Abstract
Purpose
Preoperative prediction of transsphenoidal surgical (TSS) response is important for determining individual treatment strategies for acromegaly. There is currently no accurate predictive model for TSS response for acromegaly. The current study sought to develop and validate machine learning (ML)-based models for preoperative prediction of TSS response for acromegaly.
Methods
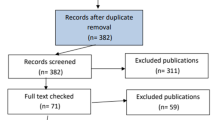
Six hundred sixty-eight patients with acromegaly were enrolled and divided into training (n = 534) and text datasets (n = 134) in this retrospective, data mining and ML study. The forward search algorithm was used to select features, and six ML algorithms were applied to construct TSS response prediction models. The performance of these ML models was validated using receiver operating characteristics analysis. Model calibration, discrimination ability, and clinical usefulness were also assessed.
Results
Three hundred forty-nine (52.2%) patients achieved postoperative remission criteria and exhibited good TSS response. A univariate analysis was conducted and eight features, including age, hypertension, ophthalmic disorders, GH, IGF-1, nadir GH, maximal tumor diameter, and Knosp grade, were significantly associated with the TSS response in patients with acromegaly. After feature selection, the gradient boosting decision tree (GBDT), which was constructed with the eight significant features showed the best favorable discriminatory ability both the training (AUC = 0.8555) and validation (AUC = 0.8178) cohorts. The GBDT model showed good discrimination ability and calibration, with the highest levels of accuracy and specificity, and provided better estimates of TTS responses of patients with acromegaly compared with using only the Knosp grade. Decision curve analysis confirmed that the model was clinically useful.
Conclusions
ML-based models could aid neurosurgeons in the preoperative prediction of TTS response for patients with acromegaly, and could contribute to determining individual treatment strategies.





Similar content being viewed by others
References
S. Melmed, M.D. Bronstein, P. Chanson, A. Klibanski, F.F. Casanueva, J.A.H. Wass et al. A Consensus Statement on acromegaly therapeutic outcomes. Nat. Rev. Endocrinol. 14(9), 552–61 (2018)
D. Esposito, O. Ragnarsson, D. Granfeldt, T. Marlow, G. Johannsson, D.S. Olsson, Decreasing mortality and changes in treatment patterns in patients with acromegaly from a nationwide study. Eur. J. Endocrinol. 178(5), 459–69. (2018)
C. Leopoldo, F. Leopoldo, A. Santos, J.C.E. Veiga, J.V.J. Lima, N.M. Scalissi et al. Long term follow-up of growth hormone-secreting pituitary adenomas submitted to endoscopic endonasal surgery. Arq. Neuropsiquiatr. 75(5), 301–6 (2017)
A. Buliman, L.G. Tataranu, V. Ciubotaru, T.L. Cazac, C. Dumitrache, The multimodal management of GH-secreting pituitary adenomas: predictive factors, strategies and outcomes. J. Med. Life 9(2), 187–92 (2016)
S. Melmed, A. Colao, A. Barkan, M. Molitch, A.B. Grossman, D. Kleinberg et al. Guidelines for acromegaly management: an update. J. Clin. Endocrinol. Metab. 94(5), 1509–17 (2009)
L. Katznelson, E.R. Laws Jr., S. Melmed, M.E. Molitch, M.H. Murad, A. Utz et al. Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99(11), 3933–51 (2014)
B. Zhao, Y.K. Wei, G.L. Li, Y.N. Li, Y. Yao, J. Kang et al. Extended transsphenoidal approach for pituitary adenomas invading the anterior cranial base, cavernous sinus, and clivus: a single-center experience with 126 consecutive cases. J. Neurosurg. 112(1), 108–17 (2010)
M.E. Sughrue, E.F. Chang, R.A. Gabriel, M.K. Aghi, L.S. Blevins, Excess mortality for patients with residual disease following resection of pituitary adenomas. Pituitary 14(3), 276–83 (2011)
S.M. Carlsen, M. Lund-Johansen, T. Schreiner, S. Aanderud, O. Johannesen, J. Svartberg et al. Preoperative octreotide treatment in newly diagnosed acromegalic patients with macroadenomas increases cure short-term postoperative rates: a prospective, randomized trial. J. Clin. Endocrinol. Metab. 93(8), 2984–90 (2008)
V.S. Nunes, J.M. Correa, M.E. Puga, E.M. Silva, C.L. Boguszewski, Preoperative somatostatin analogues versus direct transsphenoidal surgery for newly-diagnosed acromegaly patients: a systematic review and meta-analysis using the GRADE system. Pituitary 18(4), 500–8 (2015)
S. Bacigaluppi, F. Gatto, P. Anania, N.L. Bragazzi, D.C. Rossi, G. Benvegnu et al. Impact of pre-treatment with somatostatin analogs on surgical management of acromegalic patients referred to a single center. Endocrine 51(3), 524–33. (2016)
S. Yano, N. Shinojima, J. Kawashima, T. Kondo, T. Hide, Intraoperative scoring system to predict postoperative remission in endoscopic endonasal transsphenoidal surgery for growth hormone-secreting pituitary adenomas. World Neurosurg. 105, 375–85. (2017)
W.J. Zhou, S.C. Ma, M. Zhao, C. Liu, X.D. Guan, Z.S. Bao et al. Risk factors and the prognosis of sexual dysfunction in male patients with pituitary adenomas: a multivariate analysis. Asian J. Androl. 20(1), 43–9 (2018)
M. Birkhahn, A.P. Mitra, R.J. Cote, Molecular markers for bladder cancer: the road to a multimarker approach. Expert Rev. Anticancer Ther. 7(12), 1717–27. (2007)
Y. Huang, Z. Liu, L. He, X. Chen, D. Pan, Z. Ma et al. Radiomics signature: a potential biomarker for the prediction of disease-free survival in early-stage (I or II) non-small cell lung cancer. Radiology 281(3), 947–57. (2016)
T.J. Cleophas, Machine learning in therapeutic research: the hard work of outlier detection in large data. Am. J. Ther. 23(3), e837–43 (2016)
M.H. Al-Mallah, R. Elshawi, A.M. Ahmed, W.T. Qureshi, C.A. Brawner, M.J. Blaha et al. Using Machine Learning to Define the Association between Cardiorespiratory Fitness and All-Cause Mortality (from the Henry Ford Exercise Testing Project). Am. J. Cardiol. 120(11), 2078–84. (2017)
A. Rajkomar, J. Dean, I. Kohane, Machine Learning in Medicine. N. Engl. J. Med 380(14), 1347–58. (2019)
C.J. Chiew, N. Liu, T.H. Wong, Y.E. Sim, H.R. Abdullah. Utilizing machine learning methods for preoperative prediction of postsurgical mortality and intensive care unit admission. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003297. [Epub ahead of print]
A.M. Bur, A. Holcomb, S. Goodwin, J. Woodroof, O. Karadaghy, Y. Shnayder et al. Machine learning to predict occult nodal metastasis in early oral squamous cell carcinoma. Oral. Oncol. 92, 20–5 (2019)
C. Rubbert, C. Mathys, C. Jockwitz, C.J. Hartmann, S.B. Eickhoff, F. Hoffstaedter et al. Machine-learning identifies parkinson’s disease patients based on resting-state between-network functional connectivity. Br. J. Radio. 92, 20180886 (2019)
H. Yu, H. Wu, W. Wang, S. Jolly, J.Y. Jin, C. Hu, et al., Machine learning to build and validate a model for radiation pneumonitis prediction in patients with non-small-cell lung cancer. Clin. Cancer Res 25, 4343–4350 (2019).
X. Guo, L. Gao, Y. Zhao, M. Wang, B. Jiang, Q. Wang et al. Characteristics of the upper respiratory tract in patients with acromegaly and correlations with obstructive sleep apnoea/hypopnea syndrome. Sleep. Med. 48, 27–34 (2018)
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33(4), 610–7 (1993). discussion 7–8
A. Di Ieva, F. Rotondo, L.V. Syro, M.D. Cusimano, K. Kovacs, Aggressive pituitary adenomas–diagnosis and emerging treatments. Nat. Rev. Endocrinol. 10(7), 423–35 (2014)
G.E.A.P.A. Batista, M.C. Monard, An analysis of four missing data treatment methods for supervised learning. Appl. Artif. Intell. 17(5–6), 519–33 (2003)
L.A. Shalabi, Z. Shaaban, B. Kasasbeh, Data mining: a preprocessing engine. J. Computer Sci. 2(9), 735–9 (2006)
Y. Liu, X. Liu, X. Hong, P. Liu, X. Bao, Y. Yao et al. Prediction of recurrence after transsphenoidal surgery for cushing’s disease: the use of machine learning algorithms. Neuroendocrinology 108(3), 201–10. (2019)
Y.V. Sun, Multigenic modeling of complex disease by random forests. Adv. Genet 72, 73–99 (2010)
B. Fu, P. Liu, J. Lin, L. Deng, K. Hu, H. Zheng. Predicting invasive disease-free survival for early-stage breast cancer patients using follow-up clinical data. IEEE Trans. Biomed. Eng. 66(7), 2053–64 (2019)
Y. Jung, Multiple predicting K-fold cross-validation for model selection. J. Nonparametr. Stat. 30(1), 197–215 (2018)
S.M. Erturk, Receiver operating characteristic analysis. AJR Am. J. Roentgenol. 197(4), W784 (2011).
A.A. Kramer, J.E. Zimmerman, Assessing the calibration of mortality benchmarks in critical care: The Hosmer-Lemeshow test revisited. Crit. Care Med 35(9), 2052–6 (2007)
A.J. Vickers, A.M. Cronin, E.B. Elkin, M. Gonen, Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inf. Decis. Mak. 8, 53 (2008)
E.H. Kim, M.C. Oh, J.H. Chang, J.H. Moon, C.R. Ku, W.S. Chang et al. Postoperative gamma knife radiosurgery for cavernous sinus-invading growth hormone-secreting pituitary adenomas. World Neurosurg. 110, e534–e45. (2018)
J.J. Jacob, J.S. Bevan, Should all patients with acromegaly receive somatostatin analogue therapy before surgery and, if so, for how long? Clin. Endocrinol. 81(6), 812–7 (2014)
L. Duan, H. Zhu, B. Xing, F. Gu, Prolonged preoperative treatment of acromegaly with somatostatin analogs may improve surgical outcome in patients with invasive pituitary macroadenoma (Knosp grades 1-3): a retrospective cohort study conducted at a single center. BMC Endocr. Disord. 17(1), 55 (2017)
C.B. Newman, S. Melmed, A. George, D. Torigian, M. Duhaney, P. Snyder et al. Octreotide as primary therapy for acromegaly. J. Clin. Endocrinol. Metab. 83(9), 3034–40. (1998)
M. Fleseriu, A.R. Hoffman, L. Katznelson, A. Neuroendocrine; Pituitary Scientific C, American association of clinical endocrinologists and american college of endocrinology disease state clinical review: management of acromegaly patients: what is the role of pre-operative medical therapy? Endocr. Pract. 21(6), 668–73 (2015)
N. Qiao. A systematic review on machine learning in sellar region diseases: quality and reporting items. Endocr. Connect. 8(7), 952–60 (2019)
V.E. Staartjes, C.M. Zattra, K. Akeret, N. Maldaner, G. Muscas, C.H. Bas van Niftrik et al. Neural network-based identification of patients at high risk for intraoperative cerebrospinal fluid leaks in endoscopic pituitary surgery. J. Neurosurg. 21, 1–7 (2019)
V.E. Staartjes, C. Serra, G. Muscas, N. Maldaner, K. Akeret, C.H.B. van Niftrik et al. Utility of deep neural networks in predicting gross-total resection after transsphenoidal surgery for pituitary adenoma: a pilot study. Neurosurg. Focus 45(5), E12 (2018)
T.C. Hollon, A. Parikh, B. Pandian, J. Tarpeh, D.A. Orringer, A.L. Barkan et al. A machine learning approach to predict early outcomes after pituitary adenoma surgery. Neurosurg. Focus 45(5), E8 (2018)
H. Babu, A. Ortega, M. Nuno, A. Dehghan, A. Schweitzer, H.V. Bonert et al. Long-term endocrine outcomes following endoscopic endonasal transsphenoidal surgery for acromegaly and associated prognostic factors. Neurosurgery 81(2), 357–66. (2017)
M.T. Ribeiro, S. Singh, C. Guestrin. “Why Should I Trust You?”: Explaining the Predictions of Any Classifier. (2016)
Rudin C. Please Stop Explaining Black Box Models for High Stakes Decisions. (2018)
I. Shimon, Z.R. Cohen, Z. Ram, M. Hadani, Transsphenoidal surgery for acromegaly: endocrinological follow-up of 98 patients. Neurosurgery 48(6), 1239–43 (2001)
I. Anik, B. Cabuk, A. Gokbel, A. Selek, B. Cetinarslan, Y. Anik et al. Endoscopic transsphenoidal approach for acromegaly with remission rates in 401 patients: 2010 consensus criteria. World Neurosurg. 108, 278–90. (2017)
X. Antunes, N. Ventura, G.B. Camilo, L.E. Wildemberg, A. Guasti, P.J.M. Pereira et al. Predictors of surgical outcome and early criteria of remission in acromegaly. Endocrine 60(3), 415–22. (2018)
Acknowledgements
We thank Benjamin Knight, MSc., from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this paper.
Funding
This work was supported by the Graduate Innovation Fund of Peking Union Medical College (2018-1002-01-10), Natural Science Foundation of Beijing Municipality (grant no. 7182137), Capital Characteristic Clinic Project (grant no. Z16100000516092), and Chinese Academy of Medical Sciences (grant no. 2017-I2M-3-014).
Author contributions
All authors provided contributions to study conception and design, acquisition of data, or analysis and interpretation of data, drafting of the article, or revising it critically for important intellectual content, and final approval of the version to be published. All authors analyzed and interpreted the data. YF and YL revised the paper for important intellectual content. RW, and MF take final responsibility for this article.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Padova University Hospital Ethics Committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
The study only involves the collection or study of existing data, documents, records, or diagnostic specimens, and these sources are publicly available or the information is recorded by the investigator in such a manner that subjects cannot be identified, directly or through identifiers linked to the subjects. And the need for patients’ informed consent was waved.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Fan, Y., Li, Y., Li, Y. et al. Development and assessment of machine learning algorithms for predicting remission after transsphenoidal surgery among patients with acromegaly. Endocrine 67, 412–422 (2020). https://doi.org/10.1007/s12020-019-02121-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-02121-6