Abstract
Background
Treatment of parasitic infections with conventional drugs is associated with high toxicity, and undesirable side effects require cogent substitutions. Nanotechnology has provided novel approaches to synthesize nano-drugs to improve efficient antipathetic treatment.
Purpose
Nano-chitosan as a nontoxic antimicrobial agent was examined against three most prevalent protozoa in humans, Plasmodium falciparum, Giardia lamblia and Trichomonas vaginalis.
Methods
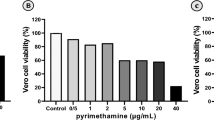
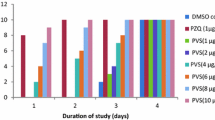
Chitosan extracted from Penicillium fungi was converted to nanoparticles to maximize its therapeutic properties. Safety of nano-chitosan was examined by determining its hemolytic property and toxicity on PC12 cells. The studied parasites were identified with RFLP-PCR and cultivation in relevant media. Characteristics of nano-chitosan as an useful and valuable curative compound was evaluated by FTIR, DLS and SEM. Dose dependent anti-parasitic effect of nano-chitosan was evaluated.
Results
The highest anti-parasitic activity of the nano-chitosan was observed at 50 μg/mL by which growth rates of cultivated P. falciparum, T. vaginalis and G. lamblia were inhibited by 59.5%, 99.4%, and 31.3%, respectively. The study demonstrated that nano-chitosan with the least toxicity, low side effects, and substantial efficacy deserved to be considered as an anti-parasitic nano-compound.
Conclusion
Nano-chitosan significantly inhibited protozoan growth in vitro promising to explore its use to combat parasitic infections. Further investigations covering extended sample size, in vivo experiments and optimizing the concentration used may lead to efficient treatment of protozoan diseases.
Graphic abstract









Similar content being viewed by others
References
Forson AO, Arthur I, Ayeh-Kumi PF (2018) The role of family size, employment and education of parents in the prevalence of intestinal parasitic infections in school children in Accra. PLoS ONE 13(2):0192303. https://doi.org/10.1371/journal.pone.0192303
Abbaszadeh MJ, Barkhori M, Rezaeian M, Mohebali M, Baigi V, Amiri S, Amirshekari MB et al (2020) Prevalence and associated risk factors of human intestinal parasitic infections: a population-based study in the southeast of Kerman province, southeastern Iran. BMC Infect Dis 20(1):12. https://doi.org/10.1186/s12879-019-4730-8
Salehi S, Elmi T, Meamar AR, Basi A, Mirhosseini A, Namdari H, Ranjbar M (2018) Investigating the Prevalence of Enteric Opportunistic Parasitic Infections among Cancer Patients of a Teaching Hospital. IJHR 7(1):1–6
Alum A, Rubino JR, Ijaz MK (2010) The global war against intestinal parasites–should we use a holistic approach? Int J Infect Dis 14(9):732–738. https://doi.org/10.1016/j.ijid.2009.11.036
Ziaei Hezarjaribi H, Elmi T, Dayer MS, Gholami Sh, Fakhar M, Akbariqomi M, Ghaffarifar F (2015) systematic review of the effects of Iranian pharmaceutical plant extracts on Giardia lamblia. Asian Pac J Trop Dis 5(12):925–929. https://doi.org/10.1016/S2222-1808(15)60959-8
World Health Organization (2019) Malaria report website: https://www.who.int/publications-detail/world-malaria-report-2019.
Elmi T, Shafiee Ardestani M, Hajialiani F, Motevalian M, Mohamadi M, Zamani Z, Tabatabaie F (2020) Novel chloroquine loaded curcumin based anionic linear globular dendrimer G2: a metabolomics study on Plasmodium falciparum in vitro using 1H NMR spectroscopy. Parasitology 147(7):747–759. https://doi.org/10.1017/S0031182020000372
Kissinger P (2015) Trichomonas vaginalis: a review of epidemiologic, clinical and treatment issues. BMC Infect Dis 15:307. https://doi.org/10.1186/s12879-015-1055-0
Coleman JS, Gaydos CA, Witter F (2013) Trichomonas vaginalis vaginitis in obstetrics and gynecology practice: new concepts and controversies. Obstet Gynecol Surv 68(1):43–50. https://doi.org/10.1097/OGX.0b013e318279fb7d.PMID:23322080;PMCID:PMC3586271
Pires SM, Fischer-Walker CL, Lanata CF, Devleesschauwer B, Hall AJ et al (2015) Aetiology-specific estimates of the global and regional incidence and mortality of diarrhoeal diseases commonly transmitted through food. PLoS ONE 10(12):e0142927. https://doi.org/10.1371/journal.pone.0142927
Degarege A, Degarege D, Veledar E, Erko B, Nacher M, Beck-Sague CM, Madhivanan P (2016) Plasmodium falciparum infection status among children with Schistosoma in Sub-Saharan Africa: a systematic review and meta-analysis. PLoS Neglect Tropic Dis 10912:e0005193. https://doi.org/10.1371/journal.pntd.0005193
Elmi T, Gholami Sh, Rahimi B, Geraili Z, Tabatabaie F (2017) Comparison of sensitivity of sucrose gradient, wet mount and formalin-ether in detecting protozoan Giardia lamblia in stool specimens of BALB/c mice. JPAM 11(1):105–109. https://doi.org/10.22207/JPAM.11.1.14
Bartelt LA, Bolick DT, Mayneris-Perxachs J, Kolling GL, Medlock GL, Zaenker EI, Donowitz J et al (2017) Cross-modulation of pathogen-specific pathways enhances malnutrition during enteric co-infection with Giardia lamblia and enteroaggregative Escherichia coli. PLoS Pathog 13(7):e1006471. https://doi.org/10.1371/journal.ppat.1006471
Hernández Ceruelos A, Romero-Quezada LC, Ruvalcaba Ledezma JC, López Contreras L (2019) Therapeutic uses of metronidazole and its side effects: an update. Eur Rev Med Pharmacol Sci 23(1):397–401. https://doi.org/10.26355/eurrev_201901_16788
Chavez de Paz LE, Resin A, Howard KA, Sutherland DS, Wejse PL (2011) Antimicrobial effect of chitosan nanoparticles on streptococcus mutans biofilms. Appl Environ Microbiol 77(11):3892–3895. https://doi.org/10.1128/AEM.02941-10
Roshdy N, Kataia EM, Helmy A (2019) Assessment of antibacterial activity of 2.5% NaOCl, chitosan nano-particles against Enterococcus faecalis contaminating root canals with and without diode laser irradiation: an in vitro study. Acta Odontol Scand 77(1):39–43. https://doi.org/10.1080/00016357.2018.1498125
Chabra A, Rahimi-Esboei B, Habibi E, Elmi T, Valian H, Akhtari J, Fakhar M (2019) Effects of some natural products from fungal and herbal sources on Giardia lamblia in vivo. Parasitology 146(9):1188–1198. https://doi.org/10.1017/S0031182019000325
Divya K, Vijayan S, George TK (2017) Antimicrobial properties of chitosan nanoparticles: Mode of action and factors affecting activity. Fibers Polym 18:221–230. https://doi.org/10.1007/s12221-017-6690-1
Hosseinnejad M, Jafari SM (2016) Evaluation of different factors affecting antimicrobial properties of chitosan. Int J Biol Macromol 85:467–475. https://doi.org/10.1016/j.ijbiomac.2016.01.022
Abdul HP, Chaturbhuj K, Adnan AS, Nurul MR, Syakir MI, Davoudpour Y, Rafatullah M et al (2016) A review on chitosan-cellulose blends and nanocellulose reinforced chitosan biocomposites: Properties and their applications. Carbohydr Polym 150:216–226. https://doi.org/10.1016/j.carbpol.2016.05.028
Moran HBT, Turley JL, Andersson M, Lavelle EC (2018) Immunomodulatory properties of chitosan polymers. Biomaterials 184:1–9. https://doi.org/10.1016/j.biomaterials.2018.08.054
Kumar MN, Muzzarelli RA, Muzzarelli C, Sashiwa H, Domb AJ (2004) Chitosan chemistry and pharmaceutical perspectives. Chem Rev 104(12):6017–6084. https://doi.org/10.1021/cr030441b
Chanphai P, Tajmir-Riahi HA (2017) Encapsulation of testosterone by chitosan nanoparticles. Int J Biol Macromol 98:535–541. https://doi.org/10.1016/j.ijbiomac.2017.02.007
Fakhar M, Chabra A, Rahimi-Esboei B, Rezaei F (2015) In vitro protoscolicidal effects of fungal chitosan isolated from Penicillium waksmanii and Penicillium citrinum. J Parasit Dis 39(2):162–167. https://doi.org/10.1007/s12639-013-0300-y
Samal SK, Dash M, Van Vlierberghe S, Kaplan DL, Chiellini E, van Blitterswijk C (2012) Cationic polymers and their therapeutic potential. Chem Soc Rev 41(21):7147–7194. https://doi.org/10.1039/C2CS35094G
Wang D, Jiang W (2019) Preparation of chitosan-based nanoparticles for enzyme immobilization. Int J Biol Macromol 126:1125–1132. https://doi.org/10.1016/j.ijbiomac.2018.12.243
Martins GO, Segalla Petrônio M, Furuyama Lima AM, Martinez Junior AM, de Oliveira Tiera VA, de Freitas CM, Vilamaiorb PSL (2019) Amphipathic chitosans improve the physicochemical properties of siRNA-chitosan nanoparticles at physiological conditions. Carbohydr Polym 216:332–342. https://doi.org/10.1016/j.carbpol.2019.03.098
Safdar R, Omar AA, Arunagiri A, Regupathi I, Thanabalan M (2019) Potential of Chitosan and its derivatives for controlled drug release applications—a review. J Drug Deliv Sci Technol 49:642–659. https://doi.org/10.1016/j.jddst.2018.10.020
Pan C, Qian J, Fan J, Guo H, Gou L, Yang H, Liang C (2019) Preparation nanoparticle by ionic cross-linked emulsified chitosan and its antibacterial activity. Colloids Surf A Physicochem 568:362–370. https://doi.org/10.1016/j.colsurfa.2019.02.039
Lee HL, Wang RS, Hsu YC, Chuang CC, Chan HR, Chiu HC, Wang YB (2018) Antifungal effect of tissue conditioners containing poly [acryloyloxyethyltrimethyl ammonium chloride]-grafted chitosan on Candida albicans growth in vitro. J Dent Sci 13(2):160–166. https://doi.org/10.1016/j.jds.2017.06.004
Du Y, Zhao Y, Dai S, Yang B (2009) Preparation of water-soluble chitosan from shrimp shell and its antibacterial activity. Iinnov Food Sci Emerg 10(1):103–107. https://doi.org/10.1016/j.ifset.2008.07.004
Tripathy S, Mahapatra SK, Chattopadhyay S, Das S, Dash SK, Majumder S, Pramanik P, Roy S (2013) A novel chitosan based antimalarial drug delivery against Plasmodium berghei infection. Acta Trop 128(3):494–503. https://doi.org/10.1016/j.actatropica.2013.07.011
Mehrizi T, Shafiee Ardestani M, Haji Molla Hoseini M, Khamesipour A, Mosaffa N, Ramezani A (2018) Novel nanosized chitosan-betulinic acid against resistant Leishmania major and first clinical observation of such parasite in kidney. Sci Rep 8(1):11759. https://doi.org/10.1038/s41598-018-30103-7
Jo HY, Kim Y, Park HW, Moon HW, Kim J, Kim DG, Paek SH (2015) The Unreliability of MTT assay in the cytotoxic test of primary cultured glioblastoma cells. Exp Neurobiol 24(3):235–245. https://doi.org/10.5607/en.2015.24.3.235
Mesdaghinia A, Pourpakc Z, Naddafia K, Nabizadeh Nodehia R, Alizadeh Z, Rezaei S, Mohammadi A, Faraji M (2019) An in vitro method to evaluate hemolysis of human red blood cells (RBCs) treated by airborne particulate matter (PM10). MethodsX 6:156–161. https://doi.org/10.1016/j.mex.2019.01.001
Kidima W, Nkwengulila G (2015) Plasmodium falciparum msp2 genotypes and multiplicity of infections among children under five years with uncomplicated malaria in Kibaha, Tanzania (2015). J Parasitol Res. https://doi.org/10.1155/2015/721201
Hooshyar H, Ghafarinasab S, Arbabi M, Delavari M, Rasti S (2017) Genetic variation of Giardia lamblia isolates from food-handlers in Kashan. Central Iran Iran J Parasitol 12(1):83–89
Upcroft JA, Delgadillo-Correa MG, Dunne RL, Sturm AW, Johnson PJ, Upcroft P (2006) Genotyping Trichomonas vaginalis. Int J Parasitol 36(7):821–828. https://doi.org/10.1016/j.ijpara.2006.02.018
Trager W, Jensen JB (1976) Human malaria parasites in continuous culture. Science 193(4254):673–675. https://doi.org/10.1126/science.781840
Bitencourt FG, de Brum VP, Meirelles LC, Rigo GV, da Silva EF, Gnoatto SCB, Tasca T (2018) Anti-Trichomonas vaginalis activity of ursolic acid derivative: a promising alternative. Parasitol Res 117(5):1573–1580. https://doi.org/10.1007/s00436-018-5839-1
Pradines B, Bories C, Vauthier C, Ponchel G, Loiseau PM, Bouchemal K (2015) Drug-free chitosan coated poly(isobutylcyanoacrylate) nanoparticles are active against Trichomonas vaginalis and non-toxic towards pig vaginal mucosa. Pharm Res 32(4):1229–1236. https://doi.org/10.1007/s11095-014-1528-7
Meri T, Jokiranta TS, Suhonen L, Meri S (2000) Resistance of Trichomonas vaginalis to metronidazole: report of the first three cases from Finland and optimization of in vitro susceptibility testing under various oxygen concentrations. J Clin Microbiol 38(2):763–767
Elmi T, Gholami S, Azadbakht M, Ziaei H (2014) Effect of chloroformic extract of Tanacetum parthenium in the treatment of Giardia lamblia infection in Balb/c mice. JMUMS23(1):157–65. https://jmums.mazums.ac.ir/article-1-3440-fa.html.
Yarahmadi M, Fakhar M, Ebrahimzadeh MA, Chabra A, Rahimi-Esboei B (2016) The anti-giardial effectiveness of fungal and commercial chitosan against Giardia intestinalis cysts in vitro. J Parasitic Dis 40(1):75–80. https://doi.org/10.1007/s12639-014-0449-z
Ficai D, Ardelean IL, Holban AM (2018) Manufacturing nanostructured chitosan-based 2D sheets with prolonged antimicrobial activity. Rom J Morphol Embryol 59(2):517–525
Sadjjadi SM, Rostami J, Azadbakht M (2006) Giardiacidal activity of lemon juice, vinifer and vinegar on Giardia intestinalis cysts. Southeast Asian J Trop Med Public Health 37(suppl 3):24–27
Wilczewska AZ, Niemirowicz-Laskowskaofia K, Markiewicz KH, Car H (2012) Nanoparticles as drug delivery systems. Pharmacol Rep 64(5):1020–1037. https://doi.org/10.1016/s1734-1140[12]70901-5
Elmi T, Gholami S, Fakhar M, Azizi F (2013) A review on the use of nanoparticles in the treatment. J Mazandaran Univ Med Sci 23(102):126–133. https://jmums.mazums.ac.ir/article-1-2396-fa.html.
Gaafar MR, Mady RF, Diab RG, Shalaby TI (2014) Chitosan and silver nanoparticles: promising anti-toxoplasma agents. Exp Parasitol 143:30–38. https://doi.org/10.1016/j.exppara.2014.05.005
Akhtar F, Rizvi MM, Kar SK (2011) Oral delivery of curcumin bound to chitosan nanoparticles cured Plasmodium yoelii infected mice. Biotechnol Adv 30(1):310–320. https://doi.org/10.1016/j.biotechadv.2011.05.009
Mirnejad R, Mofazzal Jahromi MA, Al-Musawi S, Pirestani M, Fasihi Ramandi M, Ahmadi K, Rajayi H (2014) Curcumin-loaded Chitosan Tripolyphosphate Nanoparticles as a safe, natural and effective antibiotic inhibits the infection of Staphylococcus aureus and Pseudomonas aeruginosa in vivo. Iran J Biotechnol 12(3):1012. https://doi.org/10.15171/IJB.1012
Acknowledgements
We should express our best gratitude to Pasteur Institute of Iran, Mazandaran University of Medical Sciences, and Faculty of Pharmacy, Tehran University of Medical Sciences, for providing P. falciparum strains and allowing us to use their biotechnology labs to prepare nano-chitosan. Also, we would like to take this opportunity to thank Iran University of Medical Sciences for providing the necessary fund to perform the present research.
Funding
This work was supported by Iran University of Medical Sciences (code: 97-4-4-13714).
Author information
Authors and Affiliations
Contributions
TE, BRE, ZZ, MF: conceived, analyzed data, and designed the study; MD, AC, FS, FH: performed experiments, provided samples; FT: supervised, and wrote the paper; MJN: wrote the paper.
Corresponding authors
Ethics declarations
Conflict of interest
We declare that there is no conflict of interest regarding the present study.
Ethical approval
This study was approved by the Ethical Committee of Iran University of Medical Sciences in accordance with Helsinki Declaration guidelines. In this regard, the ethical code of IR.IUMS.FMD.REC.1397.219 was designated to the present study.
Consent for publication
The authors declare that they have no competing interests regarding the publication of this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elmi, T., Rahimi Esboei, B., Sadeghi, F. et al. In Vitro Antiprotozoal Effects of Nano-chitosan on Plasmodium falciparum, Giardia lamblia and Trichomonas vaginalis. Acta Parasit. 66, 39–52 (2021). https://doi.org/10.1007/s11686-020-00255-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11686-020-00255-6