Abstract
Dapsone (DAP) is a long-established molecule that remains a promising therapeutic agent for various diseases mainly because it combines antimicrobial and anti-inflammatory activities. Its oral application, however, is limited by the dose-dependent hematological side effects that may rise from systemic exposure. As an alternative to overcome this limitation, the administration of DAP to the skin has witnessed prominent interest in the past 20 years, particularly when applied to the treatment of dermatological disorders. In this review, all technological strategies proposed to the topical delivery of DAP are presented. Most of the reported studies have been devoted to the clinical use and safety of a gel formulation containing both solubilized and microcrystalline drug, however, the technological characteristics of such preparation are still missing. In parallel, the incorporation of DAP into vesicular and particulate carriers (e.g. nano- and microemulsions, niosomes, invasomes, bilosomes, cubosomes, solid lipid nanoparticles, nanostructured lipid carriers, polymeric nanocapsules and polymer-lipid-polymer hybrid nanoparticles) appears to be an alternative to provide greater drug release control, enhanced drug solubilization and follicular targeting. Indeed, the main application of DAP topical formulations reported in the literature was the treatment of acne vulgaris, a disease located in the hair follicle. Other diseases affecting different regions of the skin (e.g. cutaneous lupus erythematosus and cutaneous leishmaniasis), however, may also benefit from a topical therapeutic regimen containing DAP. Therefore, the investigation of appendageal route in comparison to passive transmembrane diffusion as a function of targeted disease, as well as pharmacokinetic studies, are perspectives highlighted herein. Such studies may drive future efforts towards the rational development of safe and effective technologies to deliver DAP to the skin.

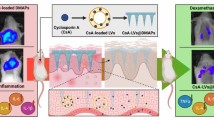
Graphical abstract




Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- BCS:
-
Biopharmaceutical classification system
- CLE:
-
Cutaneous lupus erythematosus
- DAC/NRF:
-
The German Drug Codex/New German Formulary
- DAP:
-
Dapsone
- EE:
-
Encapsulation efficiency
- FDA:
-
U.S. Food and Drug Administration
- HET-CAM:
-
Hen’s Egg Test – Chorioallantoic Membrane
- ME:
-
Microemulsion
- NE:
-
Nanoemulsion
- NLC:
-
Nanostructured lipid carriers
- SLN:
-
Solid lipid nanoparticles
References
Rang HP, Dale MM, Ritter JM, Flower RJ. Rang & Dale’s pharmacology. 7th ed. London: Churchill Livingstone; 2011. 792 p.
Brunton L, Chabner B, Knollman B. Goodman and Gilman’s the pharmacological basis of therapeutics, twelfth edition. 12th ed. McGraw-Hill Education: New York City; 2011. 1808 p.
Remington JP. In: Allen LV, Adejare A, Desselle S, Felton L, Moffat A, editors. Remington - the science and practice of pharmacy. 22nd ed. London: Pharmaceutical Press; 2012. 3024 p.
Wozel G, Blasum C. Dapsone in dermatology and beyond. Arch Dermatol Res. 2014;306(2):103–24.
Gillis TP. Mycobacterium leprae. In: Tang Y-W, Sussman M, Liu D, Poxton I, Shwartzman J, editors. Molecular medical microbiology. 2nd ed. Boston: Academic Press; 2015. p. 1655–68.
Wozel VEG. Innovative use of dapsone. Dermatol Clin. 2010;28(3):599–610.
Wolf R, Orni-Wasserlauf R. A century of the synthesis of dapsone: its anti-infective capacity now and then. Int J Dermatol. 2000;39(10):779–83.
Farrah G, Tan E. The use of oral antibiotics in treating acne vulgaris: a new approach. Dermatol Ther. 2016;29(5):377–84.
Ghaoui N, Hanna E, Abbas O, Kibbi AG, Kurban M. Update on the use of dapsone in dermatology. Int J Dermatol. 2020:1–9.
Yost JM, Christopher S, Hale, Meehan SA, BN ML. Dermatitis herpetiformis. Dermatol Online J. 2015;20(12).
Lockwood D, Mariowe S, Leprosy LS. In: Finch R, Greenwood D, Whitley R, Norrby SR, editors. Antibiotic and chemotherapy. 9th ed. London: Saunders Elsevier; 2010. p. 916.
Williams DL, Spring L, Harris E, Roche P, Gillis TP. Dihydropteroate synthase of Mycobacterium leprae and dapsone resistance. Antimicrob Agents Chemother. 2000;44(6):1530–7.
WHO. Leprosy elimination [Internet]. Leprosy. 2020. Available from: http://www.who.int/lep/mdt/en/
Lindenberg M, Kopp S, Dressman JB. Classification of orally administered drugs on the World Health Organization model list of essential medicines according to the biopharmaceutics classification system. Eur J Pharm Biopharm. 2004;58(2):265–78.
Monteiro LM, Lione VF, do Carmo FA, do Amaral LH, da Silva JH, Nasciutti LE, et al. Development and characterization of a new oral dapsone nanoemulsion system: permeability and in silico bioavailability studies. Int J Nanomedicine. 2012;7:5175–82.
Ahmad R, Rogers H. Pharmacokinetics and protein binding interactions of dapsone and pyrimethamine. Br J Clin Pharmacol. 1980;10(5):519–24.
Zuidema J, Hilbers-Modderman ESM, Merkus FWHM. Clinical pharmacokinetics of Dapsone. Clin Pharm. 1986;11:299–315.
Molinelli E, Paolinelli M, Campanati A, Brisigotti V, Offidani A. Metabolic, pharmacokinetic, and toxicological issues surrounding dapsone. Expert Opin Drug Metab Toxicol. 2019;15(5):367–79.
Chong BF, Werth VP. Management of cutaneous lupus erythematosus. In: Wallace D, Hahn B, editors. Dubois’ Lupus erythematosus and related syndromes. 9th ed. London: Elsevier; 2018. p. 816.
Pickert A, Raimer S. An evaluation of dapsone gel 5% in the treatment of acne vulgaris. Expert Opinon Pharmacother. 2009;10(9):1515–21.
Al-Salama ZT, Deeks ED. Dapsone 7.5% gel: a review in acnes vulgaris. Am J Clin Dermatol. 2017;18(1):139–45.
Scheinfeld N. Aczone, a topical gel formulation of the antibacterial, anti-inflammatory Dapsone for the treatment of acne. Curr Opin Investig Drugs. 2009;10(5):474–81.
Stotland M, Shalita AR, Kissling RF. Dapsone 5% Gel. Am J Clin Dermatol. 2009;10:221–7.
Thiboutot DM, Kircik L, McMichael A, Cook-Bolden FE, Tyring SK, Berk DR, et al. Efficacy, safety, and dermal tolerability of Dapsone gel, 7.5% in patients with moderate acne vulgaris: a pooled analysis of two phase 3 trials. J Clin Aesthet Dermatol. 2016;9(10):18–27.
Tanghetti EA, Dhawan S, Green L, Ling M, Downie J, Germain MA, et al. Clinical evidence for the role of a topical anti-inflammatory agent in Comedonal acne: findings from a randomized study of Dapsone gel 5% in combination with Tazarotene cream 0.1% in patients with acne vulgaris. J Drugs Dermatol. 2011;10(7):783–92.
FDA. The Orange Book: Approved Drug Products with Therapeutic Equivalence evaluations [Internet]. U.S. Food & Drug Administration. 2020. Available from: https://www.accessdata.fda.gov/scripts/cder/ob/
Belum VR, Marchetti MA, Dusza SW, Cercek A, Kemeny NE, Lacouture ME. A prospective, randomized, double-blinded, split-face/chest study of prophylactic topical dapsone 5% gel vs. moisturizer for the prevention of cetuximab-induced acneiform rash. J Am Acad Dermatol. 2017;77(3):577–9.
Ferguson L, Fearfield L. Topical dapsone gel is a new treatment option for acne agminata. Clin Exp Dermatol. 2019;44(4):453–5.
Frieling GW, Williams NL, Lim SJM, Rosenthal SI. Novel use of topical Dapsone 5% gel for erythema Elevatum Diutinum: safer and effective. J Drugs Dermatol. 2013;12(4):481–4.
Burbidge T, Haber RM. Topical Dapsone 5% gel as an effective therapy in dermatitis Herpetiformis. J Cutan Med Surg. 2016;20(6):600–1.
Babalola O, Zhang J, Kristjansson A, Whitaker-Worth D, McCusker M. Granuloma faciale treated with topical dapsone: a case report. Dermatol Online J. 2014;20(8).
Faghihi G, Khosravani P, Nilforoushzadeh MA, Hosseini SM, Assaf F, Zeinali N, et al. Dapsone gel in the treatment of papulopustular rosacea: a double-blind randomized clinical trial. J Drugs Dermatol. 2015;14(6):602–6.
Broussard KC, Berger TG, Rosenblum M, Murase JE. Erosive pustular dermatosis of the scalp: a review with a focus on dapsone therapy. J Am Acad Dermatol. 2012;66(4):680–6.
Doolan BJ, Cranwell WC, Nicolopoulos J, Dolianitis C. Topical dapsone gel for treatment of axillary subcorneal pustular dermatosis. J Dermatol. 2019;46(11):e437–8.
Barry BW. Novel mechanisms and devices to enable successful transdermal drug delivery. Eur J Pharm Sci. 2001;14(2):101–14.
Alexander A, Dwivedi S, Ajazuddin, Giri TK, Saraf S, Saraf S, et al. Approaches for breaking the barriers of drug permeation through transdermal drug delivery. J Control Release. 2012;164(1):26–40.
Mak WC, Patzelt A, Richter H, Renneberg R, Lai KK, Rühl E, et al. Triggering of drug release of particles in hair follicles. J Control Release. 2012;160(3):509–14.
Lane ME. Skin penetration enhancers. Int J Pharm. 2013;447(1–2):12–21.
Bouwstra JA, Honeywell-Nguyen PL. Skin structure and mode of action of vesicles. Adv Drug Deliv Rev. 2002;54(1):S41–55.
Bouwstra JA, Honeywell-nguyen PL, Gooris GS, Ponec M. Structure of the skin barrier and its modulation by vesicular formulations. Prog Lipid Res. 2003;42:1–36.
Vyas A, Sonker AK, Gidwani B. Carrier-based drug delivery system for treatment of acne. Sci World J 2014;2014(276260):1–14.
Menon GK. New insights into skin structure: scratching the surface. Adv Drug Deliv Rev. 2002;54(SUPPL):S3.
Venuganti VV, Sahdev P, Hildreth M, Guan X, Perumal O. Structure-skin permeability relationship of dendrimers. Pharm Res. 2011;28(9):2246–60.
Homayun B, Lin X, Choi HJ. Challenges and recent progress in oral drug delivery systems for biopharmaceuticals. Pharmaceutics. 2019;11(3).
Prausnitz MR, Langer R. Transdermal drug delivery. Nat Biotechnol. 2009;26(11):1261–8.
Kanitakis J. Anatomy, histology and immunohistochemistry of normal human skin. Eur J Dermatol. 2002;12(4):390–9.
Menon GK, Cleary GW, Lane ME. The structure and function of the stratum corneum. Int J Pharm. 2012;435(1):3–9.
van Smeden J, Janssens M, Gooris GS, Bouwstra JA. The important role of stratum corneum lipids for the cutaneous barrier function. Biochim Biophys Acta Mol Cell Biol Lipids. 2014;1841(3):295–313.
Moreno E, Calvo A, Schwartz J, Navarro-Blasco I, González-Peñas E, Sanmartín C, et al. Evaluation of skin permeation and retention of topical dapsone in murine cutaneous leishmaniasis lesions. Pharmaceutics. 2019;11(607):1–19.
Hedaya MA. Basic pharmacokinetics. Boca Raton: CRC Press; 2012. 595 p.
Mlosek RK, Malinowska S, Sikora M, Debowska R, Stepień A, Czekaj K, et al. The use of high frequency ultrasound imaging in skin moisturization measurement. Skin Res Technol. 2013;19(2):169–75.
Hoenig LJ. Molecular mechanisms of skin aging and age-related diseases. Skinmed. 2017;15(3):240.
Elbe-Bürger A. Skin architecture and function. In: Kamolz LP, Jeschke MG, Horch RE, Küntscher M, Brychta P, editors. Handbook of burns. Wien: Springer; 2012. p. 29–46.
Neupane R, Boddu SHS, Renukuntla J, Babu RJ, Tiwari AK. Alternatives to biological skin in permeation studies: current trends and possibilities. Pharmaceutics. 2020;12(2).
Wong TW. Electrical, magnetic, photomechanical and cavitational waves to overcome skin barrier for transdermal drug delivery. J Control Release. 2014;193:257–69.
Benson H. Transdermal drug delivery: penetration enhancement techniques. Curr Drug Deliv. 2005;2(1):23–33.
Barry BW. Drug delivery routes in skin: a novel approach. Adv Drug Deliv Rev. 2002;54(SUPPL):31–40.
Fang C-L, Aljuffali IA, Li Y-C, Fang J-Y. Delivery and targeting of nanoparticles into hair follicles. Ther Deliv. 2014;5(9):991–1006.
Cordain L, Lindeberg S, Hurtado M, Hill K, Eaton B, Brand-Miller J. Acne vulgaris: a disease of western civilization. Arch Dermatol. 2002;138(12):1584–90.
Suh DH, Kwon HH. What’s new in the physiopathology of acne? Br J Dermatol. 2015;172(S1):13–9.
Knor T. The pathogenesis of acne. Acta Dermatovenerologica Croat. 2005;13(1):44–9.
Degitz K, Placzek M, Borelli C, Plewig G. Pathophysiology of acne. JDDG - J Ger Soc Dermatol. 2007;5(4):316–23.
Dawson AL, Dellavalle RP. Acne vulgaris. BMJ. 2013;346(7907):1–7.
Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012;379(9813):361–72.
Sardana K, Gupta T, Garg VK, Ghunawat S. Antibiotic resistance to Propionobacterium acnes: worldwide scenario, diagnosis and management. Expert Rev Anti-Infect Ther. 2015;13(7):883–96.
Zaenglein AL. Acne vulgaris. N Engl J Med. 2018;379(14):1343–52.
Kuhn A, Sticherling M, Bonsmann G. Klinische manifestationen des kutanen lupus erythematodes. JDDG - J Ger Soc Dermatol. 2007;5(12):1124–37.
Wenzel J. Cutaneous lupus erythematosus: new insights into pathogenesis and therapeutic strategies. Nat Rev Rheumatol. 2019;15(9):519–32.
Kuhn A, Rondinone R, Doria A, Shoenfeld Y. 1st international conference on cutaneous lupus Erythematosus Düsseldorf, Germany, September 1-5, 2004. Autoimmun Rev. 2005;4(1):66–78.
Blake SC, Daniel BS. Cutaneous lupus erythematosus: a review of the literature. Int J Women’s Dermatol. 2019;5(5):320–9.
Kuhn A, Landmann A, Wenzel J. Advances in the treatment of cutaneous lupus erythematosus. Lupus. 2016;25(8):830–7.
Chasset F, Francès C. Current concepts and future approaches in the treatment of cutaneous lupus Erythematosus: a comprehensive review. Drugs. 2019;79:1199–215.
Kuhn A, Aberer E, Bata-Csörgő Z, Caproni M, Dreher A, Frances C, et al. S2k guideline for treatment of cutaneous lupus erythematosus – guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV). J Eur Acad Dermatol Venereol. 2017;31(3):389–404.
Klebes M, Wutte N, Aberer E. Dapsone as second-line treatment for cutaneous lupus Erythematosus? A retrospective analysis of 34 patients and a review of the literature. Dermatology. 2016;232(1):91–6.
Helton DR, Osborne DW, Pierson SK, Buonarati MH, Bethem RA. Pharmacokinetic profiles in rats after intravenous, oral, or dermal administration of dapsone. Drug Metab Dispos. 2000;28(8):925–9.
Osborne DW. Diethylene glycol monoethyl ether: an emerging solvent in topical dermatology products. J Cosmet Dermatol. 2011;10(4):324–9.
Thiboutot DM, Willmer J, Sharata H, Halder R, Garret S. Pharmacokinetics of Dapsone gel, 5% for the treatment of acne vulgaris. Clin Pharmacokinet. 2012;46(8):697–712.
Jarrat MT, Jones TM, Chang-Lin J-E, Tong W, Berk DR, Lin V, et al. Safety and pharmacokinetics of once-daily Dapsone gel, 7.5% in patients with moderate acne vulgaris patients with moderate acne vulgaris. J Drugs Dermatol. 2016;15(10):1250–9.
Del Rosso JQ, Kircik L, Gallagher CJ. Comparative efficacy and tolerability of dapsone 5% gel in adult versus adolescent females with acne vulgaris. J Clin Aesthet Dermatol. 2015;8(1):31–7.
Eichenfield LF, Lain T, Frankel EH, Jones TM, Chang-Lin J-E, Berk DR, et al. Efficacy and safety of once-daily Dapsone gel, 7.5% for the treatment of adolescents and adults with acne vulgaris: second of two identically designed, large, multicenter, randomized, vehicle-controlled trials. J Drugs Dermatol. 2016;15(8):962–9.
Alexis AF, Burgess C, Callender VD, Herzog JL, Roberts WE, Schweiger ES, et al. The efficacy and safety of topical Dapsone gel, 5% for the treatment of acne vulgaris in adult females with skin of color. J Drugs Dermatol. 2016;15(2):197–204.
Lucky AW, Maloney JM, Roberts J, Taylor S, Jones T, Ling M, et al. Dapsone gel 5% for the treatment of acne vulgaris: safety and efficacy of long-term (1 year) treatment. J Drugs Dermatol. 2007;6(10):981–7.
Lynde CW, Andriessen A. Cohort study on the treatment with Dapsone 5% gel of mild to moderate inflammatory acne of the face in women. Skinmed. 2014;12(1):15–21.
Stockton TC, Tanghetti EA, Lain E, Zeichner JA, Alvandi N. Clinical experience with once-daily Dapsone gel, 7.5% monotherapy in patients with acne vulgaris. J Drugs Dermatol. 2018;17(6):602–8.
Taylor SC, Cook-Bolden FE, McMichael A, Downie JB, Rodriguez DA, Alexis AF, et al. Efficacy and safety of topical Dapsone gel 7.5% for treatment of acne vulgaris by Fitzpatrick skin type. J Drugs Dermatol. 2018;17(2):160–7.
Draelos ZD, Rodriguez DA, Kempers SE, Bruce S, Peredo MI, Downie J, et al. Treatment response with once-daily topical Dapsone gel, 7.5% for acne vulgaris: subgroup analysis of pooled data from two randomized, double-blind study. J Drugs Dermatol. 2017;16(6):591–8.
Del RJQ, Kircik L, Tanghetti E. Management of truncal acne vulgaris with topical Dapsone 7.5% gel. J Clin Aesthet Dermatol. 2018;11(8):45–50.
Piette WW, Taylor S, Pariser D, Jarratt M, Sheth P, Wilson D. Hematologic safety of dapsone gel, 5%, for topical treatment of acne vulgaris. Arch Dermatol. 2008;144(12):1564–70.
Webster GF. Is topical Dapsone safe in glucose-6-phosphate dehydrogenase-deficient and sulfonamide-allergic patients? J Drugs Dermatol. 2010;9(5):532–6.
Tanghetti EA, Harper J, Baldwin HE, Kircik LH, Bai Z, Alvandi N. Once-daily topical Dapsone gel, 7.5%:effective for acne vulgaris regardless of baseline lesion count, with superior efficacy in females. J Drugs Dermatol. 2018;17(11):1192–8.
Warner KS, Parashar AP, Swaminathan V, Bhatt V. Topical dapsone and dapsone/adapalene compositions and methods for use thereof. United States: United States Patent Office; US 2014/0142184 A1, 2014. p. 12.
Kircik LH. Use of Dapsone 5% gel as maintenance treatment of acne vulgaris following completion of oral doxycycline and Dapsone 5% gel combination treatment. J Drugs Dermatol. 2016;15(2):191–5.
Swartzentruber GS, Yanta JH, Pizon AF. Methemoglobinemia as a complication of topical Dapsone. N Engl J Med. 2015;372:491–2.
Graff DM, Bosse GM, Sullivan J. Case report of methemoglobinemia in a toddler secondary to topical dapsone exposure. Pediatrics. 2016;138(2).
Yale S, Stefanko N, McCarthy P, McFadden V, McCarthy J. Severe methemoglobinemia due to topical dapsone misuse in a teenage girl. Pediatr Dermatol. 2020;37(2):377–8.
Osborne DW. Composition and methods for topical application of therapeutic agents. United States: United States Patent Office; 5,863,560, 1999. p. 9.
Osborne DW. Compositions and methods for topical application of therapeutic agents. United States: United States Patent Office; 6,060,085, 2000. p. 9.
Osborne DW. Topical dapsone for the treatment of acne. Canada: Canadian Intelectual Property Office; 2,776,702, 2002. p. 14.
Warner KS, Parashar AP, Swaminathan V, Bhatt V, Kaoukhov A. Methods of treatment of acne vulgaris using topical dapsone compositions. United States: United States Patent Office; US 2017/0119703 A1, 2017. p. 28.
Brewster ME, Loftsson T. Cyclodextrins as pharmaceutical solubilizers. Adv Drug Deliv Rev. 2007;59(7):645–66.
Shamma RN, Salah Ad-din I, Abdeltawab NF. Dapsone- gel as a novel platform for acne treatment: in vitro evaluation and in vivo performance and histopathological studies in acne infected mice. J Drug Deliv Sci Technol. 2019;54(101238):1–7.
Kataoulis AC, Kakepis EM, Kintziu H, Kakepis ME, Stavrianeas NG. Comedogenicity of cosmetics: a review. J Eur Acad Dermatol Venereol. 1996;7(2):115–9.
Wohlrab J, Michael J. Dapsone for topical use in extemporaneous preparations. J Ger Soc Dermatol. 2018;16(1):34–40.
Marzuki NHC, Wahab RA, Hamid MA. An overview of nanoemulsion: concepts of development and cosmeceutical applications. Biotechnol Biotechnol Equip. 2019;33(1):779–97.
De A BVR, Simon A, ARC S, Cabral LM, de Sousa VP. Nanoemulsion containing dapsone for topical administration: a study of in vitro release and epidermal permeation. Int J Nanomedicine. 2013;8:535–44.
Mahore JG, Suryawashi SD, Shirolkar SV, Deshkar SS. Enhancement of percutaneous delivery of Dapsone by microemulsion gel. J Young Pharm. 2017;9(4):507–12.
Ranjbar M, Khazaeli P, Pardakhty A, Tahamipour B, Amanatfard A. Preparation of polyacrylamide/polylactic acid co-assembled core/shell nanofibers as designed beads for dapsone in vitro efficient delivery. Artif Cells, Nanomed Biotechnol. 2019;47(1):917–26.
Wissing SA, Kayser O, Müller RH. Solid lipid nanoparticles for parenteral drug delivery. Adv Drug Deliv Rev. 2004;56(9):1257–72.
Naseri N, Valizadeh H, Zakeri-Milani P. Solid lipid nanoparticles and nanostructures lipid carriers structure, Preparation and Application. Adv Pharm Bull. 2015;5(3):305–13.
Deshkar SS, Bhalerao SG, Jadhav MS, Shirolkar SV. Formulation and optimization of topical solid lipid nanoparticles based gel of Dapsone using design of experiment. Pharm Nanotechnol. 2018;6(4):264–75.
Fang C-L, A Alsuwayeh S, Fang J-Y. Nanostructured lipid carriers (NLCs) for drug delivery and targeting. Recent Pat Nanotechnol. 2013;7(1):41–55.
Elmowafy M, Shalaby K, Ali HM, Alruwaili NK, Salama A, Ibrahim MF, et al. Impact of nanostructured lipid carriers on dapsone delivery to the skin: in vitro and in vivo studies. Int J Pharm. 2019;572(118781):1–11.
Mora-Huertas CE, Fessi H, Elaissari A. Polymer-based nanocapsules for drug delivery. Int J Pharm. 2010;385(1–2):113–42.
Cé R, Marchi JG, Bergamo VZ, Fuentefria AM, Lavayen V, Guterres SS, et al. Chitosan-coated dapsone-loaded lipid-core nanocapsules: growth inhibition of clinical isolates, multidrug-resistant Staphylococcus aureus and Aspergillus ssp. Colloids Surf A Physicochem Eng Asp. 2016;511:153–61.
Pereira RL, Leites FI, Paese K, Sponchiado RM, Michalowski CB, Guterres SS, et al. Hydrogel containing adapalene- and dapsone-loaded lipid-core nanocapsules for cutaneous application: development, characterization, in vitro irritation and permeation studies. Drug Dev Ind Pharm. 2016;46(12):2001–8.
Meraj Anjum M, Kanoujia J, Parashar P, Arya M, Yadav AK, Saraf SA. Evaluation of a polymer-lipid-polymer system utilising hybrid nanoparticles of dapsone as a novel antiacne agent. Curr Drug Ther. 2016;11(2):86–100.
Nvs M. Niosomes: a novel drug delivery system. Int J Res Pharm Chem. 2011;1(3):498–511.
Hatem AS, Fatma MM, Amal KH, Hossam MA-W, Maha HR. Dapsone in topical niosomes for treatment of acne vulgaris. Afr J Pharm Pharmacol. 2018;12(18):221–30.
Aflatoonian M, Fekri A, Rahnam Z, Khalili M, Pardakhti A, Khazaeli P, et al. The efficacy of combined topical niosomal dapsone gel and intralesional injection of meglumine antimoniate in comparison with intralesional meglumine antimoniate and cryotherapy in the treatment of cutaneous leishmaniasis. J Pakistan Assoc Dermatologists. 2016;26(4):353–60.
Fekri A, Rahnama Z, Khalili M, Dookhani AP, Khazaeli P, Beigi KB. The efficacy of co-administration of topical niosomal dapsone gel and intralesional injection of glucantime in cutaneous leishmaniasis in comparison with cryotherapy plus intralesional injection of glucantime. J Kerman Univ Med Sci. 2015;22(2):117–32.
Dragicevic N, Verma DD, Fahr A. Invasomes: vesicles for enhanced skin Delivery of drugs. In: Dragicevic N, Maibach H, editors. Percutaneous penetration enhancers chemical methods in penetration enhancement. Berlin, Heidelberg: Springer; 2016. p. 77–92.
El-Nabarawi MA, Shamma RN, Farouk F, Nasralla SM. Dapsone-loaded invasomes as a potential treatment of acne: preparation, characterization, and in vivo skin deposition assay. AAPS PharmSciTech. 2018;19(5):2174–84.
El-Nabarawi MA, Shamma RN, Farouk F, Nasralla SM. Bilosomes as a novel carrier for the cutaneous delivery for dapsone as a potential treatment of acne: preparation, characterization and in vivo skin deposition assay. J Liposome Res. 2020;30(1):1–11.
Garg G, Saraf S, Saraf S. Cubosomes: an overview. Biol Pharm Bull. 2007;30(2):350–3.
Nithya R, Jerold P, Siram K. Cubosomes of dapsone enhanced permeation across the skin. J Drug Deliv Sci Technol. 2018;48(August):75–81.
Pelikh O, Stahr PL, Huang J, Gerst M, Scholz P, Dietrich H, et al. Nanocrystals for improved dermal drug delivery. Eur J Pharm Biopharm. 2018;128:170–8.
Zhai X, Lademann J, Keck CM, Müller RH. Nanocrystals of medium soluble actives - novel concept for improved dermal delivery and production strategy. Int J Pharm. 2014;470(1–2):141–50.
Vidlářová L, Romero GB, Hanuš J, Štěpánek F, Müller RH. Nanocrystals for dermal penetration enhancement - effect of concentration and underlying mechanisms using curcumin as model. Eur J Pharm Biopharm. 2016;104:216–25.
Lademann J, Richter H, Schanzer S, Knorr F, Meinke M, Sterry W, et al. Penetration and storage of particles in human skin: perspectives and safety aspects. Eur J Pharm Biopharm. 2011;77(3):465–8.
Zhai X, Lademann J, Keck CM, Müller RH. Dermal nanocrystals from medium soluble actives - physical stability and stability affecting parameters. Eur J Pharm Biopharm. 2014;88(1):85–91.
Müller RH, Gohla S, Keck CM. State of the art of nanocrystals - special features, production, nanotoxicology aspects and intracellular delivery. Eur J Pharm Biopharm. 2011;78(1):1–9.
Badilli U, Gumustas B, Uslu B, Ozkan SA. Lipid-based nanoparticles for dermal drug delivery. In: Grumezescu A, editor. Organic materials as smart nanocarriers for drug delivery. Cambridge: William Andrew; 2018. p. 369–413.
Lademann J, Knorr F, Richter H, Jung S, Meinke MC, Rühl E, et al. Hair follicles as a target structure for nanoparticles. J Innov Opt Health Sci. 2015;8(4):1–8.
Lademann J, Richter H, Teichmann A, Otberg N, Blume-Peytavi U, Luengo J, et al. Nanoparticles - an efficient carrier for drug delivery into the hair follicles. Eur J Pharm Biopharm. 2007;66(2):159–64.
Patzelt A, Richter H, Knorr F, Schäfer U, Lehr CM, Dähne L, et al. Selective follicular targeting by modification of the particle sizes. J Control Release. 2011;150(1):45–8.
Mangelsdorf S, Vergou T, Sterry W, Lademann J, Patzelt A. Comparative study of hair follicle morphology in eight mammalian species and humans. Skin Res Technol. 2014;20(2):147–54.
Kartha VB, Patel ND, Venkateswaran S. Laser Raman spectroscopic studies on the interaction of drug Dapsone with model membranes. J Chem Sci. 1990;102(5):697–703.
Panicker L. Influence of the leprosy drug, dapsone on the model membrane dipalmitoyl phosphatidylethanolamine. Thermochim Acta. 2006;447(2):123–30.
Mittal A, Raber AS, Schaefer UF, Weissmann S, Ebensen T, Schulze K, et al. Non-invasive delivery of nanoparticles to hair follicles: A perspective for transcutaneous immunization. Vaccine. 2013;31(34):3442–51.
Farjadian F, Ghasemi A, Gohari O, Roointan A, Karimi M, Hamblin MR. Nanopharmaceuticals and nanomedicines currently on the market: Challenges and opportunities. Vol. 14. Nanomedicine. 2019:93–126.
ACKNOWLEDGMENTS AND DISCLOSURE
Authors thank the Brazilian governmental agencies CNPq/MCTI (Universal 01/2016 - Grant number: 408229/2016-0) and CAPES/MEC for the financial support and fellowships, respectively. GSR would like to specifically thank CAPES for the fellowship PDEE PRINT-CAPES/UFSC call 06/PGFAR/2019. Declarations of Interest: None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
ǂ The patents CA 2,776,702 (98) and US 2017/0119703 A1 (99) also mention the preparation of DAP formulations other than gels, for instance suspension, cream, liquid, paste, lotion, nanoemulsion, microemulsion, reverse emulsion, liposomal cream and ointment.
Rights and permissions
About this article
Cite this article
Schneider-Rauber, G., Argenta, D.F. & Caon, T. Emerging Technologies to Target Drug Delivery to the Skin – the Role of Crystals and Carrier-Based Systems in the Case Study of Dapsone. Pharm Res 37, 240 (2020). https://doi.org/10.1007/s11095-020-02951-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02951-4