Abstract
Purpose
Depression and impairment of quality of life (QoL) reduce the survival of individual on hemodialysis (HD). However, few studies evaluated the impact of these conditions on the survival of older patients undergoing HD.
Methods
A retrospective cohort study was performed including patients aged ≥ 60 years on HD in Recife, Brazil, assessed in 2013 and monitored until 2017. Depression was evaluated with the Mini-International Neuropsychiatric Interview and QoL with the Control, Autonomy, Self-realization, and Pleasure Questionnaire (CASP-16). Survival differences according to the depression and QoL status were measured by Kaplan–Meier analysis and Cox regression. Death Certificates were analyzed to assess the cause of death.
Results
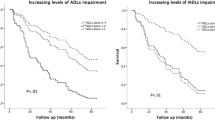
A total of 171 patients were included (mean age 68.7 ± 6.9 years). The mean follow-up time was 3 years (maximum 4.5 years) and there were 98 deaths (57.3% of the sample). In a multivariate model that included depression and QoL, only QoL impairment was associated with a higher risk of death (HR 1.62, p = 0.035). Among CASP domains, only “Control” was associated with survival (HR 0.90, p = 0.014). Depression was unrelated to the cause of death, but there was a trend for death by endocrine diseases if QoL was impaired (p = 0.057).
Conclusion
QoL impairment is a key predictor of prognosis in older patients on HD and may be more important than depression. It is important that teams dealing with this population include in protocols an assessment of QoL, in order to offer a range of care according to the needs of these patients.

Similar content being viewed by others
References
Kremers, W. K., Denic, A., Lieske, J. C., Alexander, M. P., Kaushik, V., Elsherbiny, H. E., et al. (2015). Distinguishing age-related from disease-related glomerulosclerosis on kidney biopsy: The Aging Kidney Anatomy study. Nephrology Dialysis Transplantation,30(12), 2034–2039. https://doi.org/10.1093/ndt/gfv072.
Kirkman, M. S., Briscoe, V. J., Clark, N., Florez, H., Haas, L. B., Halter, J. B., et al. (2012). Diabetes in older adults. Diabetes Care,35(12), 2650–2664. https://doi.org/10.2337/dc12-1801.
Sesso, R. C., Lopes, A. A., Thomé, F. S., Lugon, J. R., & Martins, C. T. (2017). Brazilian chronic dialysis survey 2016. Jornal Brasileiro de Nefrologia,39(3), 261–266. https://doi.org/10.5935/0101-2800.20170049.
Kramer, A., Pippias, M., Noordzij, M., Stel, V. S., Andrusev, A. M., Aparicio-Madre, M. I., et al. (2019). The European renal association—European dialysis and transplant association (ERA-EDTA) Registry Annual Report 2016: A summary. Clinical Kidney Journal. https://doi.org/10.1093/ckj/sfz011.
United States Renal Data System. 2018 USRDS annual data report. (2018). Chapter 1: Incidence, prevalence, patient characteristics, and treatment modalities. American Journal of Kidney Diseases, 71(3), S247–S276. https://doi.org/10.1053/j.ajkd.2018.01.014.
Martiny, C., de Oliveira e Silva, A. C., Neto, J. P. S., & Nardi, A. E. (2012). Psychiatric disorders in patients with end-stage renal disease. Journal of Renal Care,38(3), 131–137. https://doi.org/10.1111/j.1755-6686.2012.00261.x.
Palmer, S., Vecchio, M., Craig, J. C., Tonelli, M., Johnson, D. W., Nicolucci, A., et al. (2013). Prevalence of depression in chronic kidney disease: Systematic review and meta-analysis of observational studies. Kidney International,84(1), 179–191. https://doi.org/10.1038/ki.2013.77.
Alencar, S. B. V., de Lima, F. M., Dias, L. D. A., Dias, V. D. A., Lessa, A. C., Bezerra, J. M., et al. (2019). Depression and quality of life in older adults on hemodialysis. Brazilian Journal of Psychiatry. https://doi.org/10.1590/1516-4446-2018-0345.
Unruh, M. L., Newman, A. B., Larive, B., Dew, M. A., Miskulin, D. C., Greene, T., et al. (2008). The influence of age on changes in health-related quality of life over three years in a cohort undergoing hemodialysis. Journal of the American Geriatrics Society,56(9), 1608–1617. https://doi.org/10.1111/j.1532-5415.2008.01849.x.
Lamping, D. L., Constantinovici, N., Roderick, P., Normand, C., Henderson, L., Harris, S., et al. (2000). Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: A prospective cohort study. Lancet,356(9241), 1543–1550. https://doi.org/10.1016/S0140-6736(00)03123-8.
Cruz, L. N., Fleck, M. P., & Polanczyk, C. A. (2010). Depression as a determinant of quality of life in patients with chronic disease: Data from Brazil. Social psychiatry and psychiatric epidemiology,45(10), 953–961. https://doi.org/10.1007/s00127-009-0141-2.
Balogun, R. A., Turgut, F., Balogun, S. A., Holroyd, S., & Abdel-Rahman, E. M. (2011). Screening for depression in elderly hemodialysis patients. Nephron Clinical Practice,118(2), c72–c77. https://doi.org/10.1159/000320037.
Chilcot, J., Guirguis, A., Friedli, K., Almond, M., Day, C., Da Silva-Gane, M., et al. (2018). Depression symptoms in haemodialysis patients predict all-cause mortality but not kidney transplantation: A cause-specific outcome analysis. Annals of Behavioral Medicine,52(1), 1–8. https://doi.org/10.1007/s12160-017-9918-9.
Palmer, S. C., Vecchio, M., Craig, J. C., Tonelli, M., Johnson, D. W., Nicolucci, A., et al. (2013). Association between depression and death in people with CKD: A meta-analysis of cohort studies. American Journal of Kidney Diseases,62(3), 493–505. https://doi.org/10.1053/j.ajkd.2013.02.369.
Zhou, X., Xue, F., Wang, H., Qiao, Y., Liu, G., Huang, L., et al. (2017). The quality of life and associated factors in patients on maintenance hemodialysis—A multicenter study in Shanxi province. Renal Failure,39(1), 707–711. https://doi.org/10.1080/0886022X.2017.1398095.
Pan, C. W., Wu, Y., Zhou, H. J., Xu, B. X., & Wang, P. (2018). Health-related quality of life and its factors of hemodialysis patients in Suzhou China. Blood Purification,45(4), 327–333. https://doi.org/10.1159/000485962.
Farrokhi, F., Abedi, N., Beyene, J., Kurdyak, P., & Jassal, S. V. (2014). Association between depression and mortality in patients receiving long-term dialysis: A systematic review and meta-analysis. American Journal of Kidney Diseases,63(4), 623–635. https://doi.org/10.1053/j.ajkd.2013.08.024.
Van Loon, I. N., Bots, M. L., Boereboom, F. T. J., Grooteman, M. P. C., Blankestijn, P. J., Van Den Dorpel, M. A., et al. (2017). Quality of life as indicator of poor outcome in hemodialysis: Relation with mortality in different age groups. BMC Nephrology,18(1), 1–9. https://doi.org/10.1186/s12882-017-0621-7.
Hall, R. K., Luciano, A., Pieper, C., & Colón-Emeric, C. S. (2018). Association of kidney disease quality of life (KDQOL-36) with mortality and hospitalization in older adults receiving hemodialysis. BMC Nephrology,19(1), 11. https://doi.org/10.1186/s12882-017-0801-5.
Rinaldi, P., Mecocci, P., Benedetti, C., Ercolani, S., Bregnocchi, M., Menculini, G., et al. (2003). Validation of the five-item geriatric depression scale in elderly subjects in three different settings. Journal of the American Geriatrics Society,51(5), 694–698. https://doi.org/10.1034/j.1600-0579.2003.00216.x.
Sheehan, D. V, Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of clinical psychiatry, 59 (Suppl 2), 22–33; quiz 34-57. https://doi.org/10.1016/S0924-9338(99)80239-9
Lima, F. M., Hyde, M., Chungkham, H. S., Correia, C., Siqueira Campos, A., Campos, M., et al. (2014). Quality of life amongst older Brazilians: A cross-cultural validation of the CASP-19 into Brazilian-Portuguese. PLoS ONE,9(4), 1–8. https://doi.org/10.1371/journal.pone.0094289.
Hyde, M., Wiggins, R. D., Higgs, P., & Blane, D. B. (2003). A measure of quality of life in early old age: The theory, development and properties of a needs satisfaction model (CASP-19). Aging & Mental Health,7(3), 186–194. https://doi.org/10.1080/1360786031000101157.
Hecking, M., Bieber, B. A., Ethier, J., Kautzky-Willer, A., Sunder-Plassmann, G., Säemann, M. D., et al. (2014). Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: The dialysis outcomes and practice patterns study (DOPPS). PLoS Medicine. https://doi.org/10.1371/journal.pmed.1001750.
Eknoyan, G., Beck, G. J., Cheung, A. K., Daugirdas, J. T., Greene, T., Kusek, J. W., et al. (2002). Effect of dialysis dose and membrane flux in maintenance hemodialysis. New England Journal of Medicine,347(25), 2010–2019. https://doi.org/10.1056/NEJMoa021583.
Park, J.-M., Lee, J.-H., Jang, H. M., Park, Y., Kim, Y. S., Kang, S.-W., et al. (2018). Survival in patients on hemodialysis: Effect of gender according to body mass index and creatinine. PLoS ONE,13(5), e0196550. https://doi.org/10.1371/journal.pone.0196550.
Ebrahimi, V., Khademian, M. H., Masoumi, S. J., Morvaridi, M. R., & Ezzatzadegan Jahromi, S. (2019). Factors influencing survival time of hemodialysis patients; Time to event analysis using parametric models: A cohort study. BMC Nephrology,20(1), 1–9. https://doi.org/10.1186/s12882-019-1382-2.
Tuǧcu, M., Kasapoǧlu, U., Şahin, G., & Apaydin, S. (2018). The factors affecting survival in geriatric hemodialysis patients. International Journal of Nephrology. https://doi.org/10.1155/2018/5769762.
Balogun, R. A., Balogun, S. A., Kepple, A. L., Ma, J. Z., Turgut, F., Kovesdy, C. P., et al. (2011). The 15-item geriatric depression scale as a predictor of mortality in older adults undergoing hemodialysis. Journal of the American Geriatrics Society,59(8), 1563–1565. https://doi.org/10.1111/j.1532-5415.2011.03533.x.
Genestier, S., Meyer, N., Chantrel, F., Alenabi, F., Brignon, P., Maaz, M., et al. (2010). Prognostic survival factors in elderly renal failure patients treated with peritoneal dialysis: A nine-year retrospective study. Peritoneal Dialysis International,30(2), 218–226. https://doi.org/10.3747/pdi.2009.00043.
Gilman Scd, S. E., Sucha, E., Kingsbury, M., Scd, N. J. H., Murphy, J. M., & Colman, I. (2017). Depression and mortality in a longitudinal study: 1952–2011. CMAJ,189, 1304–1314. https://doi.org/10.1503/cmaj.170125.
Liu, Y., Ho, R. C.-M., & Mak, A. (2012). Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: A meta-analysis and meta-regression. Journal of Affective Disorders,139(3), 230–239. https://doi.org/10.1016/j.jad.2011.08.003.
Ryan, J., Pilkington, L., Neuhaus, K., Ritchie, K., Ancelin, M. L., & Saffery, R. (2017). Investigating the epigenetic profile of the inflammatory gene IL-6 in late-life depression. BMC Psychiatry,17(1), 1–7. https://doi.org/10.1186/s12888-017-1515-8.
Wei, J., Fan, L., Zhang, Y., Li, S., Partridge, J., Claytor, L., et al. (2018). Association between malnutrition and depression among community-dwelling older Chinese adults. Asia Pacific Journal of Public Health,30(2), 107–117. https://doi.org/10.1177/1010539518760632.
Allawi, A. A. D. (2018). Malnutrition, inflamation and atherosclerosis (MIA syndrome) in patients with end stage renal disease on maintenance hemodialysis (a single centre experience). Diabetes & Metabolic Syndrome: Clinical Research & Reviews,12(2), 91–97. https://doi.org/10.1016/j.dsx.2017.09.003.
Vaccarino, V., Badimon, L., Bremner, J. D., Cenko, E., Cubedo, J., Dorobantu, M., et al. (2019). Depression and coronary heart disease: 2018 ESC position paper of the working group of coronary pathophysiology and microcirculation developed under the auspices of the ESC Committee for Practice Guidelines. European Heart Journal. https://doi.org/10.1093/eurheartj/ehy913.
Chen, I. M., Lin, P. H., Wu, V. C., Wu, C. S., Shan, J. C., Chang, S. S., et al. (2017). Suicide deaths among patients with end-stage renal disease receiving dialysis: A population-based retrospective cohort study of 64,000 patients in Taiwan. Journal of Affective Disorders,227(17), 7–10. https://doi.org/10.1016/j.jad.2017.10.020.
Kurella, M., Kimmel, P. L., Young, B. S., & Chertow, G. M. (2005). Suicide in the United States end-stage renal disease program. Journal of the American Society of Nephrology,16(3), 774–781. https://doi.org/10.1681/ASN.2004070550.
Davison, S. N., & Jassal, S. V. (2016). Supportive care: Integration of patient-centered kidney care to manage symptoms and geriatric syndromes. Clinical Journal of the American Society of Nephrology,11(10), 1882–1891. https://doi.org/10.2215/CJN.01050116.
Foote, C., Morton, R. L., Jardine, M., Gallagher, M., Brown, M., Howard, K., et al. (2014). COnsiderations of nephrologists when suggesting dialysis in elderly patients with renal failure (CONSIDER): A discrete choice experiment. Nephrology Dialysis Transplantation,29(12), 2302–2309. https://doi.org/10.1093/ndt/gfu257.
Netuveli, G., Pikhart, H., Bobak, M., & Blane, D. (2012). Generic quality of life predicts all-cause mortality in the short term: evidence from British Household Panel Survey. Journal of Epidemiology and Community Health,66(10), 962–966. https://doi.org/10.1136/jech-2011-200310.
Almeida, O. P., Alfonso, H., Hankey, G. J., & Flicker, L. (2010). Depression, antidepressant use and mortality in later life: The health in men study. PLoS ONE,5(6), 1–10. https://doi.org/10.1371/journal.pone.0011266.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study conception and design: SBVA, KCLP, FM, LAD, and VAD; data collection: SBVA and FML; data analysis and interpretation: SBVA and URM; statistical analysis: SBVA and URM. Writing—review and editing: SBVA, KCLP, LAD, and VAD. All authors contributed significant intellectual content during the preparation and revision of this manuscript and take full responsibility for the overall work, ensuring proper investigation and clarification of issues regarding the accuracy or integrity of any part of this work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Alencar, S.B.V., Dias, L.A., Dias, V.A. et al. Quality of life may be a more valuable prognostic factor than depression in older hemodialysis patients. Qual Life Res 29, 1829–1838 (2020). https://doi.org/10.1007/s11136-020-02445-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02445-1