Abstract
Objective
Few studies have been carried out concerning the influence of bariatric surgery on female sexuality and hormones, particularly utilizing hormone-based questionnaires. The effect of bariatric surgery on sex hormone levels, sexual function and health-related quality of life (HRQL) in women was analyzed in this study. Participants were included in a single-center study at a regional hospital in Sweden, with a duration of one-year follow-up.
Methods
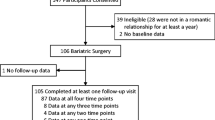
One hundred non-smoking women, undergoing laparoscopic Roux-en-Y gastric bypass, were included in the study. Blood assay for sex-hormone binding globulin (SHBG), testosterone, estrogen, progesterone, follicle-stimulating hormone (FSH) and luteinizing hormone (LH) was analyzed. Participants completed the Female Sexual Function Index (FSFI), Women’s Health Questionnaire (WHQ) and Psychological General Well-being Inventory (PGWB) parallel to lab testing.
Results
At one-year follow-up, several significant results were found concerning hormones and questionnaires. Testosterone decreased and SHBG increased, N = 68/100. Desire, arousal, orgasm, satisfaction and total score domains for the FSFI increased after one year, N = 53/100. WHQ domains concerning depressed mood, somatic symptoms, memory, anxiety, sexual behavior and attractiveness improved after one year, N = 47/100. All domains in the PGWB (N = 52), including anxiety, depressed mood, positive well-being, self-control, general health, vitality and total score improved at follow-up. Spearman’s Rho coefficient analysis found correlation between testosterone/WHQ-sexual problems (0.3), SHBG/WHQ-general health (0.3) and SHBG/FSFI-arousal (−0.3).
Conclusions
Bariatric surgery normalizes levels of sex-hormones in women, and results in improved sexual function, health-related quality of life and psychological well-being.
Similar content being viewed by others
References
Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404.
Tchernof A, Despres JP. Sex steroid hormones, sex hormone-binding globulin, and obesity in men and women. Horm Metab Res. 2000;32(11–12):526–36.
Gosman GG, King WC, Schrope B, et al. Reproductive health of women electing bariatric surgery. Fertil Steril. 2010;94(4):1426–31.
Sarwer DB, Spitzer JC, Wadden TA, et al. Changes in sexual functioning and sex hormone levels in women following bariatric surgery. JAMA Surg. 2014;149(1):26–33.
Kolotkin RL, Binks M, Crosby RD, et al. Obesity and sexual quality of life. Obesity (Silver Spring). 2006;14(3):472–9.
Sarwer DB, Lavery M, Spitzer JC. A review of the relationships between extreme obesity, quality of life, and sexual function. Obes Surg. 2012;22(4):668–76.
Esposito K, Ciotola M, Giugliano F, et al. Association of body weight with sexual function in women. Int J Impot Res. 2007;19(4):353–7.
Steffen KJ, King WC, White GE, et al. Sexual functioning of men and women with severe obesity before bariatric surgery. Surg Obes Relat Dis. 2017;13(2):334–43.
Malik SM, Traub ML. Defining the role of bariatric surgery in polycystic ovarian syndrome patients. World J Diabetes. 2012;3(4):71–9.
Tan O, Carr BR. The impact of bariatric surgery on obesity-related infertility and in vitro fertilization outcomes. Semin Reprod Med. 2012;30(6):517–28.
Bond DS, Wing RR, Vithiananthan S, et al. Significant resolution of female sexual dysfunction after bariatric surgery. Surg Obes Relat Dis. 2011;7:1):1–7.
Sarwer DB, Wadden TA, Spitzer JC, et al. 4-year changes in sex hormones, sexual functioning, and psychosocial status in women who underwent bariatric surgery. Obes Surg. 2018;28(4):892–9.
Meczekalski B, Katulski K, Czyzyk A, et al. Functional hypothalamic amenorrhea and its influence on women's health. J Endocrinol Investig. 2014;37(11):1049–56.
Pasquali R, Vicennati V, Gambineri A. Adrenal and gonadal function in obesity. J Endocrinol Investig. 2002;25(10):893–8.
Botwood N, Hamilton-Fairley D, Kiddy D, et al. Sex hormone-binding globulin and female reproductive function. J Steroid Biochem Mol Biol. 1995;53(1–6):529–31.
Boonchaya-Anant P, Laichuthai N, Suwannasrisuk P, et al. Changes in testosterone levels and sex hormone-binding globulin levels in extremely obese men after bariatric surgery. Int J Endocrinol. 2016;2016:1416503.
Rosen R, Brown C, Heiman J, et al. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208.
Wiklund I, Karlberg J, Lindgren R, et al. A Swedish version of the Women's health questionnaire. A measure of postmenopausal complaints. Acta Obstet Gynecol Scand. 1993;72(8):648–55.
Hunter M. The women's health questionnaire: a measure of mid-aged women's perceptions of their emotional and physical health. Psychol Health. 1992;7(1):45–54.
Dupuy HJ. The psychological general well-being (PGWB) index. New York: Le Jacq Publishing, Inc; 1984.
Kjaer MM, Madsbad S, Hougaard DM, et al. The impact of gastric bypass surgery on sex hormones and menstrual cycles in premenopausal women. Gynecol Endocrinol. 2017;33(2):160–3.
Ernst B, Wilms B, Thurnheer M, et al. Reduced circulating androgen levels after gastric bypass surgery in severely obese women. Obes Surg. 2013;23(5):602–7.
Wei S, Schmidt MD, Dwyer T, et al. Obesity and menstrual irregularity: associations with SHBG, testosterone, and insulin. Obesity (Silver Spring). 2009;17(5):1070–6.
Turkmen S, Ahangari A, Backstrom T. Roux-en-Y gastric bypass surgery in patients with polycystic ovary syndrome and metabolic syndrome. Obes Surg. 2016;26(1):111–8.
Steffen KJ, King WC, White GE, et al. Changes in sexual functioning in women and men in the 5 years after bariatric surgery. JAMA Surg. 2019;154:487–98.
Lynch A. "when the honeymoon is over, the real work begins:" gastric bypass patients' weight loss trajectories and dietary change experiences. Soc Sci Med (1982. 2016;151:241–9.
Biron S, Biertho L, Marceau S, et al. Long-term follow-up of disease-specific quality of life after bariatric surgery. Surg Obes Relat Dis. 2018;14(5):658–64.
Mazer LM, Azagury DE, Morton JM. Quality of life after bariatric surgery. Curr Obes Rep. 2017;6(2):204–10.
Kolotkin RL, Davidson LE, Crosby RD, et al. Six-year changes in health-related quality of life in gastric bypass patients versus obese comparison groups. Surg Obes Relat Dis. 2012;8(5):625–33.
Heiman JR, Rupp H, Janssen E, et al. Sexual desire, sexual arousal and hormonal differences in premenopausal US and Dutch women with and without low sexual desire. Horm Behav. 2011;59(5):772–9.
Cappelletti M, Wallen K. Increasing women's sexual desire: the comparative effectiveness of estrogens and androgens. Horm Behav. 2016;78:178–93.
Chidi-Ogbolu N, Baar K. Effect of estrogen on musculoskeletal performance and injury risk. Front Physiol. 2018;9:1834.
Acknowledgements
We would like to extend our deep appreciation to Annelie Villaume, R.N. and Annika Kaiser R.N., for carrying out administration duties. And our gratitude to Mats Fredriksson for assistance in statistical analysis.
Funding
This work was supported by a grant from Linkoping Medical Faculty Grant Board (LIO-309361), and grants from Region Ostergotland (LIO-421541, LIO-601561, LIO-507021, LIO-342321).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and /or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent Statement
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Paul, R., Andersson, E., Wirén, M. et al. Health-Related Quality of Life, Sexuality and Hormone Status after Laparoscopic Roux-En-Y Gastric Bypass in Women. OBES SURG 30, 493–500 (2020). https://doi.org/10.1007/s11695-019-04197-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04197-5