Abstract
Studies of active drug-excipient compatibility represent an important phase in the preformulation stage of the development of all dosage forms. For the development of conjugation estrogens and medroxyprogesterone acetate (MPA) double-layer tablets, techniques of thermal, isothermal stress testing (IST), and molecular vibrational spectroscopy analysis were performed to access the compatibility. Differential scanning calorimetry (DSC) studies were used as an important and complementary tool during preformulation to determine drug-excipient compatibility. On the basis of DSC results, MPA was found to be compatible with polyethylene glycol 6000. However, the results of Raman and IST studies showed that all the excipients defined in the prototype formula were found to be compatible with MPA. Overall, the compatibility of selected excipients with MPA was successfully evaluated using a combination of thermal and IST methods, and the formulations developed using the compatible excipients were found to be stable.
Similar content being viewed by others
Introduction
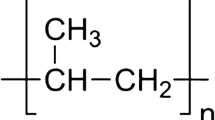
Medroxyprogesterone acetate (MPA) is a steroidal progestin, a synthetic variant of the human hormone progesterone [1, 2]. It is used as a contraceptive in hormone replacement therapy and for the treatment of endometriosis as well as several other indications. The chemical structure of MPA that correspond to pregn-4-ene-3,20-dione,17-(acetyloxy)-6-methyl-(6α)-17-hydroxy-6α-methylpregn-4-ene-3,20-dione acetate is given in (Fig. 1). MPA is also prescribed in combination with an estrogen to prevent endometrial hyperplasia in postmenopausal women who are undergoing hormone replacement therapy. As progesterone (the hormone made by the human body) could not be taken orally before, the process of micronization was developed. Our company investigates a new dosage form of conjugation estrogens and MPA double-layer tablets for better absorption. This article is to study on assessing the compatibility of MPA with some currently employed pharmaceutical excipients.
The layered tablet concept has been utilized to develop controlled-release formulations [3–8]. Such a tablet is considered as a biphasic delivery system that is designed to release the drug at two different rates and is usually composed of a fast-release layer combined with single [3–6] or double sustained-release layers [7, 8]. Generally, conventional controlled-release dosage forms delay the release of drugs and do not provide a rapid onset of action after oral administration [9, 10]. Hence, the conjugation estrogens and MPA double-layer tablets pharmacokinetic advantage over conventional controlled-release dosage forms as the drug is quickly released from the fast-release layer leading to rapid rise of drug plasma concentration followed by continuation of drug release from the sustained-release layer. This release pattern is required for successful treatment in many therapies.
The potential physical and chemical interactions and incompatibilities of pharmaceutical excipients with different active pharmaceutical ingredients in solid dosage forms can affect the chemical nature, the stability, and bioavailability of drugs and, consequently, their therapeutic efficacy and safety [11–18]. In recent years, applications of thermal analytical techniques at the preformulation stage of development of solid dosage forms have increased immensely. In particular, differential scanning calorimetric (DSC) has been proposed as a rapid method of evaluating any physicochemical interactions between components of the formulation and, therefore, selecting suitable compatible excipients. The main benefit of DSC is its ability to quickly screen potential excipients for incompatibilities derived from the appearance, shifts, or disappearances of peaks or variations in the corresponding ΔH (enthalpy of transition). However, DSC results should be interpreted carefully because of the requirement of high temperature conditions and the lack of moisture in conducting the DSC experiments. Conclusions based on the DSC results alone can be often misleading and inconclusive [13–16].
Isothermal stress testing (IST) is another commonly used method for evaluating the drug-excipient compatibility. In this approach, the drug-excipient with or without moisture at a temperature (>50 °C) for a specific period of time to accelerate drug degradation and interaction. The samples are then visually observed for any type of change in physical appearance, and the drug content, along with any degradants, is determined quantitatively. Although more useful, the disadvantage with this method is that it is time consuming and requires quantitative analysis using HPLC [12, 16]. Therefore, DSC should be used in combination with IST and molecular vibrational spectroscopy to evaluate compatibility of drugs with selected excipients [18–21].
Molecular vibrational spectroscopy spectra are also used to confirm any type of physical interaction between the drug and the excipient. In this study, the molecular vibrational spectroscopy of the pure drug was compared with the drug-excipient mixture, as the comparison could further verify drug-excipient compatibility.
Experimental
Materials
MPA and the following excipients were purchased from commercial sources. MPA (Zhejiang Xianju Pharmaceutical Co., Ltd, China), hydroxy propyl methyl cellulose (HPMC) (methocel E15, Dow, USA), PEG-6000 (Sasol, Germany), crosslinking povidone (PVPP) (XL, BASF, Germany), lactose monohydrate (Foremost, USA), magnesium stearate (Peter Greven, Netherlands), microcrystalline cellulose (MCC) (Avicel PH-301, FMC, USC), Calcium Phosphate Tribasic (Beijing Fengli Jingqiu Commerce and Trade Co., Ltd, China), and Acetonitrile HPLC grade (Tedia, USA) were used for preparing mobile phase for HPLC analysis; water used throughout the HPLC analysis was prepared by water purifier (ATC-2001-P, Aquapro, China).
Differential scanning calorimetry
A differential scanning calorimeter (DSC 821e, Mettler Toledo, Switzerland) was used to study the thermal analysis of drug-excipient compatibility. Excipients that were expected to be used in the development of formulation (sustained-release matrix, filling agent, disintegrating agent, adhesive, lubricant, hardening) and the appropriate ratio were selected for the present study; binary mixtures of drug and selected excipients (all passed through 80-mesh sieve) were weighed directly in the pierced DSC aluminum pan (Table 1). The drug-excipients mixture was scanned in the temperature range of 40–400 °C under an atmosphere of nitrogen. The heating rate was 10 °C min−1 and the obtained curves were observed for any type of interaction.
Raman spectroscopy
Raman spectra of drug and drug-excipient blends were recorded on an DXR raman microscope (DXR 532 nm, Thermo, USA) in the range of 40–4,000 cm−1.
IR spectroscopy
IR spectra of drug, and the blend of drug and selected excipient were recorded on a FTIR spectrophotometer (FTIR-8400S, Shimadzu, Japan) in the range of 4,000–500 cm−1 using potassium bromide disks.
Isothermal stress testing
Based on the DSC results and initial formulation studies, list of excipients and the expected range to be used in the formulation was narrowed down. In IST, samples of drug and different excipients (Table 2) were weighed directly in 5-mL glass vials (n = 3). Mixing was done on a cyclo mixer for 3 min, with 10 % w/w water in each of the vials, and the drug-excipient blend was further mixed with a glass capillary (both the ends of which were heat sealed). To prevent any loss of material, capillary was broken and left inside the vial. The glass vials were stored at 50 °C in a hot oven after Teflon sealing. Drug- excipient blends without added water and stored in refrigerator served as controls. The drug-excipient blends were periodically examined for any change in physical appearance. Samples were quantitatively analyzed using HPLC after 4 weeks of storage at above conditions.
For sample preparation, with 2 mL of methanol in each of the vials, the mixture was vortexed and transferred into 100 mL volumetric flask. Vials were rinsed twice with methanol and the volume made up. The samples were centrifuged and the supernatant was filtered through 0.22 μm nylon membrane filters. After appropriate dilutions, samples were analyzed using HPLC and drug content determined from the calibration curve was prepared within the expected range.
For the analysis of drug-excipient mixtures, Shimadzu HPLC system equipped with LC-20 AD pump, DGU-20A5R on-line degasser, SIL-20 A autoinjector, CTO-20 AD column oven, and SPD-M20A UV–Vis detector was utilized. Shimadzu CLASS-VP software (Version 5.03) was used for data acquisition and mathematical calculations. Chromatographic separation of MPA was performed on a C18 Spherisorb column (4.6 × 250 mm2; 5 μm particle size). Mobile phase used was acetonitrile–water in the ratio of 60:40 v/v at a flow rate of 1 mL min−1. Temperature of the column oven was maintained at 40 °C. All the samples (20 μl) were injected and analyzed at 240 nm using a UV detector. For peak purity testing, PDA detector in the range of 190–800 nm was used.
Formulation and stability study of tablets
The detail of the formulation development of the core tablets of MPA immediate release tablets is presented in Table 3. In brief, MPA immediate release tablets were prepared by wet granulation using single stroke tablet punching machine (XYP-5B, Leimai, China) fitted with 7-mm standard concave punches. MPA and all the excipients were mixed and passed through 80-mesh sieve and they were mixed for 20 min in a polyethylene bag. Granules were prepared by kneading with 95 % ethanol and kept for air drying in tray dryer at 45 °C for 4 h. The dried granules were passed through 26-mesh sieve to get uniform granules. These sized granules were then blended with magnesium stearate (80-mesh passed) and compressed into tablets having an average mass of 75 mg.
For assay, one accurately weighed tablet (n = 5) was dissolved in 100 mL of methanol. The samples were sonicated (Ultra sonic water bath, SB5200D, Ningbo Scientz Biotechnology Co., LTD, China) for 30 min, after which they were filtered through 0.45 μm nylon membrane filter. The filtered solutions, after appropriate dilution with methanol, were analyzed by HPLC.
Drug release testing of the formulations (n = 6) was carried out using USP-II dissolution apparatus (ZRS-6G, TDTF, China) at 50 rpm; 0.54 % sodium lauryl sulfate (SLS) (900 mL) maintained at 37 ± 0.5 °C was used as dissolution medium. The samples (5 mL) were withdrawn at predetermined time (5, 10, 20, 30, and 45 min) [22] and replaced with an equivalent amount of fresh medium. The samples were filtered through 0.22 μm nylon membrane and analyzed by HPLC at 240 nm. The cumulative percent drug release was plotted against time to determine the release profile.
MPA tablets were kept in open petridish and stored in stability chamber maintained at 40 ± 2 °C and 75 ± 5 % RH. The samples were withdrawn periodically and subjected to assay and dissolution study.
Results and discussion
Drug-excipient compatibility testing
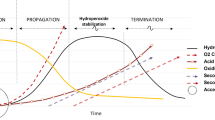
DSC curves of drug and drug-excipient mixtures are shown in Figs. 2, 3, 4, 5, 6, 7, and 8a, and corresponding peak, onset transition temperature, and enthalpy values (ΔH f) of MPA with various excipient mixtures are summarized in Table 1.
The DSC curve of MPA exhibited one sharp endothermic peak at 206.12 °C, caused by the melting of MPA, and the heat of transition (ΔH f ) was 33.09 J g−1 K−1. Chemical decomposition was not detected after the melting; MPA, therefore, has good thermal stability and does not contain crystal water. The endothermic peak of the drug was well retained in majority of cases. However, in some combinations there were slight changes in peak temperature and peak shape, which might be due to mixing of excipients with the drug as this reduces the purity of component in mixtures [23, 24].
The Raman spectra of drug and drug-excipient mixtures are shown in Figs. 2, 3, 4, 5, 6, 7, and 8b. We can determine the compatibility in accordance with the changes of main bands.
In the DSC curve of HPMC, a broad endotherm peak at 65.70 °C, due to evaporation of adsorbed moisture, is observed in (Fig. 2a). The melting endotherm of drug was present at 206.69 °C with a little change in ΔH f value (32.87 J g−1 K−1) in the DSC trace of MPA-HPMC mixture, which ruled out any incidence of incompatibility. Also, the Raman spectrum of mixture of MPA and HPMC showed the presence of characteristic bands of MPA (1,605 and 1,672 cm−1) and there were small shifts (1,606.92 and 1,673.74 cm−1) in (Fig. 2b). Thus, it was concluded that MPA is compatible with HPMC.
In the DSC curve of PEG-6000, a sharp endothermic peak at 62.35 °C was retained well in MPA and PEG-6000 (66.31 °C). However, the endothermic of MPA was completely missing in the DSC trace of mixture (Fig. 3a), from this, results point toward some incompatibility between MPA and PEG-6000. It could be because of melting of PEG-6000 and partial dissolution of drug in the molten excipient [25], we have discussed it in the part of conclusions. Drug formulation development and initial trials were taken with PEG-6000. Later on, it was observed that PEG-6000 is easy to cause the sticking phenomenon in the tablet. Therefore, it was not used in the formulation. The Raman spectrum of MPA-PEG-6000 mixture showed the presence of characteristic bands of MPA (1,606.72 and 1,672.06 cm−1) in (Fig. 3b). MPA-PEG-6000 mixture was also subjected to the IR studies and its spectrum was compared with the IR spectra of MPA. The characteristic bands of MPA (Fig. 9) were observed at 1,727 cm−1 (–COOCH3), 1,604 cm−1 (COCH3), and 1,674 cm−1 (–C=O). However, IR spectrum of MPA-PEG-6000 mixture is shown in Fig. 10, and the characteristic bands were observed at 1,728 cm−1 (–COOCH3), 1,605 cm−1 (COCH3), and 1,670 cm−1 (–C=O), which correspond to the structure of MPA. The results confirmed that there is no chemical interaction between MPA and PEG-6000. Thus, any change in the structure of MPA was ruled out and it was concluded that there is no chemical incompatibility between MPA and PEG-6000.
In the DSC curve of PVPP, a broad endothermic peak at 67.72 °C, due to evaporation of adsorbed moisture, is observed in (Fig. 4a). The curve of MPA-PVPP mixture showed an sharp peak of MPA at 207.20 °C and the ΔH f value (37.81 J g−1 K−1); the DSC results indicate that MPA is compatible with PVPP. Also, the Raman spectrum of mixture of MPA and PVPP showed the presence of characteristic bands of MPA (1,606.74 and 1,673.70 cm−1) and there are no new bands in (Fig. 4b). Thus, it was concluded that MPA is compatible with PVPP.
The DSC scan of lactose showed 147.34 °C (corresponding to dehydration of bound water), and a small peak at 181.39 °C (crystalline transition) [18], 218.10 °C (melting point). The DSC curve of MPA in the presence of lactose is shown in (Fig. 5a). DSC trace of MPA-lactose mixture showed two endothermic peaks at (208.29 °C with accompanying ΔH f of 29.79 J g−1 K−1) and 216.48 °C, which suggested that there was some incompatibility between lactose and MPA. However, Raman spectrum of MPA-lactose mixture showed the presence of characteristic band of MPA (1,605.23 and 1,672.20 cm−1) confirming that there was no change in the drug structure (Fig. 5b). Therefore, based on above results, it was concluded that MPA is compatible with lactose.
In DSC trace of magnesium stearate, an endothermic peak was observed at 91.78 °C (Fig. 6a). A small peak was also present at 115.62 °C, which might be due to palmitate impurity [26]. The curve of MPA and magnesium stearate mixture showed shifting of the peak of MPA to a lower temperature (203.18 °C with accompanying ΔH f of 34.88 J g−1 K−1). This kind of phenomenon may be due to purity of each component. This result suggests that there was no interaction between magnesium stearate and MPA. Also, the Raman spectrum of mixture of MPA and magnesium stearate showed the presence of characteristic bands of MPA (1,606.62 and 1,673.62 cm−1) and there are no new bands (Fig. 6b). Thus, it was concluded that MPA is compatible with magnesium stearate.
A sharp melting endotherm was observed at 66.06 °C in the DSC trace of MCC (Fig. 7a). In the case of MPA-MCC mixture, there was a sharping of melting endotherm of MCC at 58.45 °C. The melting endotherm of MPA was well retained in the DSC trace of MPA-MCC mixture (208.58 °C with accompanying ΔH f of 37.24 J g−1 K−1). In Raman spectra of MPA-MCC mixture, bands corresponding to MPA (1,606.662 and 1,673.14 cm−1) were observed without any new bands (Fig. 7b). It was concluded that MPA is compatible with MCC.
In the DSC curves of calcium phosphate tribasic, no peaks were observed in the range of 40–400 °C (Fig. 8a). However, the endothermic peak of MPA was well preserved at 206.23 °C with ΔH f of 30.85 J g−1 K−1 in the DSC curve of MPA-calcium phosphate tribasic mixture. It was concluded that MPA is compatible with calcium phosphate tribasic. Also, the bands corresponding to MPA were present in the Raman spectrum of both the mixtures, confirming that there was no change in the structure of MPA (1,606.47 and 1,673.44 cm−1) in (Fig. 8b). On the basis of above results, it was concluded that MPA is compatible with calcium phosphate tribasic.
Results of analysis of IST samples are shown in Table 2; the changes of drug content could reveal the compatibility of drug-excipient. There was no significant interaction between MPA and individual excipients. Moreover, the mixture of MPA and individual excipients was compared with that of pure MPA during the analysis of IST sample by HPLC, it was found that the retention time shown in (Fig. 11) remained unchanged. It indicates that MPA was not degraded in drug-excipients mixture of IST sample. Therefore, the IST results further verify that all the selected excipients are compatible with MPA.
Formulation development and stability studies
Excipients defined in the prototype formula were used for formulation development. The optimized formulation was evaluated after 12 months of storage at accelerated stability conditions (40 °C and 75 % RH), results of which are shown in (Fig. 12). It is evident that the formulation is having good stability in terms of both drug content and dissolution stability. Release profile was similar after stability studies. Based on the results, it can be concluded that the formulations are stable after 12 months of storage at accelerated stability conditions.
Conclusions
The results confirmed that DSC could be used as a rapid method to evaluate the compatibility between a drug and an excipient. However, the IST techniques after storage of a mixture of MPA and individual excipients under stressed conditions should also be adopted in conjunction with DSC and Raman studies to reach any definite conclusion. From the results of the DSC studies an interaction was suspected between MPA and PEG6000. However, based on the results of molecular vibrational spectroscopy and IST study, the possibility of incompatibility between MPA and PEG-6000 was ruled out. In this study, the DSC analysis along with molecular vibrational spectroscopy and HPLC analysis (for IST studies) were successfully employed to assess the compatibility of MPA with the excipients used in the development of immediate release tablet formulation.
To use the results of this study, immediate release formulations were developed using the excipients found to be compatible with MPA. The optimized formulation was found to be stable after 12 months of accelerated stability studies, thus, validating the claims that the above methods were successfully used to assess the compatibility between MPA and excipients.
References
Hall JA, Morton I (1999). Concise dictionary of pharmacological agents: properties and synonyms. Springer, New York, p. 173. ISBN 978-0-7514-0499-9.
MedroxyPROGESTERone: Drug information provided by Lexi-Comp. Merck Manual. 2009. Retrieved 8 July 2010.
Patra CN, Kumar AB, Pandit HK, Singh SP. Design and evaluation of sustained release bilayer tablets of propranolol hydrochloride. Acta Pharm. 2007;57:479–89.
Uekama K, Matsubara K, Abe K, Horiuchi Y, Hirayamma F, Suzuki N. Design and in vitro evaluation of slow-release dosage form of piretanide: utility of beta-cyclodextrin: cellulose derivative combination as a modified-release drug carrier. J Pharm Sci. 1990;79:244–8.
Bruni G, Berbenni V, Milanese C, Girella A, Marini A. Drug-excipient compatibility studies in binary and ternary mixtures by physicochemical techniques. J Therm Anal Calorim. 2010;102:193–210.
Ganesh G, Ramadoss A, Kannan PS, SubbiahPandi A. A Crystal growth, structural, thermal, and dielectric characterization of Tutton salt (NH4)2Fe(SO4)2·6H2O crystals. J Therm Anal Calorim. 2013;112:547–54.
Yan G, Li H, Zhang R, Ding D. Preparation and evaluation of a sustained-release formulation of nifedipine HPMC tablets. Drug Dev Ind Pharm. 2000;26:681–6.
Fassihi RA, Ritschel WA. Multiple-layer, direct-compression, controlled-release system: in vitro and in vivo evaluation. J Pharm Sci. 1993;82:750–4.
Lopes CM, Sousa Lobo JM, Pinto JF, Costa PC. Compressed matrix core tablet as a quick/slow dual-component delivery system containing ibuprofen. AAPS PharmSciTech. 2007;8:E76.
Maggi L, Machiste EO, Torre ML, Conte U. Formulation of biphasic release tablets containing slightly soluble drugs. Eur J Pharm Biopharm. 1999;48:37–42.
Ford JL, Timmins P, In: Rubinstein MH, editor. Pharmaceutical thermal analysis: techniques and applications. Chichester: Ellis Horwood; 1989. p. 201–237.
Wang Z, Horikawa T, Hirayama F, Uekama K. Design and invitro evaluation of a modified-release oral dosage form of nifedipine by hybridization of hydroxypropyl-beta-cyclodextrin and hydroxypropylcellulose. J Pharm Pharmacol. 1993;45:942–6.
Sims JL, Carreira JA, Carrier DJ, Crabtree SR, Easton L, Hancock SA, Simcox CE. A New approach to accelerated drug-excipient compatibility testing. Pharm Dev Technol. 2003;8:119–26.
Clas SD, Dalton CR, Hancock BC. Differential scanning calorimetry: applications in drug development. Pharm Sci Technol. 1999;3:311–20.
Giron D. Contribution of thermal methods and related techniques to the rational development of pharmaceuticals: part 2. Pharm Sci Technol. 1998;4:262–8.
Singh AV. A DSC study of some biomaterials relevant to pharmaceutical industry. J Therm Anal Calorim. 2013;112:791–3.
Vueba ML, Veiga F, Sousa JJ, Pina ME. Compatibility studies between ibuprofen or ketoprofen with cellulose ether polymer mixtures using thermal analysis. Drug Dev Ind Pharm. 2005;31:943–9.
Mura P, Faucci MT, Manderioli A, Bramanti G, Ceccarelli L. Compatibility study between ibuproxam and pharmaceutical excipients using differential scanning calorimetry, hot-stage microscopy and scanning electron microscopy. J Pharm Biomed Anal. 1998;18:151–63.
Botha SA, Lotter AP. Drug Dev Ind Pharm. 1989;15:415–26.
Mura P, Manderioli A, Bramanti G, Furlanetto S, Pinzauli S. Int J Pharm. 1995;119:71–9.
Bucci R, Magri AD, Magri AL. DSC in the chemical analysis of drugs. Determinations of diclofenac in pharmaceutical formations. J Therm Anal Calorim. 2000;61:369–76.
FDA/CDER (2007) Dissolution method—list of all drug in data base. US Food and Administration website. Accessed 22 December 2007.
Soares MFR, Soares-sobrinho JL, Silva KER, Alves LDS, Lopes PQ, Correia LP, Souza FS, Macedo RO, Rolim-Neto PJ. Thermal characterization of antimicrobial drug ornidazole and its compatibility in a solid pharmaceutical product. J Therm Anal Calorim. 2011;104:307–13.
Malan CEP, Villers MM, Lotter AP. J Pharm Biomed Anal. 1997;15:549–57.
Araujo AAS, Storpirtis S, Mercuri LP, Carvalho FMS, Filho MS, Matos JR. Int J Pharm. 2003;260:303–14.
Pani NR, Nath LK, Acharya S, Bhuniya B. Application of DSC, IST, and FTIR study in the compatibility testing of nateglinide with different pharmaceutical excipients. J Therm Anal Calorim. 2012;108:219–26.
Acknowledgements
This work has been supported by the National High Technology Research and Development Program of China (201291162) and the Fundamental Research Funds for the Central Universities (CXZZ12_0119).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gao, R., Sun, BW., Lin, J. et al. Compatibility of medroxyprogesterone acetate and pharmaceutical excipients through thermal and spectroscopy techniques. J Therm Anal Calorim 117, 731–739 (2014). https://doi.org/10.1007/s10973-014-3773-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-014-3773-8