Abstract
Purpose
Epidemiological data are pivotal for the estimation of disease burden in populations.
Aim
Of the study was to estimate the incidence and prevalence of acromegaly in Italy along with the impact of comorbidities and hospitalization rates as compared to the general population.
Methods
Retrospective epidemiological study (from 2000 to 2014) and case control-study. Data were extracted from the Health Search Database (HSD). HSD contains patient records from about 1000 general practitioners (GPs) throughout Italy, covering a population of more than 1 million patients. It includes information about patient demographics and medical data including clinical diagnoses and diagnostic tests.
Results
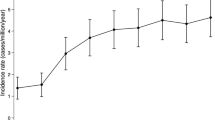
At the end of the study period, 74 acromegaly patients (out of 1,066,871 people) were identified, resulting in a prevalence of 6.9 per 100,000 inhabitants [95% CI 5.4–8.5]. Prevalence was higher in females than men (p = 0.004), and showed a statistically significant trend of increase over time (p < 0.0001). Overall, incidence during the study period was 0.31 per 100,000 person-years. Hypertension and type II diabetes mellitus were the comorbidities more frequently associated with acromegaly (31.3 and 14.6%, respectively) and patients were more likely to undergo a high frequency of yearly hospitalization (≥3 accesses/year, p < 0.001) compared to sex-age matched controls.
Conclusions
This epidemiological study on acromegaly carried out using a large GP-based database, documented a disease prevalence of about 7 cases per 100,000 inhabitants. As expected, acromegaly was associated with a number of comorbidities (mainly hypertension and type II diabetes mellitus) and a high rate of patients’ hospitalization.



Similar content being viewed by others
References
S. Melmed, Medical progress: acromegaly. N. Engl. J. Med. 355(24), 2558–2573 (2006). https://doi.org/10.1056/NEJMra062453
F.G. Davis, V. Kupelian, S. Freels, B. McCarthy, T. Surawicz, Prevalence estimates for primary brain tumors in the United States by behavior and major histology groups. Neuro. Oncol. 3(3), 152–158 (2001)
A. Lavrentaki, A. Paluzzi, J.A. Wass, N. Karavitaki, Epidemiology of acromegaly: review of population studies. Pituitary 20(1), 4–9 (2017). https://doi.org/10.1007/s11102-016-0754-x
A. Fernandez, N. Karavitaki, J.A. Wass, Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin. Endocrinol. 72(3), 377–382 (2010). https://doi.org/10.1111/j.1365-2265.2009.03667.x
A.F. Daly, M. Rixhon, C. Adam, A. Dempegioti, M.A. Tichomirowa, A. Beckers, High prevalence of pituitary adenomas: a cross-sectional study in the province of Liege, Belgium. J. Clin. Endocrinol. Metab. 91(12), 4769–4775 (2006). https://doi.org/10.1210/jc.2006-1668
A. Raappana, J. Koivukangas, T. Ebeling, T. Pirila, Incidence of pituitary adenomas in Northern Finland in 1992-2007. J. Clin. Endocrinol. Metab. 95(9), 4268–4275 (2010). https://doi.org/10.1210/jc.2010-0537
T.T. Agustsson, T. Baldvinsdottir, J.G. Jonasson, E. Olafsdottir, V. Steinthorsdottir, G. Sigurdsson, A.V. Thorsson, P.V. Carroll, M. Korbonits, R. Benediktsson, The epidemiology of pituitary adenomas in Iceland, 1955-2012: a nationwide population-based study. Eur. J. Endocrinol. 173(5), 655–664 (2015). https://doi.org/10.1530/EJE-15-0189
T. Burton, E. Le Nestour, M. Neary, W.H. Ludlam, Incidence and prevalence of acromegaly in a large US health plan database. Pituitary 19(3), 262–267 (2016). https://doi.org/10.1007/s11102-015-0701-2
M. Bex, R. Abs, G. T’Sjoen, J. Mockel, B. Velkeniers, K. Muermans, D. Maiter, AcroBel--the Belgian registry on acromegaly: a survey of the ‘real-life’ outcome in 418 acromegalic subjects. Eur. J. Endocrinol. 157(4), 399–409 (2007). https://doi.org/10.1530/EJE-07-0358
A. Tjornstrand, K. Gunnarsson, M. Evert, E. Holmberg, O. Ragnarsson, T. Rosen, H. Filipsson Nystrom, The incidence rate of pituitary adenomas in western Sweden for the period 2001-2011. Eur. J. Endocrinol. 171(4), 519–526 (2014). https://doi.org/10.1530/EJE-14-0144
J. Dal, U. Feldt-Rasmussen, M. Andersen, L.O. Kristensen, P. Laurberg, L. Pedersen, O.M. Dekkers, H.T. Sorensen, J.O. Jorgensen, Acromegaly incidence, prevalence, complications and long-term prognosis: a nationwide cohort study. Eur. J. Endocrinol. 175(3), 181–190 (2016). https://doi.org/10.1530/EJE-16-0117
A. Mestron, S.M. Webb, R. Astorga, P. Benito, M. Catala, S. Gaztambide, J.M. Gomez, I. Halperin, T. Lucas-Morante, B. Moreno, G. Obiols, P. de Pablos, C. Paramo, A. Pico, E. Torres, C. Varela, J.A. Vazquez, J. Zamora, M. Albareda, M. Gilabert, Epidemiology, clinical characteristics, outcome, morbidity and mortality in acromegaly based on the Spanish Acromegaly Registry (Registro Espanol de Acromegalia, REA). Eur. J. Endocrinol. 151(4), 439–446 (2004)
G.T. Hoskuldsdottir, S.B. Fjalldal, H.A. Sigurjonsdottir, The incidence and prevalence of acromegaly, a nationwide study from 1955 through 2013. Pituitary 18(6), 803–807 (2015). https://doi.org/10.1007/s11102-015-0655-4
S. Ezzat, S.L. Asa, W.T. Couldwell, C.E. Barr, W.E. Dodge, M.L. Vance, I.E. McCutcheon, The prevalence of pituitary adenomas: a systematic review. Cancer 101(3), 613–619 (2004). https://doi.org/10.1002/cncr.20412
A. Colao, D. Ferone, P. Marzullo, G. Lombardi, Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr. Rev. 25(1), 102–152 (2004). https://doi.org/10.1210/er.2002-0022
L. Katznelson, E.R. Laws Jr., S. Melmed, M.E. Molitch, M.H. Murad, A. Utz, J.A. Wass, S. Endocrine, Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 99(11), 3933–3951 (2014). https://doi.org/10.1210/jc.2014-2700
S.M. Webb, X. Badia, Quality of Life in Acromegaly. Neuroendocrinology 103(1), 106–111 (2016). https://doi.org/10.1159/000375451
T. Brue, F. Castinetti, The risks of overlooking the diagnosis of secreting pituitary adenomas. Orphanet. J. Rare. Dis. 11(1), 135 (2016). https://doi.org/10.1186/s13023-016-0516-x
I.M. Holdaway, R.C. Rajasoorya, G.D. Gamble, Factors influencing mortality in acromegaly. J. Clin. Endocrinol. Metab. 89(2), 667–674 (2004). https://doi.org/10.1210/jc.2003-031199
R. Kauppinen-Makelin, T. Sane, A. Reunanen, M.J. Valimaki, L. Niskanen, H. Markkanen, E. Loyttyniemi, T. Ebeling, P. Jaatinen, H. Laine, P. Nuutila, P. Salmela, J. Salmi, U.H. Stenman, J. Viikari, E. Voutilainen, A nationwide survey of mortality in acromegaly. J. Clin. Endocrinol. Metab. 90(7), 4081–4086 (2005). https://doi.org/10.1210/jc.2004-1381
I.M. Holdaway, M.J. Bolland, G.D. Gamble, A meta-analysis of the effect of lowering serum levels of GH and IGF-I on mortality in acromegaly. Eur. J. Endocrinol. 159(2), 89–95 (2008). https://doi.org/10.1530/EJE-08-0267
M. Arosio, G. Reimondo, E. Malchiodi, P. Berchialla, A. Borraccino, L. De Marinis, R. Pivonello, S. Grottoli, M. Losa, S. Cannavo, F. Minuto, M. Montini, M. Bondanelli, E. De Menis, C. Martini, G. Angeletti, A. Velardo, A. Peri, M. Faustini-Fustini, P. Tita, F. Pigliaru, G. Borretta, C. Scaroni, N. Bazzoni, A. Bianchi, M. Appetecchia, F. Cavagnini, G. Lombardi, E. Ghigo, P. Beck-Peccoz, A. Colao, M. Terzolo; Italian Study Group of, A., Predictors of morbidity and mortality in acromegaly: an Italian survey. Eur. J. Endocrinol. 167(2), 189–198 (2012). https://doi.org/10.1530/EJE-12-0084
L. Maione, T. Brue, A. Beckers, B. Delemer, P. Petrossians, F. Borson-Chazot, O. Chabre, P. Francois, J. Bertherat, C. Cortet-Rudelli, P. Chanson; French Acromegaly Registry, G., Changes in the management and comorbidities of acromegaly over three decades: the French Acromegaly Registry. Eur. J. Endocrinol. 176(5), 645–655 (2017). https://doi.org/10.1530/EJE-16-1064
A. Giustina, P. Chanson, D. Kleinberg, M.D. Bronstein, D.R. Clemmons, A. Klibanski, A.J. van der Lely, C.J. Strasburger, S.W. Lamberts, K.K. Ho, F.F. Casanueva, S. Melmed; Acromegaly Consensus, G., Expert consensus document: a consensus on the medical treatment of acromegaly. Nature reviews. Endocrinology 10(4), 243–248 (2014). https://doi.org/10.1038/nrendo.2014.21
E. Lesen, D. Granfeldt, A. Houchard, J. Dinet, A. Berthon, D.S. Olsson, I. Bjorholt, G. Johannsson, Comorbidities, treatment patterns and cost-of-illness of acromegaly in Sweden: a register-linkage population-based study. Eur. J. Endocrinol. 176(2), 203–212 (2017). https://doi.org/10.1530/EJE-16-0623
M.S. Broder, M.P. Neary, E. Chang, D. Cherepanov, L. Katznelson, Treatments, complications, and healthcare utilization associated with acromegaly: a study in two large United States databases. Pituitary 17(4), 333–341 (2014). https://doi.org/10.1007/s11102-013-0506-0
C. Cricelli, G. Mazzaglia, F. Samani, M. Marchi, A. Sabatini, R. Nardi, G. Ventriglia, A.P. Caputi, Prevalence estimates for chronic diseases in Italy: exploring the differences between self-report and primary care databases. J. Public Health Med. 25(3), 254–257 (2003)
G. Trifiro, P. Morabito, L. Cavagna, C. Ferrajolo, S. Pecchioli, M. Simonetti, E. Bianchini, G. Medea, C. Cricelli, A.P. Caputi, G. Mazzaglia, Epidemiology of gout and hyperuricaemia in Italy during the years 2005-2009: a nationwide population-based study. Ann. Rheum. Dis. 72(5), 694–700 (2013). https://doi.org/10.1136/annrheumdis-2011-201254
G. Mazzaglia, E. Ambrosioni, M. Alacqua, A. Filippi, E. Sessa, V. Immordino, C. Borghi, O. Brignoli, A.P. Caputi, C. Cricelli, L.G. Mantovani, Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 120(16), 1598–1605 (2009). https://doi.org/10.1161/CIRCULATIONAHA.108.830299
J. Etxabe, S. Gaztambide, P. Latorre, J.A. Vazquez, Acromegaly: an epidemiological study. J. Endocrinol. Invest. 16(3), 181–187 (1993). https://doi.org/10.1007/BF03344942
I.M. Holdaway, C. Rajasoorya, Epidemiology of acromegaly. Pituitary 2(1), 29–41 (1999)
L.A. Naves, L.B. Porto, J.W. Rosa, L.A. Casulari, J.W. Rosa, Geographical information system (GIS) as a new tool to evaluate epidemiology based on spatial analysis and clinical outcomes in acromegaly. Pituitary 18(1), 8–15 (2015). https://doi.org/10.1007/s11102-013-0548-3
S. Cannavo, F. Ferrau, M. Ragonese, L. Curto, M.L. Torre, M. Magistri, A. Marchese, A. Alibrandi, F. Trimarchi, Increased prevalence of acromegaly in a highly polluted area. Eur. J. Endocrinol. 163(4), 509–513 (2010). https://doi.org/10.1530/EJE-10-0465
M. Gruppetta, C. Mercieca, J. Vassallo, Prevalence and incidence of pituitary adenomas: a population based study in Malta. Pituitary 16(4), 545–553 (2013). https://doi.org/10.1007/s11102-012-0454-0
J. Dal, N. Skou, E.H. Nielsen, J.O. Jorgensen, L. Pedersen, Acromegaly according to the Danish National Registry of Patients: how valid are ICD diagnoses and how do patterns of registration affect the accuracy of registry data? Clin. Epidemiol. 6, 295–299 (2014). https://doi.org/10.2147/CLEP.S63758
S. Fieffe, I. Morange, P. Petrossians, P. Chanson, V. Rohmer, C. Cortet, F. Borson-Chazot, T. Brue, B. Delemer; French Acromegaly, R., Diabetes in acromegaly, prevalence, risk factors, and evolution: data from the French Acromegaly Registry. Eur. J. Endocrinol. 164(6), 877–884 (2011). https://doi.org/10.1530/EJE-10-1050
S. Petersenn, M. Buchfelder, M. Reincke, C.M. Strasburger, H. Franz, R. Lohmann, H.J. Quabbe, U. Plockinger, Participants of the German Acromegaly, R.: Results of surgical and somatostatin analog therapies and their combination in acromegaly: a retrospective analysis of the German Acromegaly Register. Eur. J. Endocrinol. 159(5), 525–532 (2008). https://doi.org/10.1530/EJE-08-0498
L.A. Portocarrero-Ortiz, A. Vergara-Lopez, M. Vidrio-Velazquez, A.M. Uribe-Diaz, A. Garcia-Dominguez, A.A. Reza-Albarran, D. Cuevas-Ramos, V. Melgar, J. Talavera, A.J. Rivera-Hernandez, C.V. Valencia-Mendez, M. Mercado, Mexican Acromegaly Registry, G.: The Mexican Acromegaly Registry: Clinical and Biochemical Characteristics at Diagnosis and Therapeutic Outcomes. J. Clin. Endocrinol. Metab. 101(11), 3997–4004 (2016). https://doi.org/10.1210/jc.2016-1937
P. Petrossians, A.F. Daly, E. Natchev, L. Maione, K. Blijdorp, M. Sahnoun-Fathallah, R. Auriemma, A.M. Diallo, A.L. Hulting, D. Ferone, V. Hana Jr., S. Filipponi, C. Sievers, C. Nogueira, C. Fajardo-Montanana, D. Carvalho, V. Hana, G.K. Stalla, M.L. Jaffrain-Rea, B. Delemer, A. Colao, T. Brue, S. Neggers, S. Zacharieva, P. Chanson, A. Beckers, Acromegaly at diagnosis in 3173 patients from the Liege Acromegaly Survey (LAS) Database. Endocr.-Relat. Cancer 24(10), 505–518 (2017). https://doi.org/10.1530/ERC-17-0253
O. Kwon, Y.D. Song, S.Y. Kim, E.J. Lee; Rare Disease Study Group, S., Research Committee, K.E.S., Nationwide survey of acromegaly in South Korea. Clin. Endocrinol. 78(4), 577–585 (2013). https://doi.org/10.1111/cen.12020
M. Bondanelli, M.R. Ambrosio, E.C. degli Uberti, Pathogenesis and prevalence of hypertension in acromegaly. Pituitary 4(4), 239–249 (2001)
R. Gini, M.J. Schuemie, G. Mazzaglia, F. Lapi, P. Francesconi, A. Pasqua, E. Bianchini, C. Montalbano, G. Roberto, V. Barletta, I. Cricelli, C. Cricelli, G. Dal Co, M. Bellentani, M. Sturkenboom, N. Klazinga, Automatic identification of type 2 diabetes, hypertension, ischaemic heart disease, heart failure and their levels of severity from Italian General Practitioners’ electronic medical records: a validation study. BMJ Open 6(12), e012413 (2016). https://doi.org/10.1136/bmjopen-2016-012413
T.J. Reid, K.D. Post, J.N. Bruce, M. Nabi Kanibir, C.M. Reyes-Vidal, P.U. Freda, Features at diagnosis of 324 patients with acromegaly did not change from 1981 to 2006: acromegaly remains under-recognized and under-diagnosed. Clin. Endocrinol. 72(2), 203–208 (2010). https://doi.org/10.1111/j.1365-2265.2009.03626.x
T. Burton, E. Le Nestour, T. Bancroft, M. Neary, Real-world comorbidities and treatment patterns of patients with acromegaly in two large US health plan databases. Pituitary 16(3), 354–362 (2013). https://doi.org/10.1007/s11102-012-0432-6
Funding:
This research received the unconditional support of Pfizer srl.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F.G. received fees for lectures and/or participation to advisory boards for Novartis, AMCo, and IONIS Pharmaceuticals. D.F. received grants and fees for lectures and participation to advisory boards for Novartis, Ipsen, and Pfizer. The remaining authors have declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Gatto, F., Trifirò, G., Lapi, F. et al. Epidemiology of acromegaly in Italy: analysis from a large longitudinal primary care database. Endocrine 61, 533–541 (2018). https://doi.org/10.1007/s12020-018-1630-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1630-4