Abstract
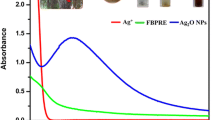
Dental caries and periodontal disease are widespread diseases for which microorganism infections have been identified as the main etiology. Silver nanoparticles (Ag Nps) were considered as potential control oral bacteria infection agent due to its excellent antimicrobial activity and non acute toxic effects on human cells. In this work, stable Ag Nps with different sizes (~5, 15 and 55 nm mean values) were synthesized by using a simple reduction method or hydrothermal method. The Nps were characterized by powder X-ray diffraction, transmission electron microscopy and UV–vis absorption spectroscopy. The antibacterial activities were evaluated by colony counting assay and growth inhibition curve method, and corresponding minimum inhibitory concentration (MIC) against five anaerobic oral pathogenic bacteria and aerobic bacteria E. coli were determined. The results showed that Ag Nps had apparent antibacterial effects against the anaerobic oral pathogenic bacteria and aerobic bacteria. The MIC values of 5-nm Ag against anaerobic oral pathogenic bacteria A. actinomycetemcomitans, F. nuceatum, S. mitis, S. mutans and S. sanguis were 25, 25, 25, 50 and 50 μg/mL, respectively. The aerobic bacteria were more susceptible to Ag NPs than the anaerobic oral pathogenic bacteria. In the mean time, Ag NPs displayed an obvious size-dependent antibacterial activity against the anaerobic bacteria. The 5-nm Ag presents the highest antibacterial activity. The results of this work indicated a potential application of Ag Nps in the inhibition of oral microorganism infections.





Similar content being viewed by others
References
Gaengler P, Markovic L, Norden D, et al. New insights in understanding dental caries and periodontal disease: the avalanche model. Health. 2009;1:263–8.
Bagramian RA, Garcia-Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. Am J Dent. 2009;22:3–8.
Qi XQ. 3th survey of oral health status of population in China. Beijing: People’s Medical Publishing House; 2008.
Marsh P, Martin MV, Lewis MAO. Oral microbiology. London: Churchill Livingstone; 2009.
Kolenbrander PE, Palmer RJ, Periasamy S, et al. Oral multispecies biofilm development and the key role of cell–cell distance. Nat Rev Microbiol. 2010;8:471–80.
Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369:51–9.
Love R, Jenkinson H. Invasion of dentinal tubules by oral bacteria. Crit Rev Oral Biol Med. 2002;13:171–83.
Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Res. 1986;50:353.
Zambon JJ. Actinobacillus actinomycetemcomitans in human periodontal disease. J Clin Periodontol. 1985;12:1–20.
Kinder SA, Holt SC. Localization of the Fusobacterium nucleatum T18 adhesin activity mediating coaggregation with Porphyromonas gingivalis T22. J Bacteriol. 1993;175:840–50.
Leistevuo J, Järvinen H, Sterblad M, et al. Resistance to mercury and antimicrobial agents in Streptococcus mutans isolates from human subjects in relation to exposure to dental amalgam fillings. Antimicrob Agents Chemother. 2000;44:456.
Espinosa-Cristóbal LF, Martínez-Castañón GA, Martínez-Martínez RE, et al. Antibacterial effect of silver nanoparticles against Streptococcus mutans. Mater Lett. 2009;63:2603–6.
Altman H, Steinberg D, Porat Y, et al. In vitro assessment of antimicrobial peptides as potential agents against several oral bacteria. J Antimicrob Chemother. 2006;58:198.
Rai MK, Deshmukh SD, Ingle AP, et al. Silver nanoparticles: the powerful nanoweapon against multidrug-resistant bacteria. J Appl Microbiol. 2012;112:841–52.
Kim JS, Kuk E, Yu KN, et al. Antimicrobial effects of silver nanoparticles. Nanomedicine. 2007;3:95–101.
Sondi I, Salopek-Sondi B. Silver nanoparticles as antimicrobial agent: a case study on E. coli as a model for Gram-negative bacteria. J Colloid Interface Sci. 2004;275:177–82.
Shahverdi AR, Fakhimi A, Shahverdi HR, et al. Synthesis and effect of silver nanoparticles on the antibacterial activity of different antibiotics against Staphylococcus aureus and Escherichia coli. Nanomedicine. 2007;3:168–71.
Jun BH, Byun JW, Kim JY, et al. Facile method of preparing silver-embedded polymer beads and their antibacterial effect. J Mater Sci. 2010;45:3106–8.
Rai M, Yadav A, Gade A. Silver nanoparticles as a new generation of antimicrobials. Biotechnol Adv. 2009;27:76–83.
Pal S, Tak YK, Song JM. Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A study of the gram-negative bacterium Escherichia coli. Appl Environ Microbiol. 2007;73:1712–20.
Yoon KY, Hoon Byeon J, Park JH, et al. Susceptibility constants of Escherichia coli and Bacillus subtilis to silver and copper nanoparticles. Sci Total Environ. 2007;373:572–5.
Martinez-Castanon GA, Nino-Martinez N, Martinez-Gutierrez F, et al. Synthesis and antibacterial activity of silver nanoparticles with different sizes. J Nanopart Res. 2008;10:1343–8.
Cao XL, Cheng C, Ma YL, et al. Preparation of silver nanoparticles with antimicrobial activities and the researches of their biocompatibilities. J Mater Sci Mater Med. 2010;21:2861–8.
Marius S, Lucian H, Marius M, et al. Enhanced antibacterial effect of silver nanoparticles obtained by electrochemical synthesis in poly(amide-hydroxyurethane) media. J Mater Sci Mater Med. 2011;22:789–96.
Hernández-Sierra JF, Ruiz F, Pena DC, et al. The antimicrobial sensitivity of Streptococcus mutans to nanoparticles of silver, zinc oxide, and gold. Nanomedicine. 2008;4:237–40.
Slenters TV, Hauser-Gerspach I, Daniels AU, et al. Silver coordination compounds as light-stable, nano-structured and anti-bacterial coatings for dental implant and restorative materials. J Mater Chem. 2008;18:5359–62.
Sadeghi R, Owlia P, Taleghani F, et al. An in vitro comparison between antimicrobial activity of nanosilver and chlorhexidine against Streptococus sanguis and Actinomyces viscosus. J Islamic Dent Assoc Iran. 2011;23:225–31.
Shrivastava S, Bera T, Roy A, et al. Characterization of enhanced antibacterial effects of novel silver nanoparticles. Nanotechnology. 2007;18:225103.
Li WR, Xie XB, Shi QS, et al. Antibacterial activity and mechanism of silver nanoparticles on Escherichia coli. Appl Microbiol Biotechnol. 2010;85:1115–22.
Lok CN, Ho CM, Chen R, et al. Proteomic analysis of the mode of antibacterial action of silver nanoparticles. J Proteome Res. 2006;5:916–24.
Liu J, Hurt RH. Ion release kinetics and particle persistence in aqueous nano-silver colloids. Environ Sci Technol. 2010;44:2169–75.
Sotiriou GA, Pratsinis SE. Antibacterial activity of nanosilver ions and particles. Environ Sci Technol. 2010;44:5649–54.
Xiu ZM, Zhang QB, Puppala HL, et al. Negligible particle-specific antibacterial activity of silver nanoparticles. Nano Lett. 2012;12:4271–5.
Spacciapoli P, Buxton D, Rothstein D, et al. Antimicrobial activity of silver nitrate against periodontal pathogens. J Periodontal Res. 2002;36:108–13.
Brandt O, Mildner M, Egger AE, et al. Nanoscalic silver possesses broad-spectrum antimicrobial activities and exhibits fewer toxicological side effects than silver sulfadiazine. Nanomedicine. 2012;8:478–88.
Acknowledgments
This work was supported by the Program for New Century Excellent Talents in University (NCET-09-0136), the Key Program of Hubei Provincial Department of Education (D20111510), the Outstanding Youth Science Foundation of Hubei Province (2009CDA075), Natural Science Foundation of Hubei Province (2011CDB219) and the International Cooperation Program of Hubei Province (2011BFA021).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, Z., Rong, K., Li, J. et al. Size-dependent antibacterial activities of silver nanoparticles against oral anaerobic pathogenic bacteria. J Mater Sci: Mater Med 24, 1465–1471 (2013). https://doi.org/10.1007/s10856-013-4894-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-013-4894-5