Abstract
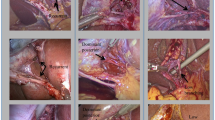
Bile duct injury remains the most serious complication of laparoscopic cholecystectomy (LC), the main cause was misidentification of cystic duct (CD). The aim of this study was to evaluate the effectiveness and security of retrograde tracing along “cystic duct” (RTACD) method for the prevention of biliary misidentification injury in LC. The conception of RTACD method was first described and then illustrated by simulation dissection with extrahepatic biliary structure charts. A total of 840 patients undergoing LC were selected. After the “CD” was separated during operation, its authenticity was identified by RTACD method according to its course and origin. The “CD” can be clipped/divided only when it was identified to be true CD. Among 840 patients, the initially separated “CD” was identified as actual CD in 831 cases, common hepatic (bile) duct in six cases, accessory right posterior sectoral duct in two cases, and right haptic duct in one case. LCs were successfully finished in 837 patients, and converted to open cholecystectomy in three cases. The average operation time was 64.23 min (range 25–225 min), and the average blood loss was 8.07 ml (range 2–200 ml). No biliary misidentification injury was found. All patients recovered smoothly. No jaundice or abdominal pain was noted in the patients during 1–19 months follow-up. RTACD method is a safe and effective new technique of preventing biliary misidentification injury.


Similar content being viewed by others
References
Go PM, Schol F, Gouma DJ (1993) Laparoscopic cholecystectomy in the Netherlands. Br J Surg 80(9):1180–1183
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(1):101–125
Archer SB, Brown DW, Smith D et al (2001) Bile duct injury during laparoscopic cholecystectomy. Results of a national survey. Ann Surg 234(4):549–558
Way LW, Stewart L, Wet G et al (2003) Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg 237(4):460–469. https://doi.org/10.1097/01.SLA.0000060680.92690.E9
Strasberg SM (2005) Biliary injury in laparoscopic surgery: part 1. Processes used in determination of standard of care in misidentification injuries. J Am Coll Surg 201(4):598–603
Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparo-scopic cholecystectomy. J Am Coll Surg 211(1):132–138. https://doi.org/10.1016/j.jamcollsurg.2010.02.053
Hori T, Oike F, Furuyama H, Machimoto T et al (2016) Protocol for laparoscopic cholecystectomy: is it rocket science? World J Gastroenterol 22(47):10287–10303. https://doi.org/10.3748/wjg.v22.i47.10287
Strasberg SM, Eagon CJ, Drebin JA (2000) The “hidden cystic duct” syndrome and the infundibular technique of laparoscopic cholecystectomy—the danger of the false infundibulum. J Am Coll Surg 191(6):661–667
Strasberg SM (2002) Avoidance of biliary injury during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg 9(5):543–547. https://doi.org/10.1007/s005340200071
Dekker SW, Hugh TB (2008) Laparoscopic bile duct injury: understanding the psychology and heuristics of the error. ANZ J Surg 78:1109–1114. https://doi.org/10.1111/j.1445-2197.2008.04761.x
Callery MP (2006) Avoiding biliary injury during laparoscopic cholecystectomy: technical considerations. Surg Endosc 20(11):1654–1658. https://doi.org/10.1007/s00464-006-0488-3
Nijssen MA, Schreinemakers JM, van der Schelling GP et al (2016) Improving critical view of safety in laparoscopic cholecystectomy by teaching Interventions. J Surg Educ 73(3):442–447. https://doi.org/10.1016/j.jsurg.2015.11.015
Alvarez FA, de Santibañes M, Palavecino M et al (2014) Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury. Br J Surg 101(6):677–684. https://doi.org/10.1002/bjs.9486
Törnqvist B, Strömberg C, Akre O et al (2015) Selective intraoperative cholangiography and risk of bile duct injury during cholecystectomy. Br J Surg 102(8):952–958. https://doi.org/10.1002/bjs.9832
Wakabayashi G, Iwashita Y, Hibi T et al (2018) Tokyo guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 25(1):73–86. https://doi.org/10.1002/jhbp.517
Conrad C, Wakabayashi G, Asbun HJ et al (2017) IRCAD recommendation on safe laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci 24(11):603–615. https://doi.org/10.1002/jhbp.491
Hunter JG (1991) Avoidance of bile duct injury during laparoscopic cholecystectomy. Am J Surg 162(1):71–76
Cai XJ, Ying HN, Yu H et al (2015) Blunt dissection: a solution to prevent bile duct injury in laparoscopic cholecystectomy. Chin Med J (Engl) 128(23):3153–3157. https://doi.org/10.4103/0366-6999.170270
Avgerinos C, Kelgiorgi D, Touloumis Z et al (2009) One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg 13(3):498–503. https://doi.org/10.1007/s11605-008-0748-8
Honda G, Hasegawa H, Umezawa A (2016) Universal safe procedure of laparoscopic cholecystectomy standardized by exposing the inner layer of the subserosal layer (with video). J Hepatobiliary Pancreat Sci 23(9):E14–19. https://doi.org/10.1002/jhbp.382
Gupta V, Jain G (2019) Safe laparoscopic cholecystectomy: adoption of universal culture of safety in cholecystectomy. World J Gastrointest Surg 11(2):62–84. https://doi.org/10.4240/wjgs.v11.i2.62
Strasberg SM (2005) Biliary injury in laparoscopic surgery: part 2. Changing the culture of cholecystectomy. J Am Coll Surg 201(4):604–611. https://doi.org/10.1016/j.jamcollsurg.2005.04.032
Strasberg SM (2017) A perspective on the critical view of safety in laparoscopic cholecystectomy. Ann Laparosc Endosc Surg 2:91–94. https://doi.org/10.1002/jhbp.616
Yegiyants S, Collins JC (2008) Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg 74(10):985–987
Dziodzio T, Weiss S, Sucher R et al (2014) A ‘critical view’ on a classical pitfall in laparoscopic cholecystectomy. Int J Surg Case Rep 5(12):1218–1221. https://doi.org/10.1016/j.ijscr.2014.11.018
Strasberg SM (2008) Error traps and vasculo-biliary injury in laparoscopic and open cholecystectomy. J Hepatobiliary Pancreat Surg 15(3):284–292. https://doi.org/10.1007/s00534-007-1267-9
Giger U, Ouaissi M, Schmitz SF et al (2011) Bile duct injury and use of cholangiography during laparoscopic cholecystectomy. Br J Surg 98(3):391–396. https://doi.org/10.1002/bjs.7335
Carroll BJ, Friedman RL, Liberman MA et al (1996) Routine cholangiography reduces sequelae of common bile duct injuries. Surg Endosc 10(12):1194–1197
Acknowledgements
We are grateful to all surgeons, First Department of Hepatobiliary Surgery, Yijishan Hospital of Wannan Medical College, for their contribution to operation and data collection. We thank Dr. G. Feng, Department of Clinical Laboratory, Yijishan Hospital of Wannan Medical College, for critically revising the manuscript.
Funding
This study was supported by the Key Research and Development Program of Anhui Province, China (No. 1804h08020273).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no potential conflict of interest.
Research involving human participants and/or animals
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, X., Cheng, B., Wang, D. et al. Retrograde tracing along “cystic duct” method to prevent biliary misidentification injury in laparoscopic cholecystectomy. Updates Surg 72, 137–143 (2020). https://doi.org/10.1007/s13304-020-00716-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00716-7