Abstract
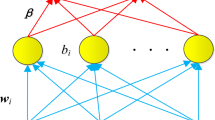
In digital mammography, which is used for the early detection of breast tumors, oversight may occur due to overlap between normal tissues and lesions. However, since digital breast tomosynthesis can acquire three-dimensional images, tissue overlapping is reduced, and, therefore, the shape and distribution of the lesions can be easily identified. However, it is often difficult to distinguish between benign and malignant breast lesions on images, and the diagnostic accuracy can be reduced due to complications from radiological interpretations, owing to acquisition of a higher number of images. In this study, we developed an automated classification method for diagnosing breast lesions on digital breast tomosynthesis images using radiomics to comprehensively analyze the radiological images. We extracted an analysis area centered on the lesion and calculated 70 radiomic features, including the shape of the lesion, existence of spicula, and texture information. The accuracy was compared by inputting the obtained radiomic features to four classifiers (support vector machine, random forest, naïve Bayes, and multi-layer perceptron), and the final classification result was obtained as an output using a classifier with high accuracy. To confirm the effectiveness of the proposed method, we used 24 cases with confirmed pathological diagnosis on biopsy. We also compared the classification results based on the presence or absence of dimension reduction using least absolute shrinkage and a selection operator (LASSO). As a result, when the support vector machine was used as a classifier, the correct identification rate of the benign tumors was 55% and that of malignant tumors was 84%, with best results. These results indicate that the proposed method may help in more accurately diagnosing cases that are difficult to classify on images.







Similar content being viewed by others
References
NIH: Cancer Statistics: Reports on Cancer: Cancer Stat Facts: Female Breast Cancer, 2015. https://seer.cancer.gov/statfacts/html/breast.html. Accessed Feb 2019.
Lee A, Mavaddat N, Wilcox A, et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med. 2019;21(8):1708–18.
Sardanelli F, Aase HS, Alvarez M, Azavedo E. Position paper on screening for breast cancer by the European Society of Breast Imaging (EUSOBI) and 30 national breast radiology bodies. Eur Radiol. 2017;27(7):2737–43.
Roth RG, Maidment AD, Weinstein SP, Roth SO, Conant EF. Digital breast tomosynthesis: lessons learned from early clinical implementation. Radiographics. 2014;34:E89–E102.
Carney PA, Miglioretti DL, Yankaskas BC, et al. Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med. 2003;138(3):168–75.
Niklason LT, Christian BT, Niklason LE, et al. Digital tomosynthesis in breast imaging. Radiology. 1997;205(2):399–406.
Rafferty EA, Park JM, Philpotts LE, et al. Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology. 2016;266(1):104–13.
Skaane P, Bandos AI, Gullien R, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267(1):47–56.
Gur D, Abrams GS, Chough DM, et al. Digital breast tomosynthesis: observer performance study. AJR Am J Roentgenol. 2009;193(2):586–91.
Gennaro G, Toledano A, di Maggio C, et al. Digital breast tomosynthesis versus digital mammography: a clinical performance study. Eur Radiol. 2010;20(7):1545–53.
John M. Core-needle biopsy for breast abnormalities. AHRQ Pub. No.14(16)-EHC040-3-EF; 2016.
Bhattacharyya D, Bandyopadhyay S, Kim T. Diagnosis of breast cancer by tissue analysis. Chin J Cancer Res. 2013;25(1):39–45.
Yamazaki M, Teramoto A, Fujita H. A hybrid detection scheme of architectural distortion in mammograms using iris filter and Gabor filter. Lect Comput Sci. 2016;9699:174–82.
Jiang Y, Jiang Y, Nishikawa RM, et al. Improving breast cancer diagnosis with computer-aided diagnosis. Acad Radiol. 1999;6(1):22–33.
Christoyianni I, Koutras A, Dermatas E, Kokkinakis G. Computer aided diagnosis of breast cancer in digitized mammograms. Comput Med Imaging Gr. 2002;26(5):309–19.
Eltoukhy M, Faye I, Samir B. A statistical based feature extraction method for breast cancer diagnosis in digital mammogram using multiresolution representation. Comput Biol Med. 2012;42(1):123–8.
LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521(7553):436–44.
Krizhevsky A, Sutskever I, Hinton GE. ImageNet classification with deep convolutional neural networks. Adv Neurol. 2012;25(6):1106–14.
Ragab D, Sharkas M, Marshall S, Ren J. Breast cancer detection using deep convolutional neural networks and support vector machines. PeerJ. 2019;7(2601):1–23.
Arevalo J, González F, Ramos-Pollán R. Convolutional neural networks for mammography mass lesion classification. In: 37th Annual international conference of the IEEE engineering in medicine and biology society (EMBC); 2015, pp 797–800.
Tian J, Dong D, Liu Z et al. Radiomics in medical imaging-detection, extraction and segmentation. In: Artificial Intelligence in Decision Support Systems for Diagnosis in Medical Imaging. Intelligent Systems Reference Library, vol 140; 2018.
Parmar C, Velazquez E, Leijenaar R, et al. Robust radiomics feature quantification using semiautomatic volumetric segmentation. PLoS ONE. 2014;9(7):1–8.
Ma J, Wang Q, Ren Y, et al. Automatic lung nodule classification with radiomics approach. In: Proceedings of SPIE 9789, medical imaging 2016: PACS and imaging informatics: next generation and innovations, 978906; 2016.
Song Q, Zhao L, Luo X, et al. Using deep learning for classification of lung nodules on computed tomography images. J Healthc Eng. 2017;2017:7.
Hologic's public data. https://www.dclunie.com/pixelmedimagearchive/upmcdigitalmammotomocollection/index.html. Accessed Nov 2018.
American College of Radiology. Breast imaging reporting and data system (BI-RADS®). 3rd ed. Reston: American College of Radiology; 1998.
Rangayyan RM, Ayres FJ. Gabor filter and phase portraits for the detection of architectural distortion in mammograms. Med Biol Eng Comput. 2006;44(10):883–94.
Li Q, Sone S, Doi K. Selective enhancement filters for nodules, vessels, and airway walls in two and three-dimensional CT scans. Med Phys. 2003;30(8):2040–51.
Teramoto A, Fujita H, Yamamuro O, Tamaki T. Automated detection of pulmonary nodules in PET/CT images: ensemble false-positive reduction using a convolutional neural network technique. Med Phys. 2016;43(6):2821–7.
Teramoto A, Tsujimoto M, Inoue T, et al. Automated classification of pulmonary nodules through a retrospective analysis of conventional CT and two-phase PET images in patients undergoing biopsy. Asia Ocean J Nucl Med Biol. 2018;7(1):29–37.
Yoshikawa R, Teramoto A, Matsubara T, Fujita H. Automated detection of architectural distortion using improved adaptive Gabor filter. International workshop on digital mammography. Cham: Springer; 2014. p. 606–611.
Selvarajah S, Kodituwakku S. Analysis and comparison of texture features for content based image retrieval. Int J Latest Trends Comput. 2011;2(1):108–13.
Carlson J. ‘Radiomic' Image Processing Toolbox. https://cran.r-project.org/web/packages/radiomics/radiomics.pdf. Accessed Nov 2018.
Zhou Y, He L, Huang Y, et al. CT-based radiomics signature: a potential biomarker for preoperative prediction of early recurrence in hepatocellular carcinoma. Abdom Radiol. 2017;42(6):1695–704.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
Filzmoser P, Liebmann B, Varmuza K. Repeated double cross validation. J Cemometrics. 2009;23:160–71.
Leijenaar RTH, Carvalho S, Velazquez ER, van Elmpt WJC, Parmar C, Hoekstra OS, Hoekstra CJ, Boellaard R, Dekker ALAJ, Gillies RJ, Aerts HJWL, Lambin P. Stability of FDGPET radiomics features: an integrated analysis of test–retest and inter-observer variability. Acta Oncol. 2013;52(7):1391–7.
Teramoto A, Yamada A, Kiriyama Y, Tsukamoto T, Yan K, Zhang L, Imaizumi K, Saito K, Fujita H. Automated classification of benign and malignant cells from lung cytological images using deep convolutional neural network. Informatics in Medicine Unlocked. 2019;16:100205.
Onishi Y, Teramoto A, Tsujimoto M, et al. Automated pulmonary nodule classification in computed tomography images using a deep convolutional neural network trained by generative adversarial networks. BioMed Res Int. 2019;2019:1–9 (Article ID 6051939).
Acknowledgements
We are grateful to Ms. Tomoko Otsuka of Daido Hospital for annotation of clinical data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All the procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The present article does not contain any studies performed on animals by any of the authors.
Informed consent
Consent from the patients was obtained with a condition that all data were anonymized.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sakai, A., Onishi, Y., Matsui, M. et al. A method for the automated classification of benign and malignant masses on digital breast tomosynthesis images using machine learning and radiomic features. Radiol Phys Technol 13, 27–36 (2020). https://doi.org/10.1007/s12194-019-00543-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-019-00543-5