Abstract
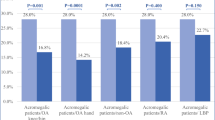
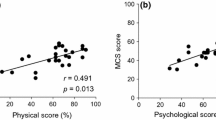
Several studies have shown that acromegaly is associated with increased psychological morbidity. However, it is not known whether this is attributed to acromegaly per se or to its chronicity as a debilitating disease affecting quality of life (QoL). The aim of this study was to assess psychological profile in acromegalics compared with those suffering from other serious chronic diseases and healthy controls. Secondary end points were QoL assessment and its association with mood disturbances. Comparative, cross-sectional study conducted in Northern Greece (2011–2012). The Greek versions of the Profile of Mood States (POMS) and AcroQoL questionnaires were used to assess psychological status and QoL, respectively. Forty acromegalics, 40 age- and sex-matched people with other chronic diseases and 80 healthy controls were included. No significant differences were identified between acromegalics and those suffering from other chronic diseases, regarding tension, anger, depression, confusion, fatigue and vigor. Compared with healthy controls, acromegalics suffered more from depression and anger, which remained significant after controlling for age, gender and marital status (p = 0.003 and p = 0.048, respectively). Negative predictors were female gender, macroadenomas and radiotherapy. AcroQoL scores were negatively associated with POMS subscales. Males had better QoL than females. Other than a negative association between AcroQoL-relationships subscale and disease duration, no association with other parameters was observed. Acromegaly has a negative impact on psychological status, which is worse than that of general population, but comparable to other chronic diseases. Mood disturbances are associated with impaired QoL, mainly in females and those with longer disease duration.
Similar content being viewed by others
References
P. Anagnostis, Z.A. Efstathiadou, S.A. Polyzos, F. Adamidou, A. Slavakis, M. Sapranidis, I.D. Litsas, S. Katergari, D. Selalmatzidou, M. Kita, Acromegaly: presentation, morbidity and treatment outcomes at a single centre. Int. J. Clin. Pract. 65, 896–902 (2011)
P. Anagnostis, Z.A. Efstathiadou, S. Gougoura, S.A. Polyzos, E. Karathanasi, P. Dritsa, M. Kita, G.N. Koukoulis, Oxidative stress and reduced antioxidative status, along with endothelial dysfunction in acromegaly. Horm. Metab. Res. 45, 314–318 (2013)
L.J. Woodhouse, A. Mukherjee, S.M. Shalet, S. Ezzat, The influence of growth hormone status on physical impairments, functional limitations, and health-related quality of life in adults. Endocr. Rev. 27, 287–317 (2006)
T.J. Reid, K.D. Post, J.N. Bruce, M. Nabi Kanibir, C.M. Reyes-Vidal, P.U. Freda, Features at diagnosis of 324 patients with acromegaly did not change from 1981 to 2006: acromegaly remains under-recognized and under-diagnosed. Clin. Endocrinol. (Oxf) 72, 203–208 (2010)
S.M. Webb, Quality of life in acromegaly. Neuroendocrinology 83, 224–229 (2006)
S.C. Hua, Y.H. Yan, T.C. Chang, Associations of remission status and lanreotide treatment with quality of life in patients with treated acromegaly. Eur. J. Endocrinol. 155, 831–837 (2006)
M.P. Matta, E. Couture, L. Cazals, D. Vezzosi, A. Bennet, P. Caron, Impaired quality of life of patients with acromegaly: control of GH/IGF-I excess improves psychological subscale appearance. Eur. J. Endocrinol. 158, 305–310 (2008)
J. Leon-Carrion, J.F. Martin-Rodriguez, A. Madrazo-Atutxa, A. Soto-Moreno, E. Venegas-Moreno, E. Torres-Vela, P. Benito-López, M.A. Gálvez, F.J. Tinahones, A. Leal-Cerro, Evidence of cognitive and neurophysiological impairment in patients with untreated naive acromegaly. J. Clin. Endocrinol. Metab. 95, 4367–4379 (2010)
C. Sievers, M. Ising, H. Pfister, C. Dimopoulou, H.J. Schneider, J. Roemmler, J. Schopohl, G.K. Stalla, Personality in patients with pituitary adenomas is characterized by increased anxiety-related traits: comparison of 70 acromegalic patients with patients with non-functioning pituitary adenomas and age- and gender-matched controls. Eur. J. Endocrinol. 160, 367–373 (2009)
A. Margo, Acromegaly and depression. Br. J. Psychiatry 139, 467–468 (1981)
A. Giustina, P. Chanson, M.D. Bronstein, A. Klibanski, S. Lamberts, F.F. Casanueva, P. Trainer, E. Ghigo, K. Ho, S. Melmed, Acromegaly Consensus Group, A consensus on criteria for cure of acromegaly. J. Clin. Endocrinol. Metab. 95, 3141–3148 (2010)
P. Anagnostis, F. Adamidou, S.A. Polyzos, Z. Efstathiadou, A. Panagiotou, M. Kita, Non-functioning pituitary adenomas: a single center experience. Exp. Clin. Endocrinol. Diabetes 119, 314–319 (2011)
D.M. McNair, M. Lorr, L.F. Droppleman, EITS manual for the Profile of Mood States (Educational and Industrial Testing Service, San Diego, CA, 1971)
K.W. Wyrwich, H. Yu, Validation of POMS questionnaire in postmenopausal women. Qual. Life Res. 20, 1111–1121 (2011)
F. Baker, M. Denniston, J. Zabora, A. Polland, W.N. Dudley, A POMS short form for cancer patients: psychometric and structural evaluation. Psychooncology 11, 273–281 (2002)
S.M. Webb, L. Prieto, X. Badia, M. Albareda, M. Catala, S. Gaztambide, T. Lucas, C. Páramo, A. Pico, A. Lucas, I. Halperin, G. Obiols, R. Astorga, Acromegaly Quality of Life Questionnaire (ACROQOL) a new health-related quality of life questionnaire for patients with acromegaly: development and psychometric properties. Clin. Endocrinol. (Oxf) 57, 251–258 (2002)
S.M. Webb, X. Badia, N.L. Surinach, Spanish AcroQol Study Group, Validity and clinical applicability of the acromegaly quality of life questionnaire, AcroQoL: a 6-month prospective study. Eur. J. Endocrinol. 155, 269–277 (2006)
R. Kauppinen-Mäkelin, T. Sane, H. Sintonen, H. Markkanen, M.J. Välimäki, E. Löyttyniemi, L. Niskanen, A. Reunanen, U.H. Stenman, Quality of life in treated patients with acromegaly. J. Clin. Endocrinol. Metab. 91, 3891–3896 (2006)
C. Sardella, M. Lombardi, G. Rossi, C. Cosci, S. Brogioni, I. Scattina, S.M. Webb, M. Gasperi, E. Martino, F. Bogazzi, Short- and long-term changes of quality of life in patients with acromegaly: results from a prospective study. J. Endocrinol. Invest. 33, 20–25 (2010)
S.K. Mattoo, A.K. Bhansali, N. Gupta, S. Grover, R. Malhotra, Psychosocial morbidity in acromegaly: a study from India. Endocrine 34, 17–22 (2008)
A. Miller, H. Doll, J. David, J. Wass, Impact of musculoskeletal disease on quality of life in long-standing acromegaly. Eur. J. Endocrinol. 158, 587–593 (2008)
Yedinak, C.G., Fleseriu, M. Self-perception of cognitive function among patients with active acromegaly, controlled acromegaly, and non-functional pituitary adenoma: a pilot study. Endocrine. (2013). doi:10.1007/s12020-013-0106-9
T. Psaras, M. Milian, V. Hattermann, B.E. Will, M. Tatagiba, J. Honegger, Predictive factors for neurocognitive function and Quality of Life after surgical treatment for Cushing’s disease and acromegaly. J. Endocrinol. Invest. 34, e168–e177 (2011)
M. Ruchala, I. Stangierska, E. Gurgul, A. Stangierski, J. Fajfer, J. Sowinski, The effect of octreotide treatment on somatic and psychological symptoms of acromegaly. Neuro. Endocrinol. Lett. 31, 265–269 (2010)
C. Sievers, P.G. Sämann, T. Dose, C. Dimopoulou, D. Spieler, J. Roemmler, J. Schopohl, M. Mueller, H.J. Schneider, M. Czisch, H. Pfister, G.K. Stalla, Macroscopic brain architecture changes and white matter pathology in acromegaly: a clinicoradiological study. Pituitary. 12, 177–185 (2009)
M. Ziegenbein, K. Held, H.E. Kuenzel, H. Murck, I.A. Antonijevic, A. Steiger, The somatostatin analogue octreotide impairs sleep and decreases EEG sigma power in young male subjects. Neuropsychopharmacology 29, 146–151 (2004)
A.M. Peiffer, C.M. Leyrer, D.M. Greene-Schloesser, E. Shing, W.T. Kearns, W.H. Hinson, S.B. Tatter, E.H. Ip, S.R. Rapp, M.E. Robbins, E.G. Shaw, M.D. Chan, Neuroanatomical target theory as a predictive model for radiation-induced cognitive decline. Neurology. 80, 747–753 (2013)
N.P. Maric, M. Doknic, D. Pavlovic, S. Pekic, M. Stojanovic, M. Jasovic-Gasic, V. Popovic, Psychiatric and neuropsychological changes in growth hormone-deficient patients after traumatic brain injury in response to growth hormone therapy. J. Endocrinol. Invest. 33, 770–775 (2010)
M.J. Wassenaar, N.R. Biermasz, M. Kloppenburg, A.A. van der Klaauw, J. Tiemensma, J.W. Smit, A.M. Pereira, F. Roelfsema, H.M. Kroon, J.A. Romijn, Clinical osteoarthritis predicts physical and psychological QoL in acromegaly patients. Growth Horm IGF Res. 20, 226–233 (2010)
S. Siegel, C. Streetz-van der Werf, J.S. Schott, K. Nolte, W. Karges, I. Kreitschmann-Andermahr, Diagnostic delay is associated with psychosocial impairment in acromegaly. Pituitary. 16, 507–514 (2013)
A. Raappana, T. Pirilä, T. Ebeling, P. Salmela, H. Sintonen, J. Koivukangas, Long-term health-related quality of life of surgically treated pituitary adenoma patients: a descriptive study. ISRN. Endocrinol. 2012, 675310 (2012)
R. Trepp, R. Everts, C. Stettler, S. Fischli, S. Allemann, S.M. Webb, E.R. Christ, Assessment of quality of life in patients with uncontrolled vs. controlled acromegaly using the acromegaly quality of life questionnaire (AcroQoL). Clin. Endocrinol. (Oxf) 63, 103–110 (2005)
N.R. Biermasz, S.W. van Thiel, A.M. Pereira, H.C. Hoftijzer, A.M. van Hemert, J.W.A. Smit, J.A. Romijn, F. Roelfsema, Decreased quality of life in patients with acromegaly despite long-term cure of growth hormone excess. J. Clin. Endocrinol. Metab. 89, 5369–5376 (2004)
M.R. Postma, R.T. Netea-Maier, G. van den Berg, J. Homan, W.J. Sluiter, M.A. Wagenmakers, A.C. van den Bergh, B.H. Wolffenbuttel, A.R. Hermus, A.P. van Beek, Quality of life is impaired in association with the need for prolonged postoperative therapy by somatostatin analogs in patients with acromegaly. Eur. J. Endocrinol. 166, 585–592 (2012)
A.A. van der Klaauw, N.R. Biermasz, H.C. Hoftijzer, A.M. Pereira, J.A. Romijn, Previous radiotherapy negatively influences quality of life during 4 years of follow-up in patients cured from acromegaly. Clin. Endocrinol. (Oxf) 69, 123–128 (2008)
T. Wexler, L. Gunnell, Z. Omer, K. Kuhlthau, C. Beauregard, G. Graham, A.L. Utz, B. Biller, L. Nachtigall, J. Loeffler, B. Swearingen, A. Klibanski, K.K. Miller, Growth hormone deficiency is associated with decreased quality of life in patients with prior acromegaly. J. Clin. Endocrinol. Metab. 94, 2471–2477 (2009)
Conflicts of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anagnostis, P., Efstathiadou, Z.A., Charizopoulou, M. et al. Psychological profile and quality of life in patients with acromegaly in Greece. Is there any difference with other chronic diseases?. Endocrine 47, 564–571 (2014). https://doi.org/10.1007/s12020-014-0166-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0166-5