Abstract
Purpose
This study aimed to explore different aspects of executive function in patients with acromegaly and investigate the cause of dysexecutive syndrome in these patients.
Methods
We conducted five typical executive function tests (Stroop test, verbal fluency [VF] test, Hayling Sentence Completion Test [HSCT], N-back test, and Sustained Attention to Response Task [SART]) on 42 acromegalic patients and 42 strictly matched healthy controls. Comparative analyses were conducted for five major executive function domains. The Dysexecutive Questionnaire (DEX) was used to assess patients’ subjective feelings about their executive function. All patients underwent a magnetic resonance imaging (MRI) examination and a blood test to determine their pituitary hormone levels before the tests were performed.
Results
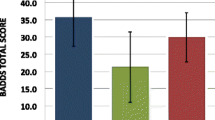
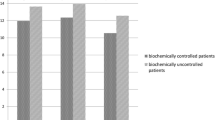
The patients exhibited worse results on the Stroop test, VF test, HSCT and N-back test compared to the healthy control group. Moreover, part B of the HSCT and the N-back test performance were negatively correlated with IGF-1 concentrations, and the duration of the disease was significantly associated with the Stroop color task results.
Conclusions
Acromegalic patients were severely impaired in semantic inhibition, executive processing, working memory and executive inhibition, and they have realized a portion of these deficits. A high level of IGF-1, disease duration may contribute to the impairment of specific aspects of executive function.
Similar content being viewed by others
References
Holdaway IM, Rajasoorya RC, Gamble GD (2004) Factors influencing mortality in acromegaly. J Clin Endocrinol Metab 89(2):667–674
Melmed S, Casanueva FF, Klibanski A et al (2013) A consensus on the diagnosis and treatment of acromegaly complications. Pituitary 16(3):294
Melmed S (2016) New therapeutic agents for acromegaly. Nat Rev Endocrinol 12(2):90–98
Abreu A, Tovar AP, Castellanos R et al (2016) Challenges in the diagnosis and management of acromegaly: a focus on comorbidities. Pituitary 19(4):448–457
Colao A, Ferone D, Marzullo P, Lombardi G (2004) Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev 25(1):102
Leoncarrion J, Martinrodriguez JF, Madrazoatutxa A et al (2010) Evidence of cognitive and neurophysiological impairment in patients with untreated naive acromegaly. J Clin Endocrinol Metab 95(9):4367–4379
Chan RCK, Shum D, Toulopoulou T, Chen EYH (2008) Assessment of executive functions: Review of instruments and identification of critical issues. Arch Clin Neuropsychol 23(2):201
Elliott R (2003) Executive functions and their disorders. Br Med Bull 65(486):49–59
Monsell S (2003) Task switching. Trends Cogn Sci 7(3):134–140
Katznelson L, Atkinson JL, Cook DM, Ezzat SZ, Hamrahian AH, Miller KK (2011) American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Diagnosis and Treatment of Acromegaly–2011 update: executive summary. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 17(4):1–44
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33(4):610–618
Cottier JP, Destrieux C, Brunereau L et al (2000) Cavernous sinus invasion by pituitary adenoma: MR imaging. Radiology 215(2):463–469
Lee TM, Chan CC (2000) Stroop interference in Chinese and English. J Clin Exp Neuropsychol 22(22):465–471
Burgess PW, Veitch E, De LCA, Shallice T (2000) The cognitive and neuroanatomical correlates of multitasking. Neuropsychologia 38(6):848–863
Fang L, Huang J, Zhang Q, Chan RC, Wang R, Wan W (2016) Different aspects of dysexecutive syndrome in patients with moyamoya disease and its clinical subtypes. J Neurosurg 125(2):1
Johnson-Selfridge MT, Zalewski C, Aboudarham JF (1998) The relationship between ethnicity and word fluency. Arch Clin Neuropsychol 13(3):319–325
Callicott JH, Ramsey NF, Tallent K et al (1998) Functional magnetic resonance imaging brain mapping in psychiatry: Methodological issues illustrated in a study of working memory in schizophrenia. Neuropsychopharmacology 18(3):186–196
Chan RC, Chen EY, Cheung EF, Chen RY, Cheung HK (2004) A study of sensitivity of the sustained attention to response task in patients with schizophrenia. Clin Neuropsychol 18(1):114–121
Robertson IH, Manly T, Andrade J, Baddeley BT, Yiend J (1997) ‘Oops!’: performance correlates of everyday attentional failures in traumatic brain injured and normal subjects. Neuropsychologia 35(6):747–758
Chan RCK (2001) Dysexecutive symptoms among a non-clinical sample: A study with the use of the Dysexecutive Questionnaire. Br J Psychol 92(3):551–565
Sievers C, Samann PG, Pfister H et al (2012) Cognitive function in acromegaly: description and brain volumetric correlates. Pituitary 15(3):350–357
Crespo I, Santos A, Valassi E, Pires P, Webb SM, Resmini E (2015) Impaired decision making and delayed memory are related with anxiety and depressive symptoms in acromegaly. Endocrine 50(3):756–763
Tanriverdi F, Yapislar H, Karaca Z, Unluhizarci K, Suer C, Kelestimur F (2008) Evaluation of cognitive performance by using P300 auditory event related potentials (ERPs) in patients with growth hormone (GH) deficiency and acromegaly. Growth Horm Igf Res Off J Growth Horm Res Soc Int Igf Res Soc 19(1):24–30
Sievers C, Sämann PG, Dose T et al (2009) Macroscopic brain architecture changes and white matter pathology in acromegaly: a clinicoradiological study. Pituitary 12(3):177
Crespo I, Webb SM (2014) Perception of health and cognitive dysfunction in acromegaly patients. Endocrine 46(3):365–367
Burke SN, Barnes CA (2006) Neural plasticity in the ageing brain. Nat Rev Neurosci 7(1):30–40
Sonntag WE, Ramsey M, Carter CS (2005) Growth hormone and insulin-like growth factor-1 (IGF-1) and their influence on cognitive aging. Ageing Res Rev 4(2):195
Müssig K, Leyhe T, Besemer B et al (2009) Younger age is a good predictor of better executive function after surgery for pituitary adenoma in adults. J Int Neuropsychol Soc 15(5):803–806
Acknowledgements
We thank all the authors of the included studies.
Funding
This study was funded by the National Natural Science Foundation of China (Grant Nos. 81,172,192 and 31,100,747) and the High-level Health Technology Personnel Training Program of Beijing Health System (Grant No. 2014-3-036).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all of the individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shan, S., Fang, L., Huang, J. et al. Evidence of dysexecutive syndrome in patients with acromegaly. Pituitary 20, 661–667 (2017). https://doi.org/10.1007/s11102-017-0831-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-017-0831-9