Abstract
Purpose of Review
Patients after intracerebral hemorrhage (ICH) are at high risk of both ischemic stroke and recurrent ICH, and stroke prevention after ICH is important to improve the long-term outcomes in this patient population. The objective of this article is to review the current guidelines on stroke prevention measures after ICH as well as the new findings and controversies for future guidance.
Recent Findings
Intensive blood pressure reduction might benefit ICH survivors significantly. Cholesterol levels and the risk of ICH have an inverse relationship, but statin therapy after ICH might be still beneficial. Anticoagulation in atrial fibrillation after ICH specifically with novel oral anticoagulants may be associated with better long-term outcomes. Left atrial appendage occlusion may be an alternative for stroke prevention in ICH survivors with atrial fibrillation for whom long-term anticoagulation therapy is contraindicated.
Summary
While complete individualized risk assessment is imperative to prevent stroke after ICH, future research is required to address current controversies and knowledge gap in this topic.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fewel, Matthew E, Thompson Jr, B Gegory, Hoff JT. Spontaneous intracerebral hemorrhage: a review. J. Neurosurg. 2003;15:
Flaherty ML, Haverbusch M, Sekar P, et al. Long-term mortality after intracerebral hemorrhage From the Departments of Neurology. 2006 Apr 25;66(8):1182-6.
Hansen BM, Nilsson OG, Anderson H, Norrving B, Säveland H, Lindgren A. Long term (13 years) prognosis after primary intracerebral haemorrhage: a prospective population based study of long term mortality, prognostic factors and causes of death. J Neurol Neurosurg Psychiatry. 2013;84:1150–5.
Virani SS, Alonso A, Aparicio HJ, et al. Heart Disease and Stroke Statistics-2021 update: a report From the American Heart Association. Circulation 2021; https://www.ahajournals.org/doi/10.1161/CIR.0000000000000950
Murthy SB, Diaz I, Wu X, Merkler AE, Iadecola C, Safford MM, Sheth KN, Navi BB, Kamel H. Risk of arterial ischemic events after intracerebral hemorrhage. Stroke. 2020;51:137–42.
van Nieuwenhuizen KM, Vaartjes I, Verhoeven JI, Rinkel GJ, Kappelle LJ, Schreuder FH, Klijn CJ. Long-term prognosis after intracerebral haemorrhage. Eur stroke J. 2020;5:336–44.
Buhl R, Barth H, Mehdorn HM. Risk of recurrent intracerebral hemorrhages. Neurol Res. 2003;25:853–6.
O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet (London, England). 2016;388:761–75.
Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke. 2015;46:2032–60.
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9:689–701.
Bailey RD, Hart RG, Benavente O, Pearce LA. Recurrent brain hemorrhage is more frequent than ischemic stroke after intracranial hemorrhage. Neurology. 2001;56:773–7.
Viswanathan A, Rakich SM, Engel C, Snider R, Rosand J, Greenberg SM, Smith EE. Antiplatelet use after intracerebral hemorrhage. Neurology. 2006;66:206–9.
Li L, Luengo-Fernandez R, Zuurbier SM, Beddows NC, Lavallee P, Silver LE, Kuker W, Rothwell PM. Ten-year risks of recurrent stroke, disability, dementia and cost in relation to site of primary intracerebral haemorrhage: population-based study. J Neurol Neurosurg Psychiatry. 2020;91:580–5.
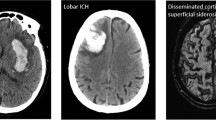
Charidimou A, Imaizumi T, Moulin S, et al. Brain hemorrhage recurrence, small vessel disease type, and cerebral microbleeds a meta-analysis. 2017; https://doi.org/10.1212/WNL.0000000000004259
Viswanathan A, Chabriat H. Cerebral microhemorrhage. Stroke. 2006;37:550–5.
Roob G, Lechner A, Schmidt R, Flooh E, Hartung H-P, Fazekas F. Frequency and location of microbleeds in patients with primary intracerebral hemorrhage. Stroke. 2000;31:2665–9.
Biffi A, Sonni A, Anderson CD, et al. Variants at APOE influence risk of deep and lobar intracerebral hemorrhage. Ann Neurol. 2010;68:934–43.
Misra UK, Kalita J, Somarajan BI. Recurrent intracerebral hemorrhage in patients with hypertension is associated with APOE gene polymorphism: a preliminary study. J Stroke Cerebrovasc Dis. 2013;22:758–63.
Carpenter AM, Singh IP, Gandhi CD, Prestigiacomo CJ. Genetic risk factors for spontaneous intracerebral haemorrhage. Nat Rev Neurol. 2016;12:40–9.
Rannikmäe K, Samarasekera N, Martînez-Gonzâlez NA, Al-Shahi Salman R, Sudlow CLM. Genetics of cerebral amyloid angiopathy: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2013;84:901–8.
Marini S, Crawford K, Morotti A, et al. Association of apolipoprotein E with intracerebral hemorrhage risk by race/ethnicity. JAMA Neurol. 2019;76:480.
Nie H, Hu Y, Liu N, et al. Apolipoprotein E gene polymorphisms are risk factors for spontaneous intracerebral hemorrhage: a systematic review and meta-analysis. Curr Med Sci. 2019;39:111–7.
Woo D, Falcone GJ, Devan WJ, et al. Meta-analysis of genome-wide association studies identifies 1q22 as a susceptibility locus for intracerebral hemorrhage. Am J Hum Genet. 2014;94:511–21.
Malik R, Chauhan G, Traylor M, et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 2018;50:524–37.
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet (London, England). 2001;358:1033–41.
SPS3 Study Group TS, Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, Pearce LA, Pergola PE, Szychowski JM. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet (London, England). 2013;382:507–15.
Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke. 2014;45:2160–236.
Arima H, Chalmers J, Woodward M, Anderson C, Rodgers A, Davis S, Macmahon S, Neal B. PROGRESS Collaborative Group. Lower target blood pressures are safe and effective for the prevention of recurrent stroke: the PROGRESS trial. J Hypertens. 2006;24:1201–8.
Ovbiagele B, Diener H-C, Yusuf S, Martin RH, Cotton D, Vinisko R, Donnan GA, Bath PM. Investigators PROFESS. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA. 2011;306:2137–44.
Group TSR. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018. https://doi.org/10.1161/HYP.0000000000000065.
Fei Y, Tsoi M-F, Cheung BMY. Determining the optimal systolic blood pressure for hypertensive patients: a network meta-analysis. Can J Cardiol. 2018;34:1581–9.
Bangalore S, Toklu B, Gianos E, Schwartzbard A, Weintraub H, Ogedegbe G, Messerli FH. Optimal systolic blood pressure target after SPRINT: insights from a network meta-analysis of randomized trials. Am J Med. 2017;130:707-719.e8.
Jolink WMT, Wiegertjes K, Rinkel GJE, Algra A, de Leeuw F-E, Klijn CJM. Location-specific risk factors for intracerebral hemorrhage: Systematic review and meta-analysis. Neurology. 2020;95:e1807–18.
Biffi A, Anderson CD, Battey K, Ayres TW, Greenberg AM, Viswanathan SM, Rosand A, Philip JJ. Association Between blood pressure control and risk of recurrent intracerebral hemorrhage HHS Public Access. JAMA. 2015;314:904-912
Arima H, Tzourio C, Anderson C, Woodward M, Bousser M-G, MacMahon S, Neal B, Chalmers J. Effects of perindopril-based lowering of blood pressure on intracerebral hemorrhage related to amyloid angiopathy. Stroke. 2010;41:394–6.
• Grundy SM, Stone NJ, Bailey AL, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019 Jun 25;73(24):3168-3209. https://doi.org/10.1016/j.jacc.2018.11.002. Epub 2018 Nov 10. This article provides the most updated and extensive evidencebased guidelines on the management of blood cholesterol.
TSP Investigators by AR in CL (SPARCL) High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549-559.
Goldstein LB, Amarenco P, Szarek M, Callahan A, Hennerici M, Sillesen H, Zivin JA, Welch KMA, Investigators SPARCL. Hemorrhagic stroke in the Stroke Prevention by Aggressive Reduction in Cholesterol Levels study. Neurology. 2008;70:2364–70.
Wang X, Dong Y, Qi X, Huang C, Hou L. Cholesterol levels and risk of hemorrhagic stroke: a systematic review and meta-analysis. Stroke. 2013;44:1833–9.
Cholesterol Treatment Trialists’ (CTT) Collaboration B, Baigent C, Blackwell L, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials Lancet. (London, England) 2010;376:1670-1681.
Hackam DG, Woodward M, Newby LK, et al. Statins and intracerebral hemorrhage: collaborative systematic review and meta-analysis. Circulation. 2011;124:2233–42.
McKinney JS, Kostis WJ. Statin therapy and the risk of intracerebral hemorrhage: a meta-analysis of 31 randomized controlled trials. Stroke. 2012;43:2149–56.
Pezzini A, Grassi M, Iacoviello L, et al. Serum cholesterol levels, HMG-CoA reductase inhibitors and the risk of intracerebral haemorrhage. The Multicenter Study on Cerebral Haemorrhage in Italy (MUCH-Italy). J Neurol Neurosurg Psychiatry. 2016;87:924–9.
Sun L, Clarke R, Bennett D, et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat Med. 2019;25:569–74.
Falcone GJ, Kirsch E, Acosta JN, et al. Genetically elevated LDL associates with lower risk of intracerebral hemorrhage. Ann Neurol. 2020;88:56–66.
Åsberg S, Eriksson M. Statin therapy and the risk of intracerebral haemorrhage: a nationwide observational study. Int J Stroke. 10 Suppl A. 2015;100:46–9.
Saliba W, Rennert HS, Barnett-Griness O, Gronich N, Molad J, Rennert G, Auriel E. Association of statin use with spontaneous intracerebral hemorrhage: a cohort study. Neurology. 2018;91:e400–9.
Chung C-M, Lin M-S, Liu C-H, Lee T-H, Chang S-T, Yang T-Y, Pan K-L, Lin Y-S. Discontinuing or continuing statin following intracerebral hemorrhage from the view of a national cohort study. Atherosclerosis. 2018;278:15–22.
Lin M-S, Lin Y-S, Chang S-T, Wang P-C, Chien-Chia WuV, Lin W-Y, Chung C-M. Effect of initiating statin therapy on long-term outcomes of patients with dyslipidemia after intracerebral hemorrhage. Atherosclerosis. 2019;288:137–45.
Flint AC, Conell C, Rao VA, Klingman JG, Sidney S, Johnston SC, Hemphill JC, Kamel H, Davis SM, Donnan GA. Effect of statin use during hospitalization for intracerebral hemorrhage on mortality and discharge disposition. JAMA Neurol. 2014;71:1364–71.
Jung J-M, Choi J-Y, Kim HJ, Seo W-K . Statin use in spontaneous intracerebral hemorrhage: a systematic review and meta-analysis. Int J Stroke. 10 Suppl A 2015;1002015:10–7
Cheng Y, Qiao L, Jiang Z, Dong X, Feng H, Gui Q, Lu Y, Liang Y. Significant reduction in the LDL cholesterol increases the risk of intracerebral hemorrhage: a systematic review and meta-analysis of 33 randomized controlled trials. Am J Transl Res. 2020;12:463–77.
Tai S-Y, Lin F-C, Lee C-Y, Chang C-J, Wu M-T, Chien C-Y. Statin use after intracerebral hemorrhage: a 10-year nationwide cohort study. Brain Behav. 2016;6:e00487
Ma C, Gurol ME, Huang Z, Lichtenstein AH, Wang X, Wang Y, Neumann S, Wu S, Gao X. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: a prospective study. Neurology. 2019;93:e445–57.
Rist PM, Buring JE, Ridker PM, Kase CS, Kurth T, Rexrode KM. Lipid levels and the risk of hemorrhagic stroke among women. Neurology. 2019;92:e2286–94.
Amarenco P, Kim JS, Labreuche J, et al. A comparison of two LDL cholesterol targets after ischemic stroke. N Engl J Med. 2020;382:9–19.
Haussen DC, Henninger N, Kumar S, Selim M. Statin use and microbleeds in patients with spontaneous intracerebral hemorrhage. Stroke. 2012;43:2677–81.
Woo D, Deka R, Falcone GJ, et al. Apolipoprotein E, statins, and risk of intracerebral hemorrhage. Stroke. 2013;44:3013–7.
Saliba W, Molad J, Auriel E. Author response: Association of statin use with spontaneous intracerebral hemorrhage: a cohort study. Neurology. 2019;92:823.
Sharma R, Matsushita K, Wu A, Jack CR, Griswold M, Mosley TH, Fornage M, Gottesman RF Common medications and intracerebral hemorrhage: the ARIC Study. J Am Heart Assoc. 2021;e014270
Feinberg WM. Anticoagulation for prevention of stroke. Neurology. 1998;51:S20–2.
• Lip GYH, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation: CHEST Guideline and Expert Panel Report. Chest. 2018;154:1121–201. This article provides guidelines on the management of atrial fibrillation that cover a broad range of relevant topics.
Vermeer SE, Algra A, Franke CL, Koudstaal PJ, Rinkel GJE. Long-term prognosis after recovery from primary intracerebral hemorrhage. Neurology. 2002;59:205–9.
Flynn RWV, MacDonald TM, Murray GD, MacWalter RS, Doney ASF. Prescribing antiplatelet medicine and subsequent events after intracerebral hemorrhage. Stroke. 2010;41:2606–11.
C-J Chen D Ding TJ Buell FD Testai S Koch D Woo BB Worrall ERICH Investigators for the E. Restarting antiplatelet therapy after spontaneous intracerebral hemorrhage: functional outcomes Neurology. 2018;91:e26-e36.
Murthy SB, Biffi A, Falcone GJ, et al. Antiplatelet therapy after spontaneous intracerebral hemorrhage and functional outcomes. Stroke. 2019;50:3057–63.
• Al-Shahi Salman R, Dennis M, Sandercock P, et al. Effects of antiplatelet therapy after stroke due to intracerebral haemorrhage (RESTART): a randomised, open-label trial. Lancet. 2019;393:2613–23. This is the first RCT on the outcome of antiplatelet use in patients with history of ICH.
Ottosen TP, Grijota M, Hansen ML, Brandes A, Damgaard D, Husted SE, Johnsen SP. Use of antithrombotic therapy and long-term clinical outcome among patients surviving intracerebral hemorrhage. Stroke. 2016;47:1837–43.
Korompoki E, Filippidis FT, Nielsen PB, et al. Long-term antithrombotic treatment in intracranial hemorrhage survivors with atrial fibrillation. Neurology. 2017;89:687–96.
Biffi A, Kuramatsu JB, Leasure A, et al. Oral anticoagulation and functional outcome after intracerebral hemorrhage. Ann Neurol. 2017;82:755–65.
Murthy SB, Gupta A, Merkler AE, Navi BB, Mandava P, Iadecola C, Sheth KN, Hanley DF, Ziai WC, Kamel H. Restarting anticoagulant therapy after intracranial hemorrhage: a systematic review and meta-analysis. Stroke. 2017;48:1594–600.
Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–62.
Tsivgoulis G, Lioutas V-A, Varelas P, et al. Direct oral anticoagulant- vs vitamin K antagonist-related nontraumatic intracerebral hemorrhage. Neurology. 2017;89:1142–51.
•• January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019;140:e125–51. This article provides the most updated evidence-based guidelines on the management of atrial fibrillation.
Eckman MHc patients be anticoagulated after intracerebral hemorrhage? A decision analysis., Rosand J, Knudsen KA, Singer DE, Greenberg SM. Can patients be anticoagulated after intracerebral hemorrhage? A decision analysis Stroke 2003;34:1710-1716
Park Y-A, Joung B. Reply to the Editor— Anticoagulation in atrial fibrillation after intracranial hemorrhage: could the hemorrhage location influence the outcome? Hear Rhythm 2017;14:e46
Lip GYH, Laroche C, Dan G-A, et al. “Real-world” antithrombotic treatment in atrial fibrillation: the EORP-AF pilot survey. Am J Med. 2014;127:519-29.e1.
Flaker GC, Eikelboom JW, Shestakovska O, Connolly SJ, Kaatz S, Budaj A, Husted S, Yusuf S, Lip GYH, Hart RG. Bleeding during treatment with aspirin versus apixaban in patients with atrial fibrillation unsuitable for warfarin: the apixaban versus acetylsalicylic acid to prevent stroke in atrial fibrillation patients who have failed or are unsuitable for vitamin K antagonist treatment (AVERROES) trial. Stroke. 2012;43:3291–7.
Pennlert J, Overholser R, Asplund K, Carlberg B, Van Rompaye B, Wiklund PG, Eriksson M. Optimal timing of anticoagulant treatment after intracerebral hemorrhage in patients with atrial fibrillation. Stroke. 2017;48:314–20.
Park Y-A, Uhm J-S, Pak H-N, Lee M-H, Joung B. Anticoagulation therapy in atrial fibrillation after intracranial hemorrhage. Hear Rhythm. 2016;13:1794–802.
Reddy VY, Sievert H, Halperin J, et al. Percutaneous left atrial appendage closure vs warfarin for atrial fibrillation. JAMA. 2014;312:1988.
Holmes DR, Kar S, Price MJ, Whisenant B, Sievert H, Doshi SK, Huber K, Reddy VY. Prospective randomized evaluation of the Watchman Left Atrial Appendage Closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014;64:1–12.
Brouwer TF, Whang W, Kuroki K, Halperin JL, Reddy VY. Net clinical benefit of left atrial appendage closure versus warfarin in patients with atrial fibrillation: a pooled analysis of the randomized PROTECT-AF and PREVAIL studies. J Am Heart Assoc 2019;8:e013525
Fauchier L, Cinaud A, Brigadeau F, et al. Device-related thrombosis after percutaneous left atrial appendage occlusion for atrial fibrillation. J Am Coll Cardiol. 2018;71:1528–36.
Boersma LV, Ince H, Kische S, et al. Evaluating real-world clinical outcomes in atrial fibrillation patients receiving the WATCHMAN left atrial appendage closure technology: final 2-year outcome data of the EWOLUTION Trial focusing on history of stroke and hemorrhage. Circ Arrhythm Electrophysiol 2019;12:e006841
• Osmancik P, Herman D, Neuzil P, et al. Left atrial appendage closure versus direct oral anticoagulants in high-risk patients with atrial fibrillation. J Am Coll Cardiol. 2020;75:3122–35. This is the first RCT which tested the efficacy and safety of LAA closure compared with NOACs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Baang has nothing to disclose.
Dr. Sheth reports grants from Biogen, Novartis, Bard, NIH, and AHA; and personal fees from NControl and Zoll; and non-financial support from Alva.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Stroke
Rights and permissions
About this article
Cite this article
Baang, H.Y., Sheth, K.N. Stroke Prevention After Intracerebral Hemorrhage: Where Are We Now?. Curr Cardiol Rep 23, 162 (2021). https://doi.org/10.1007/s11886-021-01594-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11886-021-01594-0