Abstract
Purpose of Review
Review epidemiology, pathophysiology, and management of hypertension in the pediatric dialysis population.
Recent Findings
Interdialytic blood pressure measurement, especially with ambulatory blood pressure monitoring, is the gold standard to assess for hypertension. Tools to assess dry weight aid in achievement of euvolemia, the primary therapy for management of hypertension. Persistent hypertension should be treated with antihypertensive medications and potentially with native nephrectomies.
Summary
Cardiovascular disease continues to be the primary cause of morbidity and mortality in the dialysis population with hypertension as an important modifiable factor. Achievement on dry weight and limiting both aggressiveness of interdialytic weight gain and ultrafiltration rate underlie the best approach. Tools to assess volume status beyond clinical assessment have shown promise in achieving euvolemia. When hypertension persists despite achievement of euvolemia, antihypertensive medications may be required and in some cases native nephrectomies. Future studies in children are needed to determine the best antihypertensive class and ideal rate of ultrafiltration on hemodialysis towards achievement of normotension and reduction of cardiovascular risk.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
2017 USRDS annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. In: Systems USRD, ed. Bethesda, MD2017.
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ. Epidemiology of chronic kidney disease in children. Pediatr Nephrol. 2012;27(3):363–73.
Mitsnefes MM. Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol. 2012;23(4):578–85.
• McDonald SP, Craig JC, Association AaNZPN. Long-term survival of children with end-stage renal disease. N Engl J Med. 2004;350(26):2654–62. Demonstrated the impact of cardiovascular disease among adults who had ESRD since childhood.
Groothoff JW, Gruppen MP, Offringa M, Hutten J, Lilien MR, van de Kar NJ, et al. Mortality and causes of death of end-stage renal disease in children: a Dutch cohort study. Kidney Int. 2002;61(2):621–9.
Parekh RS, Carroll CE, Wolfe RA, Port FK. Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr. 2002;141(2):191–7.
Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003;115(4):291–7.
• Halbach SM, Martz K, Mattoo T, Flynn J. Predictors of blood pressure and its control in pediatric patients receiving dialysis. J Pediatr. 2012;160(4):621–625.e621. This study, along with the study below, clarified the prevalence of hypertension in pediatric population.
• Kramer AM, van Stralen KJ, Jager KJ, et al. Demographics of blood pressure and hypertension in children on renal replacement therapy in Europe. Kidney Int. 2011;80(10):1092–8. This study, along with the study above, clarified the prevalence of hypertension in pediatric population.
Mitsnefes M, Flynn J, Cohn S, Samuels J, Blydt-Hansen T, Saland J, et al. Masked hypertension associates with left ventricular hypertrophy in children with CKD. J Am Soc Nephrol. 2010;21(1):137–44.
Bullington N, Kartel J, Khoury P, Mitsnefes M. Left ventricular hypertrophy in pediatric kidney transplant recipients: long-term follow-up study. Pediatr Transplant. 2006;10(7):811–5.
Sorof JM, Alexandrov AV, Cardwell G, Portman RJ. Carotid artery intimal-medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics. 2003;111(1):61–6.
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, et al. Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation. 2002;106(1):100–5.
Ahuja TS, Grady J, Khan S. Changing trends in the survival of dialysis patients with human immunodeficiency virus in the United States. J Am Soc Nephrol. 2002;13(7):1889–93.
• Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre- and postdialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol. 2006;1(3):389–98. Demonstrated peri-dialysis blood pressure measurements did not correlate with ambulatory blood pressure.
Agarwal R, Brim NJ, Mahenthiran J, Andersen MJ, Saha C. Out-of-hemodialysis-unit blood pressure is a superior determinant of left ventricular hypertrophy. Hypertension. 2006;47(1):62–8.
Moriya H, Ohtake T, Kobayashi S. Aortic stiffness, left ventricular hypertrophy and weekly averaged blood pressure (WAB) in patients on haemodialysis. Nephrol Dial Transplant. 2007;22(4):1198–204.
Moriya H, Oka M, Maesato K, Mano T, Ikee R, Ohtake T, et al. Weekly averaged blood pressure is more important than a single-point blood pressure measurement in the risk stratification of dialysis patients. Clin J Am Soc Nephrol. 2008;3(2):416–22.
Haskin O, Wong CJ, McCabe L, Begin B, Sutherland SM, Chaudhuri A. 44-h ambulatory blood pressure monitoring: revealing the true burden of hypertension in pediatric hemodialysis patients. Pediatr Nephrol. 2015;30(4):653–60.
Agarwal R. Blood pressure and mortality among hemodialysis patients. Hypertension. 2010;55(3):762–8.
• Alborzi P, Patel N, Agarwal R. Home blood pressures are of greater prognostic value than hemodialysis unit recordings. Clin J Am Soc Nephrol. 2007;2(6):1228–34. Demonstrated ambulatory blood pressure was more associated with mortality than peri-dialysis blood pressures.
Bircan Z, Duzova A, Cakar N, Bayazit AK, Elhan A, Tutar E, et al. Predictors of left ventricular hypertrophy in children on chronic peritoneal dialysis. Pediatr Nephrol. 2010;25(7):1311–8.
Ozçakar ZB, Yalçinkaya F, Tutar E, et al. Hypertension and left ventricular hypertrophy in pediatric peritoneal dialysis patients: ambulatory blood pressure monitoring and echocardiographic evaluation. Nephron Clin Pract. 2006;104(2):c101–6.
Tkaczyk M, Nowicki M, Bałasz-Chmielewska I, Boguszewska-Bączkowska H, Drożdż D, Kołłątaj B, et al. Hypertension in dialysed children: the prevalence and therapeutic approach in Poland—a nationwide survey. Nephrol Dial Transplant. 2006;21(3):736–42.
Zaloszyc A, Schaefer B, Schaefer F, Krid S, Salomon R, Niaudet P, et al. Hydration measurement by bioimpedance spectroscopy and blood pressure management in children on hemodialysis. Pediatr Nephrol. 2013;28(11):2169–77.
Twardowski ZJ. Sodium, hypertension, and an explanation of the “lag phenomenon” in hemodialysis patients. Hemodial Int. 2008;12(4):412–25.
Jaeger JQ, Mehta RL. Assessment of dry weight in hemodialysis: an overview. J Am Soc Nephrol. 1999;10(2):392–403.
Zhu F, Rosales L, Kotanko P. Techniques for assessing fluids status in patients with kidney disease. Curr Opin Nephrol Hypertens. 2016;25(6):473–9.
Dou Y, Zhu F, Kotanko P. Assessment of extracellular fluid volume and fluid status in hemodialysis patients: current status and technical advances. Semin Dial. 2012;25(4):377–87.
Lukaski HC, Bolonchuk WW. Estimation of body fluid volumes using tetrapolar bioelectrical impedance measurements. Aviat Space Environ Med. 1988;59(12):1163–9.
Kouw PM, Olthof CG, ter Wee PM, Oe LP, Donker AJM, Schneider H, et al. Assessment of post-dialysis dry weight: an application of the conductivity measurement method. Kidney Int. 1992;41(2):440–4.
Oh G, Wong C, Begin B, Salsbery K, Sutherland S, Chaudhuri A. Whole-body single-frequency bioimpedance analysis in pediatric hemodialysis patients. Pediatr Nephrol. 2014;29(8):1417–23.
Paglialonga F, Ardissino G, Galli MA, Scarfia RV, Testa S, Edefonti A. Bioimpedance analysis and cardiovascular status in pediatric patients on chronic hemodialysis. Hemodial Int. 2012;16(Suppl 1):S20–5.
Allinovi M, Saleem M, Romagnani P, Nazerian P, Hayes W. Lung ultrasound: a novel technique for detecting fluid overload in children on dialysis. Nephrol Dial Transplant. 2017;32(3):541–7.
Trezzi M, Torzillo D, Ceriani E, Costantino G, Caruso S, Damavandi PT, et al. Lung ultrasonography for the assessment of rapid extravascular water variation: evidence from hemodialysis patients. Intern Emerg Med. 2013;8(5):409–15.
Noble VE, Murray AF, Capp R, Sylvia-Reardon MH, Steele DJR, Liteplo A. Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest. 2009;135(6):1433–9.
Vitturi N, Dugo M, Soattin M, Simoni F, Maresca L, Zagatti R, et al. Lung ultrasound during hemodialysis: the role in the assessment of volume status. Int Urol Nephrol. 2014;46(1):169–74.
Basso F, Milan Manani S, Cruz DN, Teixeira C, Brendolan A, Nalesso F, et al. Comparison and reproducibility of techniques for fluid status assessment in chronic hemodialysis patients. Cardiorenal Med. 2013;3(2):104–12.
Zoccali C, Tripepi R, Torino C, Bellantoni M, Tripepi G, Mallamaci F. Lung congestion as a risk factor in end-stage renal disease. Blood Purif. 2013;36(3–4):184–91.
Torino C, Gargani L, Sicari R, Letachowicz K, Ekart R, Fliser D, et al. The agreement between auscultation and lung ultrasound in hemodialysis patients: the LUST study. Clin J Am Soc Nephrol. 2016;11(11):2005–11.
Siriopol D, Hogas S, Voroneanu L, Onofriescu M, Apetrii M, Oleniuc M, et al. Predicting mortality in haemodialysis patients: a comparison between lung ultrasonography, bioimpedance data and echocardiography parameters. Nephrol Dial Transplant. 2013;28(11):2851–9.
Allinovi M, Saleem MA, Burgess O, Armstrong C, Hayes W. Finding covert fluid: methods for detecting volume overload in children on dialysis. Pediatr Nephrol. 2016;31(12):2327–35.
Rodriguez HJ, Domenici R, Diroll A, Goykhman I. Assessment of dry weight by monitoring changes in blood volume during hemodialysis using Crit-Line. Kidney Int. 2005;68(2):854–61.
Steuer RR, Germain MJ, Leypoldt JK, Cheung AK. Enhanced fluid removal guided by blood volume monitoring during chronic hemodialysis. Artif Organs. 1998;22(8):627–32.
Dasselaar JJ, Huisman RM, de Jong PE, Burgerhof JG, Franssen CF. Effects of relative blood volume-controlled hemodialysis on blood pressure and volume status in hypertensive patients. ASAIO J. 2007;53(3):357–64.
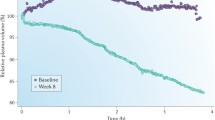
Sinha AD, Light RP, Agarwal R. Relative plasma volume monitoring during hemodialysis AIDS the assessment of dry weight. Hypertension. 2010;55(2):305–11.
Reddan DN, Szczech LA, Hasselblad V, Lowrie EG, Lindsay RM, Himmelfarb J, et al. Intradialytic blood volume monitoring in ambulatory hemodialysis patients: a randomized trial. J Am Soc Nephrol. 2005;16(7):2162–9.
Georgianos PI, Agarwal R. Epidemiology, diagnosis and management of hypertension among patients on chronic dialysis. Nat Rev Nephrol. 2016;12(10):636–47.
Jain SR, Smith L, Brewer ED, Goldstein SL. Non-invasive intravascular monitoring in the pediatric hemodialysis population. Pediatr Nephrol. 2001;16(1):15–8.
Michael M, Brewer ED, Goldstein SL. Blood volume monitoring to achieve target weight in pediatric hemodialysis patients. Pediatr Nephrol. 2004;19(4):432–7.
• Patel HP, Goldstein SL, Mahan JD, et al. A standard, noninvasive monitoring of hematocrit algorithm improves blood pressure control in pediatric hemodialysis patients. Clin J Am Soc Nephrol. 2007;2(2):252–7. Demonstrated that the use of non-invasive blood volume monitoring in children resulted in improved blood pressure control, decreased antihypertensives, and reduced intra-dialytic symptoms.
Candan C, Sever L, Civilibal M, Caliskan S, Arisoy N. Blood volume monitoring to adjust dry weight in hypertensive pediatric hemodialysis patients. Pediatr Nephrol. 2009;24(3):581–7.
Alexiadis G, Panagoutsos S, Roumeliotis S, Stibiris I, Markos A, Kantartzi K, et al. Comparison of multiple fluid status assessment methods in patients on chronic hemodialysis. Int Urol Nephrol. 2017;49(3):525–32.
Ronco C, Kaushik M, Valle R, Aspromonte N, Peacock WF. Diagnosis and management of fluid overload in heart failure and cardio-renal syndrome: the “5B” approach. Semin Nephrol. 2012;32(1):129–41.
Dahl LK. Salt and hypertension. Am J Clin Nutr. 1972;25(2):231–44.
Oliver WJ, Cohen EL, Neel JV. Blood pressure, sodium intake, and sodium related hormones in the Yanomamo Indians, a “no-salt” culture. Circulation. 1975;52(1):146–51.
SCRIBNER BH, BURI R, CANER JE, HEGSTROM R, BURNELL JM. The treatment of chronic uremia by means of intermittent hemodialysis: a preliminary report. Trans Am Soc Artif Intern Organs. 1960;6:114–22.
Kooman JP, van der Sande F, Leunissen K, Locatelli F. Sodium balance in hemodialysis therapy. Semin Dial. 2003;16(5):351–5.
Kayikcioglu M, Tumuklu M, Ozkahya M, et al. The benefit of salt restriction in the treatment of end-stage renal disease by haemodialysis. Nephrol Dial Transplant. 2009;24(3):956–62.
Mc Causland FR, Waikar SS, Brunelli SM. Increased dietary sodium is independently associated with greater mortality among prevalent hemodialysis patients. Kidney Int. 2012;82(2):204–11.
Maduell F, Navarro V. Dietary salt intake and blood pressure control in haemodialysis patients. Nephrol Dial Transplant. 2000;15(12):2063.
(K/DOQI) KDOQI. K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004;43(5 Suppl 1):S1–290.
Hui WF, Betoko A, Savant JD, Abraham AG, Greenbaum LA, Warady B, et al. Assessment of dietary intake of children with chronic kidney disease. Pediatr Nephrol. 2017;32(3):485–94.
Quader ZS, Gillespie C, Sliwa SA, et al. Sodium intake among US school-aged children: National Health and Nutrition Examination Survey, 2011–2012. J Acad Nutr Diet. 2017;117(1):39–47.e35.
Harnack LJ, Cogswell ME, Shikany JM, Gardner CD, Gillespie C, Loria CM, et al. Sources of sodium in US adults from 3 geographic regions. Circulation. 2017;135(19):1775–83.
Munoz Mendoza J, Arramreddy R, Schiller B. Dialysate sodium: choosing the optimal hemodialysis bath. Am J Kidney Dis. 2015;66(4):710–20.
Kramer H, Yee J, Weiner DE, Bansal V, Choi MJ, Brereton L, et al. Ultrafiltration rate thresholds in maintenance hemodialysis: an NKF-KDOQI controversies report. Am J Kidney Dis. 2016;68(4):522–32.
• Lowrie EG, Laird NM, Parker TF, Sargent JA. Effect of the hemodialysis prescription of patient morbidity: report from the National Cooperative Dialysis Study. N Engl J Med. 1981;305(20):1176–81. First randomized control trial in dialysis that studied if time or time-averaged urea concentration was more important to reduce morbidity and mortality. Led to the creation of Kt/V to measure clearance, and a shift toward shorter time on dialysis.
Sadowski RH, Allred EN, Jabs K. Sodium modeling ameliorates intradialytic and interdialytic symptoms in young hemodialysis patients. J Am Soc Nephrol. 1993;4(5):1192–8.
Song JH, Lee SW, Suh CK, Kim MJ. Time-averaged concentration of dialysate sodium relates with sodium load and interdialytic weight gain during sodium-profiling hemodialysis. Am J Kidney Dis. 2002;40(2):291–301.
Song JH, Park GH, Lee SY, Lee SW, Kim MJ. Effect of sodium balance and the combination of ultrafiltration profile during sodium profiling hemodialysis on the maintenance of the quality of dialysis and sodium and fluid balances. J Am Soc Nephrol. 2005;16(1):237–46.
Thein H, Haloob I, Marshall MR. Associations of a facility level decrease in dialysate sodium concentration with blood pressure and interdialytic weight gain. Nephrol Dial Transplant. 2007;22(9):2630–9.
Marsenic O, Anderson M, Couloures KG, Hong WS, Kevin Hall E, Dahl N. Effect of the decrease in dialysate sodium in pediatric patients on chronic hemodialysis. Hemodial Int. 2016;20(2):277–85.
Basile C, Pisano A, Lisi P, Rossi L, Lomonte C, Bolignano D. High versus low dialysate sodium concentration in chronic haemodialysis patients: a systematic review of 23 studies. Nephrol Dial Transplant. 2016;31(4):548–63.
Hecking M, Karaboyas A, Saran R, Sen A, Hörl WH, Pisoni RL, et al. Predialysis serum sodium level, dialysate sodium, and mortality in maintenance hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2012;59(2):238–48.
Hecking M, Karaboyas A, Saran R, Sen A, Inaba M, Rayner H, et al. Dialysate sodium concentration and the association with interdialytic weight gain, hospitalization, and mortality. Clin J Am Soc Nephrol. 2012;7(1):92–100.
Tattersall J, Martin-Malo A, Pedrini L, et al. EBPG guideline on dialysis strategies. Nephrol Dial Transplant. 2007;22(Suppl 2):ii5–21.
Foley RN, Gilbertson DT, Murray T, Collins AJ. Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med. 2011;365(12):1099–107.
Tandon T, Sinha AD, Agarwal R. Shorter delivered dialysis times associate with a higher and more difficult to treat blood pressure. Nephrol Dial Transplant. 2013;28(6):1562–8.
Brunet P, Saingra Y, Leonetti F, Vacher-Coponat H, Ramananarivo P, Berland Y. Tolerance of haemodialysis: a randomized cross-over trial of 5-h versus 4-h treatment time. Nephrol Dial Transplant. 1996;11(Suppl 8):46–51.
• Chertow GM, Levin NW, Beck GJ, et al. In-center hemodialysis six times per week versus three times per week. N Engl J Med. 2010;363(24):2287–300. Demonstrated decreased morbidity in patients that received more frequent dialysis.
Georgianos PI, Sarafidis PA, Sinha AD, Agarwal R. Adverse effects of conventional thrice-weekly hemodialysis: is it time to avoid 3-day interdialytic intervals? Am J Nephrol. 2015;41(4–5):400–8.
Ok E, Duman S, Asci G, Tumuklu M, Onen Sertoz O, Kayikcioglu M, et al. Comparison of 4- and 8-h dialysis sessions in thrice-weekly in-centre haemodialysis: a prospective, case-controlled study. Nephrol Dial Transplant. 2011;26(4):1287–96.
Fischbach M, Terzic J, Laugel V, Escande B, Dangelser C, Helmstetter A. Measurement of hydrostatic intraperitoneal pressure: a useful tool for the improvement of dialysis dose prescription. Pediatr Nephrol. 2003;18(10):976–80.
Goldstein SL, Silverstein DM, Leung JC, Feig DI, Soletsky B, Knight C, et al. Frequent hemodialysis with NxStage system in pediatric patients receiving maintenance hemodialysis. Pediatr Nephrol. 2008;23(1):129–35.
Hoppe A, von Puttkamer C, Linke U, et al. A hospital-based intermittent nocturnal hemodialysis program for children and adolescents. J Pediatr. 2011;158(1):95–9. 99.e91
Thumfart J, Puttkamer CV, Wagner S, Querfeld U, Müller D. Hemodiafiltration in a pediatric nocturnal dialysis program. Pediatr Nephrol. 2014;29(8):1411–6.
Thumfart J, Hilliger T, Stiny C, Wagner S, Querfeld U, Müller D. Is peritoneal dialysis still an equal option? Results of the Berlin pediatric nocturnal dialysis program. Pediatr Nephrol. 2015;30(7):1181–7.
McIntyre CW. Effects of hemodialysis on cardiac function. Kidney Int. 2009;76(4):371–5.
Movilli E, Gaggia P, Zubani R, Camerini C, Vizzardi V, Parrinello G, et al. Association between high ultrafiltration rates and mortality in uraemic patients on regular haemodialysis. A 5-year prospective observational multicentre study. Nephrol Dial Transplant. 2007;22(12):3547–52.
Movilli E, Camerini C, Gaggia P, Zubani R, Feller P, Poiatti P, et al. Magnitude of end-dialysis overweight is associated with all-cause and cardiovascular mortality: a 3-year prospective study. Am J Nephrol. 2013;37(4):370–7.
• Saran R, Bragg-Gresham JL, Levin NW, Twardowski ZJ, Wizemann V, Saito A, et al. Longer treatment time and slower ultrafiltration in hemodialysis: associations with reduced mortality in the DOPPS. Kidney Int. 2006;69(7):1222–8. International study demonstrated the risk of aggressive ultrafiltration.
• Hothi DK, Rees L, Marek J, Burton J, McIntyre CW. Pediatric myocardial stunning underscores the cardiac toxicity of conventional hemodialysis treatments. Clin J Am Soc Nephrol. 2009;4(4):790–7. Described that myocardial stunning occurs in the pediatric population as well.
Rippe B. A three-pore model of peritoneal transport. Perit Dial Int. 1993;13(Suppl 2):S35–8.
Fischbach M, Schmitt CP, Shroff R, Zaloszyc A, Warady BA. Increasing sodium removal on peritoneal dialysis: applying dialysis mechanics to the peritoneal dialysis prescription. Kidney Int. 2016;89(4):761–6.
Erixon M, Wieslander A, Lindén T, Carlsson O, Forsbäck G, Svensson E, et al. How to avoid glucose degradation products in peritoneal dialysis fluids. Perit Dial Int. 2006;26(4):490–7.
Frampton JE, Plosker GL. Icodextrin: a review of its use in peritoneal dialysis. Drugs. 2003;63(19):2079–105.
Rousso S, Banh TM, Ackerman S, Piva E, Licht C, Harvey EA. Impact of fill volume on ultrafiltration with icodextrin in children on chronic peritoneal dialysis. Pediatr Nephrol. 2016;31(10):1673–9.
Collins A, Mujais S. Advancing fluid management in peritoneal dialysis. Kidney Int Suppl. 2002;81:S1–2.
Mujais S, Vonesh E. Profiling of peritoneal ultrafiltration. Kidney Int Suppl. 2002;62(81):S17–22.
Fischbach M, Desprez P, Donnars F, Hamel G, Geisert J. Optimization of CCPD prescription in children using peritoneal equilibration test. Adv Perit Dial. 1994;10:307–9.
Fischbach M, Issad B, Dubois V, Taamma R. The beneficial influence on the effectiveness of automated peritoneal dialysis of varying the dwell time (short/long) and fill volume (small/large): a randomized controlled trial. Perit Dial Int. 2011;31(4):450–8.
Hayashi SY, Seeberger A, Lind B, et al. Acute effects of low and high intravenous doses of furosemide on myocardial function in anuric haemodialysis patients: a tissue Doppler study. Nephrol Dial Transplant. 2008;23(4):1355–61.
Lemes HP, Araujo S, Nascimento D, Cunha D, Garcia C, Queiroz V, et al. Use of small doses of furosemide in chronic kidney disease patients with residual renal function undergoing hemodialysis. Clin Exp Nephrol. 2011;15(4):554–9.
Weidmann P, Maxwell MH, Lupu AN, Lewin AJ, Massry SG. Plasma renin activity and blood pressure in terminal renal failure. N Engl J Med. 1971;285(14):757–62.
Van Buren PN, Inrig JK. Hypertension and hemodialysis: pathophysiology and outcomes in adult and pediatric populations. Pediatr Nephrol. 2012;27(3):339–50.
Simões e Silva AC, Diniz JS, Pereira RM, Pinheiro SV, Santos RA. Circulating renin angiotensin system in childhood chronic renal failure: marked increase of angiotensin-(1-7) in end-stage renal disease. Pediatr Res. 2006;60(6):734–9.
Converse RL, Jacobsen TN, Toto RD, et al. Sympathetic overactivity in patients with chronic renal failure. N Engl J Med. 1992;327(27):1912–8.
Hausberg M, Kosch M, Harmelink P, Barenbrock M, Hohage H, Kisters K, et al. Sympathetic nerve activity in end-stage renal disease. Circulation. 2002;106(15):1974–9.
Rauh W, Hund E, Sohl G, Rascher W, Mehls O, Schärer K. Vasoactive hormones in children with chronic renal failure. Kidney Int Suppl. 1983;15:S27–33.
Liu M, Takahashi H, Morita Y, et al. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrol Dial Transplant. 2003;18(3):563–9.
Zilch O, Vos PF, Oey PL, Cramer MJM, Ligtenberg G, Koomans HA, et al. Sympathetic hyperactivity in haemodialysis patients is reduced by short daily haemodialysis. J Hypertens. 2007;25(6):1285–9.
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999;99(18):2434–9.
Gbadegesin R, Kudelka T, Gadegbeku CA, Brophy P, Smoyer WE, Lin JJ. Arterial compliance in adolescents and young adults receiving chronic hemodialysis. Ren Fail. 2008;30(6):591–6.
Brandt JR, Avner ED, Hickman RO, Watkins SL. Safety and efficacy of erythropoietin in children with chronic renal failure. Pediatr Nephrol. 1999;13(2):143–7.
Shichiri M, Hirata Y, Ando K, Emori T, Ohta K, Kimoto S, et al. Plasma endothelin levels in hypertension and chronic renal failure. Hypertension. 1990;15(5):493–6.
Xu J, Li G, Wang P, Velazquez H, Yao X, Li Y, et al. Renalase is a novel, soluble monoamine oxidase that regulates cardiac function and blood pressure. J Clin Invest. 2005;115(5):1275–80.
Agarwal R, Weir MR. Dry-weight: a concept revisited in an effort to avoid medication-directed approaches for blood pressure control in hemodialysis patients. Clin J Am Soc Nephrol. 2010;5(7):1255–60.
Flynn JT, Mitsnefes M, Pierce C, Cole SR, Parekh RS, Furth SL, et al. Blood pressure in children with chronic kidney disease: a report from the Chronic Kidney Disease in Children study. Hypertension. 2008;52(4):631–7.
Kupferman JC, Aronson Friedman L, Cox C, Flynn J, Furth S, Warady B, et al. BP control and left ventricular hypertrophy regression in children with CKD. J Am Soc Nephrol. 2014;25(1):167–74.
Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG. Hypertension in hemodialysis patients treated with atenolol or lisinopril: a randomized controlled trial. Nephrol Dial Transplant. 2014;29(3):672–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Hypertension
Rights and permissions
About this article
Cite this article
Munshi, R., Flynn, J.T. Hypertension in Pediatric Dialysis Patients: Etiology, Evaluation, and Management. Curr Hypertens Rep 20, 61 (2018). https://doi.org/10.1007/s11906-018-0857-z
Published:
DOI: https://doi.org/10.1007/s11906-018-0857-z