Abstract
Objective
To evaluate the effect of maternal iron deficiency anemia (IDA) on fetal thrombopoiesis.
Methods
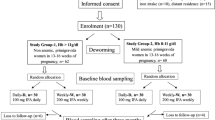
In this prospective observational study, maternal and cord blood iron status parameters (serum iron, serum ferritin, total iron-binding capacity, and transferrin saturation), and platelet indices, such as, absolute platelet count (APC), mean platelet volume (MPV), platelet distribution width (PDW) and plateletcrit, were estimated in a convenient sample of 142 mothers with IDA (hemoglobin <11 g/dl and serum ferritin <12 ng/ml) and an equal number of healthy non-anemic (hemoglobin ≥11 g/dl) mothers, who delivered singleton live neonates at term gestation. Mothers with antenatal thrombocytopenia, infections, inflammatory conditions, pregnancy-induced hypertension and neonates with perinatal asphyxia, sepsis and congenital malformations were excluded.
Results
For statistical analysis, the IDA group was further subdivided into mild-to-moderate (hemoglobin 7–10.9 g/dl) and severe (hemoglobin <7 g/dl) anemia. Cord blood APC and PDW were comparable between non-anemic and mild-to-moderate anemic mothers (242,550 ± 54,320/μL vs. 235,260 ± 34,620/μL for APC and 16.2 ± 1.4 vs. 16.4 ± 1.8 fl for PDW, respectively), but in severe IDA group, cord blood APC and PDW were significantly lower (74,520 ± 12,380/μL and 17.8 ± 2.1 fl, respectively, p < 0.001). MPV and plateletcrit were comparable. None of the study neonates had a platelet count <30,000/μL or showed any evidence of clinical bleeding.
Conclusions
Neonates born to mothers with severe IDA had moderate thrombocytopenia with increased PDW, though no change was observed in MPV and plateletcrit. Further studies should be carried out to identify the cause and consequences of this observation.
Similar content being viewed by others
References
McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. 2009;12:444–54.
Pasricha SR, Drakesmith H, Black J, Hipgrave D, Biggs BA. Control of iron deficiency anemia in low- and middle-income countries. Blood. 2013;121:2607–17.
Young MF, Griffin I, Pressman E, et al. Maternal hepcidin is associated with placental transfer of iron derived from dietary heme and nonheme sources. J Nutr. 2012;142:33–9.
Siddappa AM, Rao R, Long JD, Widness JA, Georgieff MK. The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations. Neonatology. 2007;92:73–82.
Kumar A, Rai AK, Basu S, Dash D, Singh JS. Cord blood and breast milk iron status in maternal anemia. Pediatrics. 2008;121:e673–7.
Adediran A, Gbadegesin A, Adeyemo TA, et al. Cord blood haemoglobin and ferritin concentrations in newborns of anaemic and non-anaemic mothers in Lagos, Nigeria. Niger Med J. 2013;54:22–6.
Kuku I, Kaya E, Yologlu S, Gokdeniz R, Baydin A. Platelet counts in adults with iron deficiency anemia. Platelets. 2009;20:401–5.
Perlman MK, Schwab JG, Nachman JB, Rubin CM. Thrombocytopenia in children with severe iron deficiency. J Pediatr Hematol Oncol. 2002;24:380–4.
Mokhtar GM, Ibrahim WE, Kassim NA, Ragab IA, Saad AA, Abdel Raheem HG. Alterations of platelet functions in children and adolescents with iron-deficiency anemia and response to therapy. Platelets. 2014;15:1–5.
Yıldırım ZK, Orhan MF, Büyükavcı M. Platelet function alterations and their relation to P-selectin (CD62P) expression in children with iron deficiency anemia. Blood Coagul Fibrinolysis. 2011;22:98–101.
Ballard JL, Khoury JC, Wedling K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard score expanded to include premature infants. J Pediatr. 1991;119:417–23.
Park MJ, Park PW, Seo YH, et al. The relationship between iron parameters and platelet parameters in women with iron deficiency anemia and thrombocytosis. Platelets. 2013;24:348–51.
Kadikoylu G, Yavasoglu I, Bolaman Z, Senturk T. Platelet parameters in women with iron deficiency anemia. J Natl Med Assoc. 2006;98:398–402.
Chakravorty S, Murray N, Roberts I. Neonatal thrombocytopenia. Early Hum Dev. 2005;81:35–41.
Roberts I, Murray NA. Neonatal thrombocytopenia. Semin Fetal Neonatal Med. 2008;13:256–64.
Maruyama H, Shinozuka M, Kondoh Y, et al. Thrombocytopenia in preterm infants with intrauterine growth restriction. Acta Med Okayama. 2008;62:313–7.
Stanworth SJ. Thrombocytopenia, bleeding, and use of platelet transfusions in sick neonates. Hematol Am Soc Hematol Educ Program. 2012;2012:512–6.
Sola-Visner M. Platelets in the neonatal period: developmental differences in platelet production, function, and hemostasis and the potential impact of therapies. Hematol Am Soc Hematol Educ Program. 2012;2012:506–11.
Wang X, Mendelsohn L, Rogers H, et al. Heme-bound iron activates placenta growth factor in erythroid cells via erythroid Krüppel-like factor. Blood. 2014;124:946–54.
Guida JD, Kunig AM, Leef KH, McKenzie SE, Paul DA. Platelet count and sepsis in very low birth weight neonates: is there an organism-specific response? Pediatrics. 2003;111:1411–5.
Catal F, Tayman C, Tonbul A, et al. Mean platelet volume (MPV) may simply predict the severity of sepsis in preterm infants. Clin Lab. 2014;60:1193–200.
Bhat MA, Bhat JI, Kawoosa M, Ahmad S, Ali S. Organism-specific platelet response and factors affecting survival in thrombocytopenic very low birth weight babies with sepsis. J Perinatol. 2009;29:702–8.
Manzoni P, Mostert M, Galletto P, et al. Is thrombocytopenia suggestive of organism-specific response in neonatal sepsis? Pediatr Int. 2009;51:206–10.
Eissa DS, El-Farrash RA. New insights into thrombopoiesis in neonatal sepsis. Platelets. 2013;24:122–8.
Gao Y, Li Y, Yu X, et al. The impact of various platelet indices as prognostic markers of septic shock. PLoS One. 2014;9:e103761.
Acknowledgments
The authors would like to thank all the residents who managed the neonates and all the mother-infant pairs who were included in the study.
Contributions
SB: Conceptualization and design of the study, collection of data, patient management, critical literature review and drafting of the manuscript; NK: Concept and study design, collection of samples, patient management, literature review and drafting of the manuscript; RS: Concept and study design, biochemical analysis of samples, literature review and drafting of the manuscript; AK: Concept and study design, patient management, critical literature review and drafting of the manuscript. All authors have approved the final version of the manuscript. SB will act as guarantor for this paper.
Conflict of Interest
None.
Source of Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Basu, S., Kumar, N., Srivastava, R. et al. Effect of Severe Maternal Iron Deficiency Anemia on Neonatal Platelet Indices. Indian J Pediatr 82, 1091–1096 (2015). https://doi.org/10.1007/s12098-015-1775-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-015-1775-6