Abstract
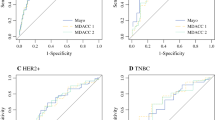
Optimization of axillary staging among patients converting from clinically node-positive disease to clinically node-negative disease through primary systemic therapy is needed. We aimed at developing a nomogram predicting the probability of positive axillary status after chemotherapy based on clinical/pathological parameters. Patients from study arm C of the SENTINA trial were included. Univariable/multivariable analyses were performed for 13 clinical/pathological parameters to predict a positive pathological axillary status after chemotherapy using logistic regression models. Odds ratios and 95%-confidence-intervals were reported. Model performance was assessed by leave-one-out cross-validation. Calculations were performed using the SAS Software (Version 9.4, SAS Institute Inc., Cary, NC, USA). 369 of 553 patients in Arm C were included in multivariable analysis. Stepwise backward variable selection based on a multivariable analysis resulted in a model including estrogen receptor (ER) status (odds ratio (OR) 3.916, 95% confidence interval (CI) 2.318–6.615, p < 0.001), multifocality (OR 2.106, 95% CI 1.203–3.689, p = 0.0092), lymphovascular invasion (OR 9.196, 95% CI 4.734–17.864, p < 0.001), and sonographic tumor diameter after PST (OR 1.034, 95% CI 1.010–1.059, p = 0.0051). When validated, our model demonstrated an accuracy of 70.2% using 0.5 as cut-point. An area under the curve of 0.81 was calculated. The use of individual parameters as predictors of lymph node status after chemotherapy resulted in an inferior accuracy. Our model was able to predict the probability of a positive axillary nodal status with a high accuracy. The use of individual parameters showed reduced predictive performance. Overall, tumor biology was the strongest parameter in our models.

Similar content being viewed by others
References
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14:500–515
Viehoff PB, Heerkens YF, Van Ravensberg CD, Hidding J, Damstra RJ, Ten Napel H et al (2015) Development of consensus International Classification of Functioning, Disability and Health (ICF) core sets for lymphedema. Lymphology 48:38–50
Mamounas EP (2015) Impact of neoadjuvant chemotherapy on locoregional surgical treatment of breast cancer. Ann Surg Oncol 22:1425–1433
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW et al (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305:569–575
Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G et al (2013) Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol 14:609–618
Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG et al (1997) Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol 15:2483–2493
Kuerer HM, Sahin AA, Hunt KK, Newman LA, Breslin TM, Ames FC et al (1999) Incidence and impact of documented eradication of breast cancer axillary lymph node metastases before surgery in patients treated with neoadjuvant chemotherapy. Ann Surg 230:72–78
Coutant C, Olivier C, Lambaudie E, Fondrinier E, Marchal F, Guillemin F et al (2009) Comparison of models to predict nonsentinel lymph node status in breast cancer patients with metastatic sentinel lymph nodes: a prospective multicenter study. J Clin Oncol 27:2800–2808
Boughey JC, Suman VJ, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B et al (2013) Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA 310:1455–1461
Caudle AS, Yang WT, Krishnamurthy S, Mittendorf EA, Black DM, Gilcrease MZ et al (2016) Improved axillary evaluation following neoadjuvant therapy for patients with node-positive breast cancer using selective evaluation of clipped nodes: implementation of targeted axillary dissection. J Clin Oncol 34:1072–1078
Diego EJ, McAuliffe PF, Soran A, McGuire KP, Johnson RR, Bonaventura M et al (2016) Axillary staging after neoadjuvant chemotherapy for breast cancer: a pilot study combining sentinel lymph node biopsy with radioactive seed localization of pre-treatment positive axillary lymph nodes. Ann Surg Oncol 23:1549–1553
Boughey JC, McCall LM, Ballman KV, Mittendorf EA, Ahrendt GM, Wilke LG et al (2014) Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (alliance) prospective multicenter clinical trial. Ann Surg 260:608–614
Acknowledgements
The SENTINA-study received financial and logistic support from AGO-B, Brustkrebs Deutschland and the German Breast Group (GBG).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors stated no potential conflicts of interest as to the content of the manuscript.
Ethical approval
The SENTINA trial was approved by the ethics committee of the University of Frankfurt.
Informed consent
Consent for publication has been obtained from all co-authors.
Rights and permissions
About this article
Cite this article
Liedtke, C., Kolberg, HC., Kerschke, L. et al. Systematic analysis of parameters predicting pathological axillary status (ypN0 vs. ypN+) in patients with breast cancer converting from cN+ to ycN0 through primary systemic therapy (PST). Clin Exp Metastasis 35, 777–783 (2018). https://doi.org/10.1007/s10585-018-9938-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-018-9938-2