Abstract
Purpose
Historically, thoracic malignancies, such as non-small cell lung cancer and malignant pleural mesothelioma, have been marked by poor prognosis. Current standard of care for these diseases results in limited improvements in survival benefit. This has prompted researchers to explore new and innovative treatment alternatives. Immunotherapy is an emerging therapeutic modality that harnesses the power of the human immune system against cancer cells. Herein, we summarize the concepts and current status of immunotherapy for the treatment of thoracic malignancies.
Methods
Using ClinicalTrials.gov, we conducted a literature review using the terms “immunotherapy” and “immune therapy,” and combined them with the conditions “pleural mesothelioma” and “carcinoma, non-small cell lung.” The search results yielded 452 trials, among which 122 trials met our specific criteria.
Results
Our search identified immune checkpoint blockade, immunotoxin therapy, anticancer vaccines, and adoptive cell therapy as the most common and relevant immunotherapies that are currently being assessed in clinical trials.
Conclusion
We have highlighted the successes, as well as the limitations, of immunotherapy for non-small cell lung cancer and malignant pleural mesothelioma. We have identified early phase clinical trials that assess immunotherapy as first-line, second-line, and maintenance therapy, and compared these drugs as monotherapeutics or in combination with chemotherapy or other types of immunotherapy.
Similar content being viewed by others
Introduction
Epidemiology of thoracic malignancies
Thoracic malignancies are a major health concern worldwide. Traditionally, lung cancer has been divided into two groups, non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC consists of different subtypes—squamous cell carcinoma, adenocarcinoma, and large cell carcinoma—and it accounts for 85% of newly diagnosed cases of lung cancer [1]. Lung cancer is the most frequently diagnosed cancer in men and the third most frequently diagnosed cancer in woman worldwide and, in developed countries, it is the leading cause of cancer-related death for both men and woman [2]. This is due largely to the fact that the majority (70%) of patients diagnosed with NSCLC have tumors that are advanced and unresectable [3]. Because of this, there has been marginal improvement over the past several decades with 5-year survival rates that only range from 10 to 20% and median survival of approximately 12 months [2].
Malignant pleural mesothelioma (MPM) is an aggressive cancer of the pleura. The most common etiology is asbestos exposure and, while the use of the silicate mineral has been banned in most developed countries, it is still mined and manufactured in many developing countries [4]. The global incidence of MPM is likely underreported and it is estimated to peak in the late 2020s [5]. Similar to NSCLC, MPM has a poor prognosis that may be secondary to the difficulties in early diagnosis and the advanced stage of the disease at time of diagnosis. Without treatment, median survival is 12 months and with treatment the 6-month, 1-year, and 5-year overall survival (OS) rates are 55, 33, and 5%, respectively [6].
Currently established therapy
The prevalence and aggressiveness of these two conditions clearly underscores the importance of discovering and implementing new and innovative therapies. It is important to briefly describe the current standards of care before discussing future therapeutic interventions.
For many years, the standard of care for advanced NSCLC was platinum-based doublet chemotherapy; however, this treatment offered only small improvements in survival compared with supportive care [7]. Discoveries of tumor-specific mutations in NSCLC have led to the development of targeted therapies that inhibit specific molecular pathways for lung cancer. For example, gefitinib is a tyrosine kinase inhibitor (TKI) that targets epidermal growth factor receptor (EGFR). When used as a monotherapy, approximately 70% of patients with EGFR mutations had a radiographic response [8]. Despite this positive result, responsiveness was seen typically in a distinct patient population—women, no smoking history, and of Asian descent—and the majority of responders developed acquired resistance [8]. Subsequently, additional TKIs and monoclonal antibodies (mAbs) have been developed to target EGFR and other driver mutations (e.g., VEGF and cMET), and have shown promising, yet modest, results. Nonetheless, these therapies have been effective in only a minority of NSCLC patients.
For MPM, systemic chemotherapy is a standard component in the treatment of patients with resectable or unresectable disease. A phase III trial (EMPHACIS) of 456 patients demonstrated a 3-month survival benefit (12.1 vs. 9.3 months) in patients who were treated with pemetrexed and cisplatin combination therapy as opposed to cisplatin alone [9]. Surgical resection for MPM is a controversial subject with no established guidelines. Furthermore, there has been considerable debate about the optimal role of surgery given the high morbidity associated with these complicated surgical interventions. Extrapleural pneumonectomy (EPP) entails en bloc resection of the visceral and parietal pleura, pericardium, ipsilateral hemidiaphragm, and lung; this is the most extensive intervention for MPM. The MARS trial compared patients treated using EPP with those who were not treated using EPP. The investigators of this trial concluded that EPP offers no added benefit and may possibly harm patients [10]. Conversely, cytoreductive, lung-sparing procedures, such as pleurectomy/decortication and extended pleurectomy/decortication, are associated with improved survival rates, albeit, at the cost of higher morbidity than supportive care [11].
The goal of surgical resection is the removal of macroscopic disease (R1 resection). Radiation therapy has been employed in an adjuvant setting to control microscopic disease, but is associated with toxicity in the lungs and adjacent organs [12]. To counteract this, clinicians have employed innovative techniques such as intensity-modulated pleural radiation therapy (IMPRINT). IMPRINT targets pleural surfaces while limiting lung exposure. Studies have shown that this is safe as there have been no episodes of grade 4 or 5 radiation pneumonitis [13]. Despite this, chemotherapy, surgery, and radiation have proven to be ineffective as solitary therapy. The advent of trimodality therapy, which is the combination of the aforementioned three therapies, has resulted in less morbidity and mortality at high patient volume treatment centers. But, completion of trimodality therapy can be difficult due to disease progression, treatment side effects, and limited access to high volume centers [14].
The high recurrence rate, development of resistance to targeted therapies for NSCLC, and the challenges associated with delivery of trimodality therapy for MPM are only some of the hurdles that drive researchers toward the development of innovative and efficacious therapies for these deadly diseases. One such innovative therapy is immunotherapy, an emerging therapeutic modality that harnesses the power of the human immune system against cancer cells.
Immunoediting and immunotherapy
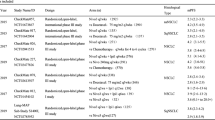
The theory of immunosurveillance states that a healthy immune system can protect an individual from the development and uncontrolled growth of malignancies [15]. Immunoediting is the theory that explains how an immunocompetent host develops cancer and is divided into three phases—elimination, equilibrium, and escape [15]. Elimination entails activation of the host immune mechanisms that results in apoptosis of tumor cells. If this process is unsuccessful, tumor cells may enter the equilibrium phase where tumor growth is maintained chronically. Alternatively, tumor cells may adapt to the immune microenvironment and develop tumor variants. If these variants overcome host immunity, they enter the escape phase and become the clinically detectable lesions that lead to the physical symptoms of cancer that are manifested by the host [15]. Immunotherapy is designed to counteract these evasive techniques that are employed by the tumor cell. In this review we will provide an overview of various immunotherapeutic strategies and discuss the results of select clinical trials (Fig. 1) of patients with NSCLC and MPM.
Using ClinicalTrials.gov, we searched the terms “immunotherapy” and “immune therapy,” and combined them with the conditions “pleural mesothelioma” and “carcinoma, non-small cell lung.” We excluded all closed trials and trials that resulted from multiple search terms (overlapping). We then screened 169 trials and excluded trials that tested non-immunotherapy medications, non-therapeutic trials (e.g., biomarker studies), trials where radiation/energy was the primary intervention, and radiologic studies.
Checkpoint blockade
As previously mentioned, during the equilibrium phase tumor cells adapt to the tumor immune microenvironment. One method of adaptation is the upregulation of inhibitory ligands on the surface of tumor cells. These ligands interact with inhibitory receptors on tumor-infiltrating immune cells and result in immune cell inhibition. These inhibitory receptors (i.e., immune checkpoints) act as a regulatory system that physiologically protects the body from autoimmunity and plays a pivotal role in tumor development. Checkpoint blockade immunotherapy utilizes antibodies to block inhibitory signaling to prevent T cell inhibition. Several different checkpoint inhibitors have been used to treat NSCLC and MPM. The most noteworthy immune checkpoints are cytotoxic T lymphocyte-associated protein 4 (CTLA-4) and programmed cell death protein 1 (PD-1)/programmed death ligand 1 (PD-L1) pathways.
CTLA-4 inhibition
CTLA-4 is a glycoprotein that is expressed by activated T cells and regulatory T cells (Tregs), and is a strong negative regulator of T cells [16]. CTLA-4 competes with co-stimulatory receptor CD28 for B7 ligands (CD80 and CD86) that are expressed on antigen-presenting cells (APCs). The binding of CTLA-4/CD80 results in a direct inhibitory signal that decreases T cell effector function [17].
Ipilimumab (IgG1) is a fully human antibody that targets CTLA-4 and has demonstrated an impressive anti-melanoma immune response. This has led to a significant improvement in OS for patients with unresectable stage III/IV melanoma [18]. These results have led to several clinical trials that assess anti-CTLA-4 checkpoint inhibitors in a variety of solid malignancies including NSCLC and MPM.
A phase II trial compared ipilimumab plus chemotherapy with chemotherapy alone in previously untreated patients with extensive-stage SCLC. Ipilimumab was administered either concurrently with carboplatin and paclitaxel or in a phased approach. The primary endpoint was immune-related progression-free survival (PFS). Improvement in PFS was only seen with a phased approach (5.7 vs. 4.6 months, HR = 0.72, P = 0.05). The results from this trial suggest that patients with squamous NSCLC may derive even greater benefit from ipilimumab treatment [19]. There are two open clinical trials no longer recruiting patients (NCT01285609 and NCT02279732) that are assessing ipilimumab in patients with squamous histology. Additionally, there is an open clinical trial that is assessing ipilimumab in combination with nivolumab, a PD-1 pathway checkpoint inhibitor, for the treatment of patients with chemotherapy-naïve or recurrent stage IV NSCLC (Table 1).
CTLA-4 checkpoint inhibitors have also been used in the treatment of MPM. A phase II clinical trial evaluated the anti-CTLA-4 antibody tremelimumab in 29 patients with unresectable MPM. Disease control was achieved in 52% of patients with a median duration of 10.9 months (95% CI, 8.2–13.6 months) [20]. There is currently one active phase II clinical trial that is no longer recruiting patients (NCT01843374) that is comparing tremelimumab as a solitary therapy and tremelimumab as a placebo for patients with unresectable MPM. There is also an open clinical trial currently recruiting patients that is evaluating combination therapy of tremelimumab with durvalumab, an anti-PD-L1 checkpoint inhibitor (Table 2).
PD-1 inhibition
The surface receptor PD-1 is a member of the B7-CD28 superfamily—similar to CTLA-4—and is a key immune checkpoint receptor. PD-1 is expressed by activated T cells, B cells, and natural killer (NK) cells. It functions in peripheral tissue where it binds to the immunosuppressive PD-L1 and PD-L2 ligands that are expressed on tumor cells and APCs [21]. The PD-1/PD-L1 interaction leads to decreased T cell cytotoxicity, cytokine release, proliferation, and, ultimately, T cell exhaustion [22]. PD-1-specific antibodies (i.e., nivolumab and pembrolizumab) are being evaluated in ongoing clinical trials.
Nivolumab is a human IgG4 monoclonal antibody that targets PD-1. It was initially studied in a phase I clinical trial that assessed the drug’s safety, antitumor activity, and pharmacokinetics [21]. In 122 patients with advanced NSCLC who had previously received systemic chemotherapy or immunotherapy, patients received 1, 3, or 10 mg/kg doses every 2 weeks. The optimal dose was 3 mg/kg and it yielded an objective response rate (ORR) of 32%. Subsequently, multiple trials have tested nivolumab as either monotherapy or in combination with other therapies. The CheckMate 017 study assessed nivolumab as a second-line therapy for recurrent stage IIIB/IV squamous NSCLC. Nivolumab had a statistically significant improvement in OS compared with docetaxel (9.2 vs. 6.0 months) [23]; these results ultimately led to FDA approval as a second-line therapy for metastatic NSCLC with progression after standard therapy. Borghaei et al. assessed nivolumab versus docetaxel as second-line therapy for non-squamous NSCLC and nivolumab demonstrated improved median OS (12.2 vs. 9.4 months) [24].
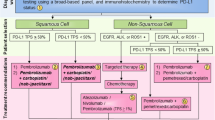
Pembrolizumab is a human IgG4 antibody that targets the PD-1 immune checkpoint. In the KEYNOTE-001 trial, patients with NSCLC who had >50% PD-L1 expression exhibited a higher response rate, greater OS, and greater PFS than patients with <50% membrane PD-L1 expression; median OS for all patients was 12 months [25]. During the KEYNOTE-010 trial, PD-L1 expression and its effect on efficacy were prospectively assessed. The study involved 1034 patients with NSCLC who were randomized to receive pembrolizumab, at 2 and 10 mg/kg doses, or docetaxel. Median OS was greater for patients who had received pembrolizumab at either 10 mg/kg (12.7 months) or 2 mg/kg (10.4 months) compared with docetaxel (8.5 months) [26].
Finally, the KEYNOTE-028 trial studied response to pembrolizumab in PD-L1-positive solid tumors. There were 25 patients with MPM who had received 10 mg/kg every 2 weeks for 2 years or until observable disease progression and severe toxicity. The overall response rate was 24% (n = 6) and 13 patients (52%) had stable disease, which resulted in a disease control rate of 76% [27].
Anti-PD-L1 immunotherapies
PD-L1 is upregulated in a variety of malignancies—including NSCLC and MPM—and its expression correlates with poor prognosis [28, 29]. PD-L1 is expressed in 25–36% of NSCLC [30]. Mansfield et al. showed that PD-L1 expression occurred in approximately 40% of 106 mesothelioma specimens and that higher expression was correlated with worse prognoses (5.0 vs. 14.5 months) [31]. Additionally, Awad et al. showed that patients with PD-L1-positive tumors had lower median survival (4.79 vs. 16.3 months, P = 0.012) [29]. Several anti-PD-L1 therapies are currently being investigated in clinical trials as a result of these findings, which are in addition to the critical role that PD-L1 plays in the effectiveness of anti-PD-1 therapy that has been shown in the KEYNOTE-010 and KEYNOTE-028 trials. These IgG1 monoclonal antibodies inhibit binding of PD-L1 to PD-1.
The POPLAR trial was a phase II trial that compared atezolizumab, a PD-L1 checkpoint inhibitor, with docetaxel. The OS was 12.6 and 9.7 months for atezolizumab and docetaxel, respectively. Of note, patients with low PD-L1 expression did not benefit as much as patients with higher PD-L1 expression [32]. The ongoing JAVELIN trial is assessing avelumab, a human anti-PD-L1 IgG1, in patients with both metastatic and locally advanced solid tumors. In this cohort, there are 53 patients with MPM who have been assessed and results indicate that the disease control rate was 56.6% and median PFS was 17.1 weeks (95% CI, 6.1–30.1 weeks) [33].
There are several open and recruiting clinical trials that are utilizing checkpoint inhibition as monotherapy, combined with chemotherapy, or in combination with other methods of immunotherapy for the treatment of NSCLC and MPM (Tables 1 and 2). Despite the rapid growth in this method of immunotherapy, there are still several limitations. Stimulating the immune system leads to a unique assortment of side effects and toxicities called immune-related adverse events (irAE). Common irAEs associated with checkpoint inhibitors are fatigue, rash, colitis, and hepatitis. Severe side effects include pneumonitis and endocrinopathies such as hypophysitis [34]. Of note, biomarkers that can predict safety or predisposition for irAEs are lacking. Similarly lacking are methods or biomarkers that can predict if a patient population will benefit from checkpoint inhibition. Finally, blocking checkpoint inhibition pathways has been shown to lead to an upregulation of different inhibitory checkpoints, such as T cell immunoglobulin and mucin domain 3 (TIM-3) and lymphocyte-activation gene 3 (LAG-3) [35], which is an obstacle that will receive increasing attention going forward.
Immunotoxin
Immunotoxin therapy is an antibody-based immunotherapy that targets specific antigens and utilizes antibodies to chaperone potent toxins to the cytosol of a cancer cell via endocytosis and results in cell death. This therapy has shown promising results in hematologic malignancies, such as hairy cell leukemia, where the majority of patients had achieved complete remission after therapy [36]. Although it has been applied in MPM, its application in solid malignancies has been limited.
Mesothelin (MSLN) is a cell surface protein that is overexpressed in a variety of solid tumors including mesothelioma, ovarian, and pancreatic cancers. SS1P is an immunotoxin consisting of an anti-MSLN antibody fragment that is linked to a cytotoxic fragment of pseudomonas exotoxin A. Hassan et al. initially demonstrated that SS1P can be administered safely as a monotherapy with moderate antitumor efficacy [37]. But, when it was combined with pentostatin and cyclophosphamide there were impressive observable antitumor responses—10 of 13 patients with MPM exhibited at least a partial response [38]. A recently completed phase I clinical trial (NCT01445392) that is awaiting data analysis tested SS1P combined with cisplatin and pemetrexed. LMB-100, a MSLN-targeted immunotoxin, is being studied in a phase I clinical trial (NCT02798536) that is currently recruiting patients.
Although there has yet to be a clinical trial that assesses an immunotoxin therapy exclusively for NSCLC, MSLN has been shown to be highly expressed on NSCLC tumors [39]; this may be a potential application for immunotoxin therapy in the future. It is important to note that a limitation of immunotoxin therapy is the potential for patients to develop neutralizing antibodies against the toxin [40]. Additionally, there are few target antigens and identification of additional targets will be important going forward.
Anticancer vaccines
Cancer vaccination is a method of immunotherapy that involves activating the innate or adaptive immune response using biologically active whole cell or specific peptide antigens. The purpose is to induce specific antitumor immunity against tumor-associated antigens (TAAs).
Whole cell vaccines
Tergenpumatucel-L is a whole cell vaccine that was developed from three allogenic lung tumor cell lines that have been genetically modified to express carbohydrate α-galactosyltransferase, a potent immunogenic enzyme. There was a phase II clinical trial where 28 patients with advanced NSCLC received tergenpumatucel-L and the treatment was well tolerated with no serious adverse events [41]. A subsequent phase IIB/III clinical trial (NCT01774578) that compared tergenpumatucel-L with docetaxel in patients with progressive or relapsed NSCLC has stopped collecting data as of February 2017. A phase I/II trial (NCT02460367) studying combination tergenpumatucel-L with a checkpoint inhibitor that blocks the indoleamine 2,3-dioxygenase (IDO) pathway is open and currently recruiting patients.
Antigen-associated vaccines
The melanin associated antigen-A3 (MAGE-A3) is an antigen with limited expression on non-malignant cells. It is widely expressed in various malignancies including melanoma, sarcoma, esophageal cancer, and NSCLC. MAGE-A3 is expressed in 35% of patients with NSCLC [42]. A phase II trial that evaluated MAGE-3 as adjuvant therapy in resected NSCLC failed to show a statistically significant difference in disease-free survival (DFS) and OS [42]. Additionally, the follow-up “MAGE-A3 as Adjuvant Non-Small-Cell Lung Cancer Immunotherapy” (MAGRIT) phase III trial compared a vaccine with placebo in MAGE-A3-positive tumors, but was stopped in early 2014 because it failed to reach their primary endpoint of extending DFS [43]. Nonetheless, MAGE-A3 continues to be a target antigen of interest as a vaccine (Table 1).
Mucin 1 (MUC1) is a membrane-bound glycoprotein that becomes overexpressed in a variety of malignancies including >60% of NSCLC tumors [44]. Tecemotide (liposomal Braun’s lipoprotein [BLP]-25) is an antigen-associated vaccine that targets the MUC1 glycoprotein. In a phase II trial, patients who received tecemotide showed a statistically significant increase in median 3-year OS and patients with stage IIIB locoregional disease exhibited the most significant benefit [45]. These findings led to the stimulating targeted antigenic response to NSCLC (START) trial. This phase III trial evaluated tecemotide versus placebo as maintenance therapy in stage III patients with unresectable disease who had completed chemoradiation therapy; there was no significant difference in OS between both groups (median OS, 25.6 vs. 22.3 months, HR = 0.88, P = 0.123) [46].
MUC1 has also been targeted by TG4010, which is generated from a modified vaccinia Ankara virus that contains the sequence for the MUC1 and IL-2 proteins. There was a phase IIB trial that demonstrated an increase in 6-month PFS with TG4010 plus cisplatin/gemcitabine when compared with chemotherapy alone [47]. These results led to a phase IIB/III trial that compared the efficacy and safety of first-line chemotherapy compared with TG4010. The results have demonstrated that TG4010 administered with chemotherapy improves PFS relative to placebo plus chemotherapy [47]. TG4010, in combination with nivolumab, is currently being assessed in a phase II trial of NSCLC patients with progressive disease after systemic therapy (Table 1).
EGFR is a well-known oncogene that promotes proliferation of tumors cells. A lung cancer vaccine for advanced NSCLC that was developed in Cuba (CIMAvax-EGF) is an antigen-associated vaccine where human EGF is fused to a carrier protein. This vaccine aims to induce anti-EGF antibodies, thus helping the host fight EGF-positive tumors [48]. In a phase III trial, 405 patients were randomized to receive CIMAvax-EGF or the control for 4–6 weeks following first-line chemotherapy. Median survival time was 12.43 months for patients who were treated with the vaccine and 9.43 months in the control group (HR = 0.77, P = 0.036). This difference was further amplified in patients with high EGF concentration at baseline (14.66 months) [48]. A follow-up international phase III randomized trial assessing an EGF cancer vaccine in patients with unresectable EGFR-positive NSCLC is currently open and recruiting patients (Table 1).
With regard to antigen presentation, antigen-exposed autologous dendritic cells (DCs) are perhaps the most potent APCs [49]. They are capable of capturing and processing tumor antigens, expressing co-stimulatory molecules, and they secrete cytokines to initiate immune responses. Due to this, DCs have been increasingly used in tumor cell vaccinations for both NSCLC and MPM. In a recent trial of MPM patients (n = 10), DC vaccination combined with cyclophosphamide resulted in 7 patients who survived ≥24 months and 2 patients who survived 50 and 66 months after treatment [50]. There are several open and recruiting clinical trials that are assessing autologous DC vaccination (DC-VAC) for the treatment of NSCLC (Table 1) and MPM (Table 2). There are also open and recruiting clinical trials that are evaluating targeted vaccinations such as monotherapy, combination chemotherapy, and other types of immunotherapy.
In summary, both whole cell and targeted vaccine therapies have shown mixed results with early phase III trials showing no significant survival benefits; however, recent results with CIMAvax-EGF, TG4010, and DC seem promising. The two limitations that must be overcome if cancer vaccination is to be successful are the lack of strong expression of target antigens on cancer cells and the reliance of host immunity to mount an immune response.
Adoptive cell therapy
Adoptive cell therapy (ACT) entails the collection of immune cells from peripheral blood or the tumor itself, isolation, modification, and ex vivo expansion of targeted immune cells, and then reinfusion of those immune cells to the patient [51]. ACT offers the advantage of targeting effector cells to a specific TAA that eventually leads to direct cytotoxicity.
The evolution of ACT dates back to the 1960s but has seen a rapid growth in development and application since the turn of the century. The first application of adoptive T cell therapy involved in vitro activation, expansion, and reinfusion of antigen-specific tumor-infiltrating lymphocytes (TILs) [52]. Since then, there have been several different strategies that aim to harness the antitumor efficacy of T cells including genetically modifying the T cell receptor (TCR) and chimeric antigen receptor (CAR)-modified T cells. Additionally, ACT has been applied to NK and cytokine-induced killer (CIK) cells.
Natural killer cell therapy
Human NK cells are peripheral blood lymphocytes defined by the expression of CD56 and the absence of TCR CD3. NK cells can target “non-self” antigens, virally infected cells, and malignant cells. This interaction results in the release of cytokines and, when exposed to cytokines, NK cells proliferate, release additional cytokines, and become increasingly cytotoxic via the release of perforins and granzymes [53].
In a phase I trial, patients with advanced NSCLC who were currently receiving chemotherapy were given NK cells. Fifteen patients received two to four doses of allogeneic-activated NK cells; there were no local or systemic side effects. Furthermore, 56% of patients had a 1-year survival rate whereas 19% had a 2-year survival rate [54]. There are currently several open and recruiting clinical trials that are employing autologous administration of NK cells (Table 1).
Cytokine-induced killer cells
CIK cells are rapidly proliferating effector CD8+ T cells with diverse TCR specificities. CIKs exhibit non-major histocompatibility complex (MHC)-restricted cytolytic activity against tumor cells that can result in enhanced cytotoxicity. CIKs can be expanded from peripheral blood lymphocytes (PBLs) and proliferate rapidly when stimulated with interleukin-2 (IL-2), interferon-γ (IFN-γ), and anti-CD3 monoclonal antibody [29].
Li et al. investigated the efficacy of CIK cell therapy following adjuvant chemotherapy. The 3-year OS rate and median OS were significantly higher in the group treated with combined chemotherapy plus CIK therapy versus chemotherapy alone (82 vs. 66%; P = 0.049, and 73 vs. 53 months; P = 0.006, respectively) [55]. Furthermore, combination therapy with CIK cells and DC-based cancer vaccines may have a synergistic effect and there are several open clinical trials assessing this combination in patients with NSCLC (Table 1).
Tumor-infiltrating lymphocyte therapy
The aforementioned TIL therapy involves isolation of T cells from fresh cancer specimens, expansion ex vivo using high doses of IL-2, and then infusion back into autologous hosts. Although there was success using this modality in malignant melanoma, the use of TILs still poses several challenges. Specifically, tumor-reactive lymphocytes are relatively scarce in cancer patients and isolation and expansion of T cells that retain specificity and functionality can be difficult [56]. Additionally, without lymphodepletion via chemotherapy, clinical response to TIL therapy was often short-lived [51]. Despite this, there is an open phase II trial (NCT02133196) currently recruiting patients that is using autologous young TILs derived from patients with NSCLC following a non-myeloablative, lymphocyte-depleting chemotherapeutic regimen (cyclophosphamide and fludarabine).
Engineered T cell therapy
Given the difficulties encountered with TIL therapy, there have been developments in methods for engineered T cell therapy. This therapy entails redirecting T cells toward specific TAAs. To achieve this goal, two strategies have been employed—genetic insertion of TCRs into T cells and genetic insertion of a CAR into T cells.
T cell receptor therapy
This therapy consists of genetically engineering large T cell populations to target specific TAAs. The specificity of a T cell toward a specific antigen is mediated through the alpha- and beta-chain heterodimers of the TCR complex [56]. A TCR alpha/beta-chain gene can be modified to target a specific antigen and then retrovirally transduced into T cells from healthy donors [56]. The restriction is that TCR therapy is MHC-dependent. Therefore, in order for T cell activation to occur, the TCR must bind to a specific MHC-antigen complex. Because of this, the therapy is limited to MHC-matched patients [52]. Tumors can also evade the effect of TCRs by downregulating MHC class I expression, which results in less T cell-dependent tumor cell lysis [56]. There are several open and recruiting clinical trials that involve TCR immunotherapy targeting cancer-testis antigen (NY-ESO-1), MAGE-A3, and Wilms tumor 1 (WT-1) (Tables 1 and 2).
Chimeric antigen receptor T cell therapy
Limitations of TCR therapy have led to the development of an alternative to TCR gene-redirected T cells. CAR-modified T cells are not restricted by MHC and can theoretically target any antigen or tumor. A CAR consists of an extracellular antigen-binding domain that is hinged to one or more intracellular signaling domains [57]. Once constructed, the CAR is transduced, either by use of retroviral or lentiviral vectors, into autologous T cells and transfused back to the patient for therapy. The use of CARs that target CD19, a B cell activation receptor, has had success treating B cell malignancies such as acute lymphoblastic leukemia and chronic lymphocytic leukemia [58]. The results of CAR T cells in hematologic malignancies have led to rapid growth in this intriguing field of immunotherapy.
Our laboratory work is focused on investigating CAR T cell therapy for MSLN-expressing tumors. As previously mentioned, MSLN is expressed in a variety of malignancies including NSCLC and MPM. We have shown that MSLN is uniformly and strongly expressed on MPM cells and has limited expression on normal tissue [59].
Our preclinical studies have shown that regional delivery of MSLN-targeted CAR T cells were able to eradicate tumors at a 30-fold lower dose than systemically delivered CAR T cells. Additionally, these intrapleurally administered CAR T cells outperformed the systemically delivered T cells in terms of T cell activation, proliferation, persistence, tumor eradication, and survival. These results have led to the development of an open and recruiting phase I study (NCT02414269) where patients with MPM or other secondary pleural malignancies receive a single dose of intrapleurally delivered MSLN-targeted CAR T cells, with or without prior cyclophosphamide therapy. There are several additional clinical trials evaluating CAR T cells that target MSLN for the treatment of MPM (Table 2). Finally, there is an open and recruiting trial assessing CAR T cell therapy in patients with mucin-positive solid tumors including NSCLC (Table 1).
Conclusion
Immunotherapy employs several novel therapies and is a promising and rapidly developing approach for treating solid tumor malignancies. This review highlighted some of the key successes of immunotherapy for the treatment of NSCLC and MPM. We have also discussed some of the limitations of immunotherapy—including identification of biomarkers to identify potential target populations who will benefit most, identification of target antigens, and identification of the mechanisms of resistance and inhibition within the complex tumor immune microenvironment. There are many early phase clinical trials that have assessed immunotherapy as first-line, second-line, and maintenance therapy, and have compared those drugs as monotherapies or in combination with chemotherapy or other types of immunotherapy. The results and data generated from these diverse trials, combined with the failures and successes of the complete body of research, will lay the foundation for the future of this exciting therapeutic modality.
References
Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology, and prevention. Clin Chest Med. 2011;32:605–44.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
Aerts JG, Lievense LA, Hoogsteden HC, Hegmans JP. Immunotherapy prospects in the treatment of lung cancer and mesothelioma. Transl Lung Cancer Res. 2014;3:34–45.
Park EK, Takahashi K, Hoshuyama T, et al. Global magnitude of reported and unreported mesothelioma. Environ Health Perspect. 2011;119:514–8.
Robinson BM. Malignant pleural mesothelioma: an epidemiological perspective. Ann Cardiothorac Surg. 2012;1:491–6.
Milano MT, Zhang H. Malignant pleural mesothelioma: a population-based study of survival. J Thorac Oncol. 2010;5:1841–8.
Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346:92–8.
Jackman DM, Miller VA, Cioffredi LA, et al. Impact of epidermal growth factor receptor and KRAS mutations on clinical outcomes in previously untreated non-small cell lung cancer patients: results of an online tumor registry of clinical trials. Clin Cancer Res. 2009;15:5267–73.
Vogelzang NJ, Rusthoven JJ, Symanowski J, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol. 2003;21:2636–44.
Treasure T, Lang-Lazdunski L, Waller D, et al. Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol. 2011;12:763–72.
Zahid I, Sharif S, Routledge T, Scarci M. Is pleurectomy and decortication superior to palliative care in the treatment of malignant pleural mesothelioma? Interact Cardiovasc Thorac Surg. 2011;12:812–7.
Kotova S, Wong RM, Cameron RB. New and emerging therapeutic options for malignant pleural mesothelioma: review of early clinical trials. Cancer Manag Res. 2015;7:51–63.
Rimner A, Zauderer MG, Gomez DR, et al. Phase II study of hemithoracic intensity-modulated pleural radiation therapy (IMPRINT) as part of lung-sparing multimodality therapy in patients with malignant pleural mesothelioma. J Clin Oncol. 2016;34:2761–8.
Krug LM, Pass HI, Rusch VW, et al. Multicenter phase II trial of neoadjuvant pemetrexed plus cisplatin followed by extrapleural pneumonectomy and radiation for malignant pleural mesothelioma. J Clin Oncol. 2009;27(18):3007–13.
Dunn GP, Old LJ, Schreiber RD. The three Es of cancer immunoediting. Annu Rev Immunol. 2004;22:329–60.
Woo EY, Yeh H, Chu CS, et al. Cutting edge: Regulatory T cells from lung cancer patients directly inhibit autologous T cell proliferation. J Immunol. 2002;168:4272–6.
Grosso JF, Jure-Kunkel MN. CTLA-4 blockade in tumor models: an overview of preclinical and translational research. Cancer Immun. 2013;13:5.
Hodi FS, O'Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23.
Lynch TJ, Bondarenko I, Luft A, et al. Ipilimumab in combination with paclitaxel and carboplatin as first-line treatment in stage IIIB/IV non-small-cell lung cancer: results from a randomized, double-blind, multicenter phase II study. J Clin Oncol. 2012;30:2046–54.
Calabro L, Morra A, Fonsatti E, et al. Efficacy and safety of an intensified schedule of tremelimumab for chemotherapy-resistant malignant mesothelioma: an open-label, single-arm, phase 2 study. Lancet Respir Med. 2015;3:301–9.
Topalian S, Hodi FS, Brahmer JR, et al. Safety, Activity, and Immune Correlates of Anti–PD-1 Antibody in Cancer. N Engl J Med. 2012;366:2443–54.
Zhang Y, Huang S, Gong D, Qin Y, Shen Q. Programmed death-1 upregulation is correlated with dysfunction of tumor-infiltrating CD8+ T lymphocytes in human non-small cell lung cancer. Cell Mol Immunol. 2010;7:389–95.
Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373:123–35.
Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373:1627–39.
Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372:2018–28.
Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50.
Alley EN, Molife LR, Santoro A, et al. Clinical safety and efficacy of pembrolizumab (MK-3475) in patients with malignant pleural mesothelioma: preliminary results from KEYNOTE-028. Am Assoc Cancer Resear. 2015. abstr number CT103.
Zhang Y, Wang L, Li Y, et al. Protein expression of programmed death 1 ligand 1 and ligand 2 independently predict poor prognosis in surgically resected lung adenocarcinoma. Onco Targets Ther. 2014;7:567–73.
Awad MM, Jones RE, Liu H, et al. Cytotoxic T Cells in PD-L1-positive malignant pleural mesotheliomas are counterbalanced by Distinct Immunosuppressive Factors. Cancer Immunol Res. 2016;4:1038–48.
Velcheti V, Schalper KA, Carvajal DE, et al. Programmed death ligand-1 expression in non-small cell lung cancer. Lab Investig. 2014;94:107–16.
Mansfield AS, Roden AC, Peikert T, et al. B7-H1 expression in malignant pleural mesothelioma is associated with sarcomatoid histology and poor prognosis. J Thorac Oncol. 2014;9:1036–40.
Fehrenbacher L, Spira A, Ballinger M, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387:1837–46.
Hassan R, Thomas A, Patel MR, et al. Avelumab (MSB0010718C; anti-PD-L1) in patients with advanced unresectable mesothelioma from the JAVELIN solid tumor phase Ib trial: Safety, clinical activity, and PD-L1 expression. J Clin Oncol. 2016;34 abstr8503
Kumar V, Chaudhary N, Garg M, Floudas CS, Soni P, Chandra AB. Current diagnosis and management of immune related adverse events (irAEs) induced by immune checkpoint inhibitor therapy. Front Pharmacol. 2017;8:49.
Koyama S, Akbay EA, Li YY, et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat Commun. 2016;7:10501.
Kreitman RJ, Wilson WH, Bergeron K, et al. Efficacy of the anti-CD22 recombinant immunotoxin BL22 in chemotherapy-resistant hairy-cell leukemia. N Engl J Med. 2001;345:241–7.
Hassan R, Bullock S, Premkumar A, et al. Phase I study of SS1P, a recombinant anti-mesothelin immunotoxin given as a bolus I.V. infusion to patients with mesothelin-expressing mesothelioma, ovarian, and pancreatic cancers. Clin Cancer Res. 2007;13:5144–9.
Hassan R, Sharon E, Thomas A, et al. Phase 1 study of the antimesothelin immunotoxin SS1P in combination with pemetrexed and cisplatin for front-line therapy of pleural mesothelioma and correlation of tumor response with serum mesothelin, megakaryocyte potentiating factor, and cancer antigen 125. Cancer. 2014;120:3311–9.
Kachala SS, Bograd AJ, Villena-Vargas J, et al. Mesothelin overexpression is a marker of tumor aggressiveness and is associated with reduced recurrence-free and overall survival in early-stage lung adenocarcinoma. Clin Cancer Res. 2014;20:1020–8.
Ho M, Bera TK, Willingham MC, et al. Mesothelin expression in human lung cancer. Clin Cancer Res. 2007;13:1571–5.
Morgensztern D, Campo MJ, Dahlberg SE, et al. Molecularly targeted therapies in non-small-cell lung cancer annual update 2014. J Thorac Oncol. 2015;10:S1–S63.
Vansteenkiste J, Zielinski M, Linder A, et al. Adjuvant MAGE-A3 immunotherapy in resected non-small-cell lung cancer: phase II randomized study results. J Clin Oncol. 2013;31:2396–403.
Tyagi P, Mirakhur B. MAGRIT: the largest-ever phase III lung cancer trial aims to establish a novel tumor-specific approach to therapy. Clin Lung Cancer. 2009;10:371–4.
Sharma S, Srivastava MK, Harris-White M, Lee JM, Dubinett S. MUC1 peptide vaccine mediated antitumor activity in non-small cell lung cancer. Expert Opin Biol Ther. 2011;11:987–90.
Butts C, Maksymiuk A, Goss G, et al. Updated survival analysis in patients with stage IIIB or IV non-small-cell lung cancer receiving BLP25 liposome vaccine (L-BLP25): phase IIB randomized, multicenter, open-label trial. J Cancer Res Clin Oncol. 2011;137:1337–42.
Butts C, Socinski MA, Mitchell PL, et al. Tecemotide (L-BLP25) versus placebo after chemoradiotherapy for stage III non-small-cell lung cancer (START): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2014;15:59–68.
Quoix E, Lena H, Losonczy G, et al. TG4010 immunotherapy and first-line chemotherapy for advanced non-small-cell lung cancer (TIME): results from the phase 2b part of a randomised, double-blind, placebo-controlled, phase 2b/3 trial. Lancet Oncol. 2016;17:212–23.
Rodriguez PC, Popa X, Martinez O, et al. A Phase III clinical trial of the epidermal growth factor vaccine CIMAvax-EGF as switch maintenance therapy in advanced non-small cell lung cancer patients. Clin Cancer Res. 2016;22:3782–90.
Thomas A, Hassan R. Immunotherapies for non-small-cell lung cancer and mesothelioma. Lancet Oncol. 2012;13:e301–10.
Cornelissen R, Hegmans JP, Maat AP, et al. Extended tumor control after dendritic cell vaccination with low-dose cyclophosphamide as adjuvant treatment in patients with malignant pleural mesothelioma. Am J Respir Crit Care Med. 2016;193:1023–31.
Rosenberg SA, Restifo NP. Adoptive cell transfer as personalized immunotherapy for human cancer. Science. 2015;348:62–8.
Cartellieri M, Bachmann M, Feldmann A, et al. Chimeric antigen receptor-engineered T cells for immunotherapy of cancer. J Biomed Biotechnol. 2010;2010:956304.
Geller MA, Miller JS. Use of allogeneic NK cells for cancer immunotherapy. Immunotherapy. 2011;3:1445–59.
Iliopoulou EG, Kountourakis P, Karamouzis MV, et al. A phase I trial of adoptive transfer of allogeneic natural killer cells in patients with advanced non-small cell lung cancer. Cancer Immunol Immunother. 2010;59:1781–9.
Li R, Wang C, Liu L, et al. Autologous cytokine-induced killer cell immunotherapy in lung cancer: a phase II clinical study. Cancer Immunol Immunother. 2012;61:2125–33.
Sadelain M, Riviere I, Brentjens R. Targeting tumours with genetically enhanced T lymphocytes. Nat Rev Cancer. 2003;3:35–45.
Sadelain M, Brentjens R, Riviere I. The basic principles of chimeric antigen receptor design. Cancer Discov. 2013;3:388–98.
Grupp SA, Kalos M, Barrett D, et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med. 2013;368:1509–18.
Servais EL, Colovos C, Rodriguez L, et al. Mesothelin overexpression promotes mesothelioma cell invasion and MMP-9 secretion in an orthotopic mouse model and in epithelioid pleural mesothelioma patients. Clin Cancer Res. 2012;18:2478–89.
Acknowledgements
We thank Alex Torres of the MSK Thoracic Surgery Service for his editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approvals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This is review article and not a study. Hence, there is no study participation involved and no requirement of consent.
Financial statement
The author’s research is supported by grants from the National Institutes of Health (P30 CA008748), the U.S. Department of Defense (LC160212), the Mesothelioma Applied Research Foundation, the Baker Street Foundation, the Joanne and John DallePezze Foundation, the Derfner Foundation, and the Mr. William H. Goodwin and Alice Goodwin, the Commonwealth Foundation for Cancer Research, and the Experimental Therapeutics Center.
Rights and permissions
About this article
Cite this article
Dozier, J., Chintala, N. & Adusumilli, P. Immunotherapy for thoracic malignancies. Indian J Thorac Cardiovasc Surg 34 (Suppl 1), 54–64 (2018). https://doi.org/10.1007/s12055-017-0566-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-017-0566-2