Abstract
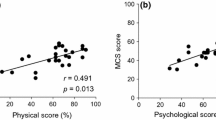
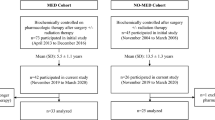
Various factors influence quality of life (QoL) in acromegaly. Whether disease control and treatment approach are related to QoL is still a matter of debate. The aim of the present study was to evaluate QoL in patients with acromegaly using the disease-specific Acromegaly Quality of Life Questionnaire in respect to disease activity, treatment modalities, and other factors. We studied 212 patients with acromegaly in a cross-sectional manner over a 6-year period in a single tertiary center. As a second step, seventy of the patients who were with active disease at baseline were followed up prospectively and 45 of them were in remission at re-evaluation. In regard to the cross-sectional group, active acromegaly independently predicted worse appearance scores. Prior radiotherapy and older age were independent negative predictors of all scales. Female gender negatively predicted all scales except the appearance domain. Longer duration of remission predicted worse personal relations scores in biochemically controlled patients. The use of somatostatin analog (SSA) was associated with worse personal relations scores, while higher IGF-1 index predicted worse appearance scores in patients with active acromegaly. In the prospective group, achievement of remission independently predicted improvement of the total scale. Lower corresponding baseline scores predicted improvement of the total, physical, and appearance scales, while the absence of hypopituitarism independently predicted improvement of the appearance scale. The use of SSA was associated with improvement of the total and appearance scores. In conclusion, QoL is a multifactorial issue that needs an individualized approach for detection and management.

Similar content being viewed by others
References
O.M. Dekkers, N.R. Biermasz, A.M. Pereira, J.A. Romijn, J.P. Vandenbroucke, Mortality in acromegaly: a metaanalysis. J. Clin. Endocrinol. Metab. 93(1), 61–67 (2008). doi:10.1210/jc.2007-1191
A. Santos, E. Resmini, M.A. Martinez, C. Marti, J. Ybarra, S.M. Webb, Quality of life in patients with pituitary tumors. Curr. Opin. Endocrinol. Diabetes Obes. 16(4), 299–303 (2009). doi:10.1097/MED.0b013e32832cdec9
S.M. Webb, X. Badia, N.L. Surinach, Validity and clinical applicability of the acromegaly quality of life questionnaire, AcroQoL: a 6-month prospective study. Eur. J. Endocrinol. 155(2), 269–277 (2006). doi:10.1530/eje.1.02214
N.R. Biermasz, S.W. van Thiel, A.M. Pereira, H.C. Hoftijzer, A.M. van Hemert, J.W. Smit, J.A. Romijn, F. Roelfsema, Decreased quality of life in patients with acromegaly despite long-term cure of growth hormone excess. J. Clin. Endocrinol. Metab. 89(11), 5369–5376 (2004). doi:10.1210/jc.2004-0669
S.V. Rowles, L. Prieto, X. Badia, S.M. Shalet, S.M. Webb, P.J. Trainer, Quality of life (QOL) in patients with acromegaly is severely impaired: use of a novel measure of QOL: acromegaly quality of life questionnaire. J. Clin. Endocrinol. Metab. 90(6), 3337–3341 (2005). doi:10.1210/jc.2004-1565
S.C. Hua, Y.H. Yan, T.C. Chang, Associations of remission status and lanreotide treatment with quality of life in patients with treated acromegaly. Eur. J. Endocrinol. 155(6), 831–837 (2006). doi:10.1530/eje.1.02292
G. T’Sjoen, M. Bex, D. Maiter, B. Velkeniers, R. Abs, Health-related quality of life in acromegalic subjects: data from AcroBel, the Belgian registry on acromegaly. Eur. J. Endocrinol. 157(4), 411–417 (2007). doi:10.1530/EJE-07-0356
R. Trepp, R. Everts, C. Stettler, S. Fischli, S. Allemann, S.M. Webb, E.R. Christ, Assessment of quality of life in patients with uncontrolled vs. controlled acromegaly using the Acromegaly Quality of Life questionnaire (AcroQoL). Clin. Endocrinol. (Oxf) 63(1), 103–110 (2005). doi:10.1111/j.1365-2265.2005.02307.x
M.P. Matta, E. Couture, L. Cazals, D. Vezzosi, A. Bennet, P. Caron, Impaired quality of life of patients with acromegaly: control of GH/IGF-I excess improves psychological subscale appearance. Eur. J. Endocrinol. 158(3), 305–310 (2008). doi:10.1530/EJE-07-0697
C. Sardella, M. Lombardi, G. Rossi, C. Cosci, S. Brogioni, I. Scattina, S.M. Webb, M. Gasperi, E. Martino, F. Bogazzi, Short- and long-term changes of quality of life in patients with acromegaly: results from a prospective study. J. Endocrinol. Invest. 33(1), 20–25 (2010)
H. Kepicoglu, E. Hatipoglu, I. Bulut, E. Darici, N. Hizli, P. Kadioglu, Impact of treatment satisfaction on quality of life of patients with acromegaly. Pituitary (2013). doi:10.1007/s11102-013-0544-7
N.R. Biermasz, A.M. Pereira, J.W. Smit, J.A. Romijn, F. Roelfsema, Morbidity after long-term remission for acromegaly: persisting joint-related complaints cause reduced quality of life. J. Clin. Endocrinol. Metab. 90(5), 2731–2739 (2005). doi:10.1210/jc.2004-2297
S.J. Neggers, M.O. van Aken, W.W. de Herder, R.A. Feelders, J.A. Janssen, X. Badia, S.M. Webb, A.J. van der Lely, Quality of life in acromegalic patients during long-term somatostatin analog treatment with and without pegvisomant. J. Clin. Endocrinol. Metab. 93(10), 3853–3859 (2008). doi:10.1210/jc.2008-0669
M.R. Postma, R.T. Netea-Maier, G. van den Berg, J. Homan, W.J. Sluiter, M.A. Wagenmakers, A.C. van den Bergh, B.H. Wolffenbuttel, A.R. Hermus, A.P. van Beek, Quality of life is impaired in association with the need for prolonged postoperative therapy by somatostatin analogs in patients with acromegaly. Eur. J. Endocrinol. 166(4), 585–592 (2012). doi:10.1530/EJE-11-0853
R. Mangupli, P. Camperos, S.M. Webb, Biochemical and quality of life responses to octreotide-LAR in acromegaly. Pituitary (2013). doi:10.1007/s11102-013-0533-x
A.A. van der Klaauw, N.R. Biermasz, H.C. Hoftijzer, A.M. Pereira, J.A. Romijn, Previous radiotherapy negatively influences quality of life during 4 years of follow-up in patients cured from acromegaly. Clin. Endocrinol. (Oxf) 69(1), 123–128 (2008). doi:10.1111/j.1365-2265.2007.03169.x
E. Hatipoglu, N. Topsakal, O.E. Atilgan, N. Alcalar, A.F. Camliguney, M. Niyazoglu, H.B. Cotuk, P. Kadioglu, Impact of exercise on quality of life and body-self perception of patients with acromegaly. Pituitary 17(1), 38–43 (2014). doi:10.1007/s11102-013-0463-7
S.M. Webb, L. Prieto, X. Badia, M. Albareda, M. Catala, S. Gaztambide, T. Lucas, C. Paramo, A. Pico, A. Lucas, I. Halperin, G. Obiols, R. Astorga, Acromegaly Quality of Life Questionnaire (ACROQOL) a new health-related quality of life questionnaire for patients with acromegaly: development and psychometric properties. Clin. Endocrinol. (Oxf) 57(2), 251–258 (2002)
A. Giustina, A. Barkan, F.F. Casanueva, F. Cavagnini, L. Frohman, K. Ho, J. Veldhuis, J. Wass, K. Von Werder, S. Melmed, Criteria for cure of acromegaly: a consensus statement. J. Clin. Endocrinol. Metab. 85(2), 526–529 (2000)
M.C. Sheppard, Growth hormone assay standardization: an important clinical advance. Clin. Endocrinol. (Oxf) 66(2), 157–161 (2007). doi:10.1111/j.1365-2265.2007.02703.x
A.N. Paisley, S.V. Rowles, M.E. Roberts, S.M. Webb, X. Badia, L. Prieto, S.M. Shalet, P.J. Trainer, Treatment of acromegaly improves quality of life, measured by AcroQol. Clin. Endocrinol. (Oxf) 67(3), 358–362 (2007). doi:10.1111/j.1365-2265.2007.02891.x
P. Anagnostis, Z.A. Efstathiadou, M. Charizopoulou, D. Selalmatzidou, E. Karathanasi, M. Poulasouchidou, M. Kita, Psychological profile and quality of life in patients with acromegaly in Greece. Is there any difference with other chronic diseases? Endocrine (2014). doi:10.1007/s12020-014-0166-5
M.J. Wassenaar, N.R. Biermasz, M. Kloppenburg, A.A. van der Klaauw, J. Tiemensma, J.W. Smit, A.M. Pereira, F. Roelfsema, H.M. Kroon, J.A. Romijn, Clinical osteoarthritis predicts physical and psychological QoL in acromegaly patients. Growth Horm IGF Res. 20(3), 226–233 (2010). doi:10.1016/j.ghir.2010.02.003
B.J. Spiegler, E. Bouffet, M.L. Greenberg, J.T. Rutka, D.J. Mabbott, Change in neurocognitive functioning after treatment with cranial radiation in childhood. J. Clin. Oncol. 22(4), 706–713 (2004). doi:10.1200/JCO.2004.05.186
A. Miller, H. Doll, J. David, J. Wass, Impact of musculoskeletal disease on quality of life in long-standing acromegaly. Eur. J. Endocrinol. 158(5), 587–593 (2008). doi:10.1530/EJE-07-0838
P.J. Jenkins, P. Bates, M.N. Carson, P.M. Stewart, J.A. Wass, Conventional pituitary irradiation is effective in lowering serum growth hormone and insulin-like growth factor-I in patients with acromegaly. J. Clin. Endocrinol. Metab. 91(4), 1239–1245 (2006). doi:10.1210/jc.2005-1616
S.J. Neggers, J.J. Kopchick, J.O. Jorgensen, A.J. van der Lely, Hypothesis: extra-hepatic acromegaly: a new paradigm? Eur. J. Endocrinol. 164(1), 11–16 (2011). doi:10.1530/EJE-10-0969
T. Psaras, J. Honegger, B. Gallwitz, M. Milian, Are there gender-specific differences concerning quality of life in treated acromegalic patients? Exp. Clin. Endocrinol. Diabetes 119(5), 300–305 (2011). doi:10.1055/s-0030-1267912
A.P. Arnold, Promoting the understanding of sex differences to enhance equity and excellence in biomedical science. Biol. Sex Differ. 1(1), 1 (2010). doi:10.1186/2042-6410-1-1
T. Wexler, L. Gunnell, Z. Omer, K. Kuhlthau, C. Beauregard, G. Graham, A.L. Utz, B. Biller, L. Nachtigall, J. Loeffler, B. Swearingen, A. Klibanski, K.K. Miller, Growth hormone deficiency is associated with decreased quality of life in patients with prior acromegaly. J. Clin. Endocrinol. Metab. 94(7), 2471–2477 (2009). doi:10.1210/jc.2008-2671
Acknowledgments
This work has been supported by the National Science Fund, Ministry of Education, Youth and Science, Grant No. DO02-356/31.12.2008.
Conflict of interest
The authors declare that there is no conflict of interest that would prejudice the impartiality of the reported scientific work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vandeva, S., Yaneva, M., Natchev, E. et al. Disease control and treatment modalities have impact on quality of life in acromegaly evaluated by Acromegaly Quality of Life (AcroQoL) Questionnaire. Endocrine 49, 774–782 (2015). https://doi.org/10.1007/s12020-014-0521-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0521-6