absorption of curcumin prodrugs, development of accurate analytical methods for simultaneous measurement of plasma levels of prodrug and released curcumin, and acquisition of more pharmacokinetic data in animal models for dose prediction in humans are required to facilitate movement of curcumin prodrugs into clinical trials.
Similar content being viewed by others
References
El-Magboub A, et al. Biological targets and pharmacology of curcumin. In: Pouliquen DL, editor. Curcumin: synthesis, emerging role in pain management and health implications. Nova Science Publishers Inc: New York; 2014. p. 103–34.
Dona S, et al. Chemopreventive and chemotherapeutic potential of curcumin in breast cancer. Curr Drug Targets. 2012;13(14):1799–819.
Nautiyal J, et al. Combination of dasatinib and curcumin eliminates chemo-resistant colon cancer cells. J Mol Signal. 2011;6(1):1–11.
Begum AN, et al. Curcumin structure-function, bioavailability, and efficacy in models of neuroinflammation and alzheimer’s disease. J Pharmacol Exp Ther. 2008;326(1):196–208.
Ishrat T, et al. Amelioration of cognitive deficits and neurodegeneration by curcumin in rat model of sporadic dementia of Alzheimer’s type (SDAT). Eur Neuropsychopharm. 2009;19(9):636–47.
Nemmar A, Subramaniyan D, Ali BH. Protective effect of curcumin on pulmonary and cardiovascular effects induced by repeated exposure to diesel exhaust particles in mice. PLoS One. 2012;7(6):e39554.
Buadonpri W, et al. Synthetic curcumin inhibits carrageenan-induced paw edema in rats. J Health Res. 2009;23(1):11–6.
Chandran B, Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother Res. 2012;26(11):1719–25.
Chuengsamarn S, et al. Curcumin extract for prevention of type 2 diabetes. Diabetes Care. 2012;35(11):2121–7.
Gandapu U, et al. Curcumin-loaded apotransferrin nanoparticles provide efficient cellular uptake and effectively inhibit HIV-1 replication in vitro. PLoS One. 2011;6(8):e23388.
Dhillon N, et al. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res. 2008;14(14):4491–9.
Carvalho DDM, et al. Production, solubility and antioxidant activity of curcumin nanosuspension. Food Sci Technol (Campinas). 2015;35(1):115–9.
Wang YJ, et al. Stability of curcumin in buffer solutions and characterization of its degradation products. J Pharm Biomed Anal. 1997;15(12):1867–76.
Oetari S, et al. Effects of curcumin on cytochrome P450 and glutathione S-transferase activities in rat liver. Biochem Pharmacol. 1996;51(1):39–45.
Anand P, et al. Bioavailability of curcumin: problems and promises. Mol Pharmaceut. 2007;4(6):807–18.
Prasad S, Tyagi AK, Aggarwal BB. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: the golden pigment from golden spice. Cancer Res Treat. 2014;46(1):2–18.
Liu W, et al. Oral bioavailability of curcumin: problems and advancements. J Drug Target. 2016;24(8):694–702.
Wahlström B, Blennow G. A study on the fate of curcumin in the rat. Acta Pharmacol Toxicol. 1978;43(2):86–92.
Shoba G, et al. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998;64(4):353–6.
Safavy A, et al. Design and development of water-soluble curcumin conjugates as potential anticancer agents. J Med Chem. 2007;50(24):6284–8.
Ireson C, et al. Characterization of metabolites of the chemopreventive agent curcumin in human and rat hepatocytes and in the rat in vivo, and evaluation of their ability to inhibit phorbol ester-induced prostaglandin E2 production. Cancer Res. 2001;61(3):1058–64.
Ireson CR, et al. Metabolism of the cancer chemopreventive agent curcumin in human and rat intestine. Cancer Epidem Biomar. 2002;11(1):105–11.
Asai A, Miyazawa T. Occurrence of orally administered curcuminoid as glucuronide and glucuronide/sulfate conjugates in rat plasma. Life Sci. 2000;67(23):2785–93.
Metzler M, et al. Curcumin uptake and metabolism. BioFactors. 2013;39(1):14–20.
Rojsitthisak P, et al. Design, synthesis and biological activities of curcumin prodrugs. In: Pouliquen DL, editor. Curcumin: synthesis, emerging role in pain management and health implications. Nova Science Publishers Inc: New York; 2014. p. 135–76.
Dubey SK, et al. Design, synthesis and characterization of some bioactive conjugates of curcumin with glycine, glutamic acid, valine and demethylenated piperic acid and study of their antimicrobial and antiproliferative properties. Eur J Med Chem. 2008;43(9):1837–46.
Parvathy KS, Negi PS, Srinivas P. Curcumin–amino acid conjugates: synthesis, antioxidant and antimutagenic attributes. Food Chem. 2010;120(2):523–30.
Singh RK, et al. Synthesis, antibacterial and antiviral properties of curcumin bioconjugates bearing dipeptide, fatty acids and folic acid. Eur J Med Chem. 2010;45(3):1078–86.
Han YR, et al. A simple RP-HPLC method for the simultaneous determination of curcumin and its prodrug, curcumin didecanoate, in rat plasma and the application to pharmacokinetic study. Biomed Chromatogr. 2011;25(10):1144–9.
Wei XL, et al. Oily nanosuspension for long-acting intramuscular delivery of curcumin didecanoate prodrug: preparation, characterization and in vivo evaluation. Eur J Pharm Sci. 2013;49(2):286–93.
Wichitnithad W, et al. Synthesis, characterization and biological evaluation of succinate prodrugs of curcuminoids for colon cancer treatment. Molecules. 2011;16(2):1888–900.
Wongsrisakul J, et al. Antinociceptive effects of curcumin diethyl disuccinate in animal models. J Health Res. 2010;24(4):175–80.
Bangphumi K, et al. Pharmacokinetics of curcumin diethyl disuccinate, a prodrug of curcumin, in Wistar rats. Eur J Drug Metab Pharmacokinet. 2015;1–9.
Tang H, et al. Amphiphilic curcumin conjugate-forming nanoparticles as anticancer prodrug and drug carriers: in vitro and in vivo effects. Nanomedicine. 2010;5(6):855–65.
Bhunchu S, Rojsitthisak P, Rojsitthisak P. Effects of preparation parameters on the characteristics of chitosan–alginate nanoparticles containing curcumin diethyl disuccinate. J Drug Deliv Sci Technol. 2015;28:64–72.
Sarika PR, et al. Galactosylated pullulan–curcumin conjugate micelles for site specific anticancer activity to hepatocarcinoma cells. Colloids Surf B Biointerfaces. 2015;133:347–55.
Yan L, et al. Targeted delivery of macromolecular drugs: asialoglycoprotein receptor (ASGPR) expression by selected hepatoma cell lines used in antiviral drug development. Curr Drug Deliv. 2008;5(4):299–302.
Li J, et al. Modified curcumin with hyaluronic acid: combination of pro-drug and nano-micelle strategy to address the curcumin challenge. Food Res Int. 2015;69:202–8.
Dey S, Sreenivasan K. Conjugation of curcumin onto alginate enhances aqueous solubility and stability of curcumin. Carbohydr Polym. 2014;99:499–507.
Sarika PR, et al. Gum arabic-curcumin conjugate micelles with enhanced loading for curcumin delivery to hepatocarcinoma cells. Carbohydr Polym. 2015;134:167–74.
Wang Z, et al. Tuning the architecture of polymeric conjugate to mediate intracellular delivery of pleiotropic curcumin. Eur J Pharm Biopharm. 2015;90:53–62.
Li M, et al. Acetal-linked polymeric prodrug micelles for enhanced curcumin delivery. Colloids Surf B Biointerfaces. 2016;140:11–8.
Yang R, et al. Biodegradable polymer-curcumin conjugate micelles enhance the loading and delivery of low-potency curcumin. Pharm Res. 2012;29(12):3512–25.
Waghela BN, et al. Curcumin conjugated with PLGA potentiates sustainability, anti-proliferative activity and apoptosis in human colon carcinoma cells. PLoS One. 2015;10(2):e0117526.
Cai Y, et al. Synthesis, characterization and anti-cancer activity of Pluronic F68–curcumin conjugate micelles. Drug Deliv 2015;1–9.
Fang XB, et al. pH-sensitive micelles based on acid-labile pluronic F68–curcumin conjugates for improved tumor intracellular drug delivery. Int J Pharm. 2016;502(1–2):28–37.
Grill AE, Koniar B, Panyam J. Co-delivery of natural metabolic inhibitors in a self-microemulsifying drug delivery system for improved oral bioavailability of curcumin. Drug Deliv Transl Res. 2014;4(4):344–52.
Ahmad MZ, et al. Progress in nanotechnology-based drug carrier in designing of curcumin nanomedicines for cancer therapy: current state-of-the-art. J Drug Target. 2016;24(4):273–93.
Rungphanichkul N, et al. Preparation of curcuminoid niosomes for enhancement of skin permeation. Pharmazie. 2011;66(8):570–5.
Khalil NM, et al. Pharmacokinetics of curcumin-loaded PLGA and PLGA–PEG blend nanoparticles after oral administration in rats. Colloids Surf B Biointerfaces. 2013;101:353–60.
Reid JM, et al. Mouse pharmacokinetics and metabolism of the curcumin analog, 4-piperidinone, 3,5-bis[(2-fluorophenyl)methylene]-acetate(3E,5E) (EF-24; NSC 716993). Cancer Chemother Pharmacol. 2014;73(6):1137–46.
Alok V, et al. Perspectives on new synthetic curcumin analogs and their potential anticancer properties. Curr Pharm Des. 2013;19(11):2047–69.
Zhou L and Wang J. Physico-chemical characterization in drug discovery. Trends in bio/pharmaceutical industry. Preclinical formulation. 2009;12–18
Wichitnithad W, et al. Effects of different carboxylic ester spacers on chemical stability, release characteristics, and anticancer activity of mono-PEGylated curcumin conjugates. J Pharm Sci. 2011;100(12):5206–18.
Manju S, Sreenivasan K. Synthesis and characterization of a cytotoxic cationic polyvinylpyrrolidone–curcumin conjugate. J Pharm Sci. 2011;100(2):504–11.
Li AP. Screening for human ADME/Tox drug properties in drug discovery. Drug Discov Today. 2001;6(7):357–66.
van Breemen RB, Li Y. Caco-2 cell permeability assays to measure drug absorption. Expert Opin Drug Metab Toxicol. 2005;1(2):175–85.
Liederer BM, Borchardt RT. Enzymes involved in the bioconversion of ester-based prodrugs. J Pharm Sci. 2006;95(6):1177–95.
Yang YH, et al. Enzyme-mediated hydrolytic activation of prodrugs. Acta Pharm Sin B. 2011;1(3):143–59.
Fukami T, Yokoi T. The emerging role of human esterases. Drug Metab Pharmacokinet. 2012;27(5):466–77.
Bahar FG, et al. Species difference of esterase expression and hydrolase activity in plasma. J Pharm Sci. 2012;101(10):3979–88.
Li W, Zhang J, Tse FLS. Strategies in quantitative LC-MS/MS analysis of unstable small molecules in biological matrices. Biomed Chromatogr. 2011;25(1–2):258–77.
Li W, et al. LC-MS bioanalysis of ester prodrugs and other esterase labile molecules. In: Li W, Zhang J and Tse FLS (eds.) Handbook of LC-MS Bioanalysis. Wiley; 2013. pp. 429–445.
Zeng J, et al. Simultaneous determination of a selective adenosine 2A agonist, BMS-068645, and its acid metabolite in human plasma by liquid chromatography-tandem mass spectrometry—evaluation of the esterase inhibitor, diisopropyl fluorophosphate, in the stabilization of a labile ester-containing drug. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;852(1–2):77–84.
Fung EN, et al. Effective screening approach to select esterase inhibitors used for stabilizing ester-containing prodrugs analyzed by LC–MS/MS. Bioanalysis. 2010;2(4):733–43.
Ratnatilaka Na Bhuket P, et al. Simultaneous determination of curcumin diethyl disuccinate and its active metabolite curcumin in rat plasma by LC–MS/MS: application of esterase inhibitors in the stabilization of an ester-containing prodrug. J Chromatogr B Analyt Technol Biomed Life Sci. 2016;1033–1034:301–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this manuscript was supported by the Annual Research Fund of the Faculty of Pharmaceutical Sciences, Chulalongkorn University (P. Rojsitthisak), the Ratchadapiseksompoch Endowment Fund of Chulalongkorn University (CU-58-003-HR and CU-59-031-AM) (P. Rojsitthisak), the National Research University Project, Office of Higher Education Commission (NRU59-047-AM) (P. Rojsitthisak) and the scholarship from the Graduate School, Chulalongkorn University to commemorate the 72nd anniversary of his Majesty King Bhumibala Aduladeja (P. Ratnatilaka Na Bhuket).
Conflicts of interest
Pahweenvaj Ratnatilaka Na Bhuket, Asma El-Magboub, Ian S. Haworth and Pornchai Rojsitthisak declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ratnatilaka Na Bhuket, P., El-Magboub, A., Haworth, I.S. et al. Enhancement of Curcumin Bioavailability Via the Prodrug Approach: Challenges and Prospects. Eur J Drug Metab Pharmacokinet 42, 341–353 (2017). https://doi.org/10.1007/s13318-016-0377-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-016-0377-7