Abstract
Sexually transmitted infections (STIs) have been explored in various sexual subgroups. While excellent, these analyses have primarily occurred from uniquely biologic, epidemiologic, or sociologic perspectives. Missing from these discussions has been in-depth presentations of the dynamics of STI transmission from all three viewpoints simultaneously. In this paper, I present information about STI transmission for each STI, including considerations of prevalence, and then review the STI research and of the concept of risk. I then apply these three considerations to a fictitious case study to show their importance and utility. I close by arguing that this information could strengthen future sociologic reviews of STIs and sexual health by helping such researchers include more nuanced understandings about STIs.
Similar content being viewed by others
Notes
In the jurisdiction where I work, nurse practitioners can autonomously order all medications and testing related to STI diagnosis, treatment, and management, including referrals and consultations. Nurse practitioners are thus equal in scope of practice to family physicians and can work independently in their practice, without needing to collaborate with physicians.
References
Akobeng, A. K. (2007). Understanding diagnostic tests 1: Sensitivity, specificity, and predictive values. Acta Paediatrica,96, 338–341.
Alexander, P. (1996). Bathhouses and brothels: Symbolic sites in discourse and practice. In Dangerous Bedfellows (Eds.), Policing public sex (pp. 221–250). Boston: South End Press.
Anderson, R. M., & May, R. M. (1991). Infectious diseases of humans: Dynamics and control. Oxford, England: Oxford University Press.
Barker, M., & Langdridge, D. (2010). Introduction. In M. Barker & D. Langdridge (Eds.), Understanding non-monogamies (pp. 3–8). New York: Routledge.
Berube, A. (2003). The history of gay bathhouses. Journal of Homosexuality,44(3–4), 33–53.
Beuhler, J. W. (2008). Surveillance. In K. J. Rothman, S. Greenland, & T. L. Lash (Eds.), Modern epidemiology (3rd ed., pp. 459–480). Philadelphia: Lippincott Williams & Wilkins.
Brandt, A. M. (1978). Racism and research: The case of the Tuskegee syphilis study. The Hastings Center Report,8(6), 21–29.
Buechner, S. A. (2002). Common skin disorders of the penis. British Journal of Urology International,90, 498–506.
Calabrese, S. K., & Mayer, K. H. (2019). Providers should discuss U = U with all patients with HIV. The Lancet HIV,6(4), E211–E213. https://doi.org/10.1016/S2352-3018(19)30030-X.
Celada, M. T., Merchant, R. C., Waxman, M. J., & Sherwin, A. M. (2011). An ethical evaluation of the 2006 Centers for Disease Control and Prevention recommendations for HIV testing in health care settings. American Journal of Bioethics,11(4), 31–40.
Centers for Disease Control and Prevention [CDC]. (2018a). Sexually transmitted disease surveillance 2017. https://www.cdc.gov/std/stats17/natoverview.htm.
Centers for Disease Control and Prevention [CDC]. (2018b). Antibiotic-resistant gonorrhea. https://www.cdc.gov/std/gonorrhea/arg/default.htm.
Centers for Disease Control and Prevention [CDC]. (2018c). Sexually transmitted disease surveillance 2017—Syphilis. https://www.cdc.gov/std/stats17/syphilis.htm.
Chan, P. A., Robinette, A., Montgomery, M., Almonte, A., Cu-Uvin, S., Lonks, J. R., et al. (2016). Extragenital infections caused by Chlamydia trachomatis and Neisseria gonorrhoeae: A review of the literature. Infectious Diseases in Obstetrics and Gynecology. https://doi.org/10.1155/2016/5758387
Choudhri, Y., Miller, J., Sandhu, J., Leon, A., & Aho, J. (2018). Infectious and congenital syphilis in Canada, 2010–2015. Canadian Communicable Disease Report,44(2), 43–48.
Chu, L. F., Utengen, A., Kadry, B., Kucharski, S. E., Campos, H., Crockett, J., … Clauson, K. A. (2016). “Nothing about us without us”—Patient partnership in medical conferences. British Medical Journal,354, i3883. https://doi.org/10.1136/bmj.i3883
Conley, T. D., Perry, M., Gusakova, S., & Piemonte, J. L. (2019). Monogamous halo effects: The stigma of non-monogamy within collective sex environments [Commentary]. Archives of Sexual Behavior,48, 31–34.
Deeks, S. G., Overbaugh, J., Phillips, A., & Buchbinder, S. (2015). HIV infection. Nature Reviews,1, 15035. https://doi.org/10.1038/nrdp.2015.35.
Dicker, R. C. (1992). Principles of epidemiology (2nd ed.). Atlanta, GA: U.S. Department of Health and Human Services. http://www.ciphi.ca/hamilton/Content/documents/principles.pdf.
Fleming, D. T., & Wasserheit, J. N. (1999). From epidemiological synergy to public health policy and practice: The contribution of other sexually transmitted diseases to sexual transmission of HIV. Sexually Transmitted Infections,75(1), 3–17.
Foucault, M. (1977). Discipline and punish: The birth of the prison. New York: Vintage Books.
Frank, K. (2019a). Rethinking risk, culture, and intervention in collective sex environments. Archives of Sexual Behavior,48, 3–30.
Frank, K. (2019b). Response to commentaries. Archives of Sexual Behavior,48, 69–77.
Frank, K., & DeLamater, J. (2010). Deconstructing monogamy: Boundaries, identities, and fluidities across relationships. In M. Barker & D. Langdridge (Eds.), Understanding non-monogamies (pp. 9–20). New York: Routledge.
Friedman, D. S., & O’Byrne, P. (in press). Extragenital testing increases case detection of gonorrhea and chlamydia: The impact of implementing nucleic acid amplification testing. Canadian Communicable Disease Report.
Garnett, G. P. (2008). The transmission dynamics of sexually transmitted infections. In K. K. Holmes, P. Sparling, W. Stamm, P. Piot, J. Wasserheit, L. Corey, & M. Cohen (Eds.), Sexually transmitted diseases (4th ed., pp. 27–39). New York: McGraw Hill.
Grant, R. M., Lama, J. R., Anderson, P. L., McMahan, V., Liu, A. Y., Vargas, L., et al. (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine,363(27), 2587–2599.
Grov, C., & Parsons, J. T. (2006). Bug chasing and gift giving: The potential for HIV transmission among barebackers on the Internet. AIDS Education and Prevention,18(6), 490–503.
Hanssens, C. (2007). Legal and ethical implications of opt-out HIV testing. Clinical Infectious Diseases,45(Suppl. 4), S232–S239.
Hollingsworth, T. D., Anderson, R. M., & Fraser, C. (2008). HIV-1 transmission, by stage of infection. Journal of Infectious Diseases,198(5), 687–693.
Holmes, D., O’Byrne, P., Murray, S. J., Hammond, C., & Mercier, M. (2018). Transgressive assemblages: An ethnography of gay group sex. In D. Holmes, S. J. Murray, & T. Foth (Eds.), Radical sex between men: Assembling desiring-machines (pp. 153–176). New York: Routledge.
Huffam, S., Chow, E. P. F., Leeyaphan, C., Fairley, C. K., Hocking, J. S., Phillips, S., et al. (2017). Chlamydia infection between men and women: A cross-sectional study of heterosexual partnerships. Open Forum of Infectious Diseases,4(3), ofx160. https://doi.org/10.1093/ofid/ofx160.
Knox, J., Yi, H., Reddy, V., Maimane, S., & Sandfort, T. (2010). The fallacy of intimacy: Sexual risk behavior and beliefs about trust and condom use among men who have sex with men in South Africa. Psychology, Health & Medicine,15(6), 660–671.
Lotringer, S. (2007). Overexposed: Perverting perspectives. Los Angeles: Semiotext(e).
Luiken, G. P. M., Joore, I. K., Taselaar, A., Schuit, S. C. E., Geerlings, S. E., Govers A., et al. (2017). Non-targeted HIV screening in emergency departments in the Netherlands. Netherlands Journal of Medicine,75(9), 386–393.
Lupton, D. (1995). The imperative of health: Public health and the regulated body. London: Sage.
Lupton, D. (1999). Risk. London: Routledge.
Mays, V. M., Coles, C. N., & Cochran, S. D. (2012). Is there a legacy of the U.S. Public Health syphilis study at Tuskegee in HIV/AIDS-related beliefs among heterosexual African Americans and Latinos? Ethics & Behavior,22(6), 461–471.
McGough, L. J. (2008). Historical perspectives on sexually transmitted diseases: Challenges for prevention and control. In K. K. Holmes, P. Sparling, W. Stamm, P. Piot, J. Wasserheit, L. Corey, & M. Cohen (Eds.), Sexually transmitted diseases (4th ed., pp. 3–11). New York: McGraw Hill.
McGough, L. J., & Handsfield, H. H. (2007). History of behavioral interventions in STD control. In S. O. Aral & J. M. Douglas (Eds.), Behavioral interventions for prevention and control of sexually transmitted diseases (pp. 3–22). New York: Springer.
Mertz, G. J. (2008). Asymptomatic shedding of herpes simplex virus 1 and 2: Implications for prevention and transmission. Journal of Infectious Diseases,198(8), 1098–1100.
Meunier, E., Escoffier, J., & Siegal, K. (2019). Rethinking risks and interventions beyond HIV: The importance of contextualizing collective sex [Commentary]. Archives of Sexual Behavior,48, 51–56.
Moores, A., Phillips, J. C., O’Byrne, P., & MacPherson, P. A. (2015). Anal cancer screening knowledge, attitudes, and experiences among men who have sex with men in Ottawa, Ontario. Canadian Journal of Human Sexuality,24(3), 228–236.
Moors, A. C. (2019). Moving past the rose-tinted lens of monogamy: Onward with critical self-examination and (sexually) healthy science. Archives of Sexual Behavior,48, 57–61.
Morris, M., Goodreau, S., & Moody, J. (2008). Sexual networks, concurrency, and STD/HIV. In K. K. Holmes, P. Sparling, W. Stamm, P. Piot, J. Wasserheit, L. Corey, & M. Cohen (Eds.), Sexually transmitted diseases (4th ed., pp. 109–125). New York: McGraw Hill.
O’Byrne, P. (2008). The dissection of risk: A conceptual analysis. Nursing Inquiry,15(1), 30–39.
O’Byrne, P. (2012). Population health and social governance: Analyzing the mainstream incorporation of ethnography. Qualitative Health Research,22(6), 859–867.
O’Byrne, P. (2019a). Population health and social governance: A review, an update, some clarifications, and a response. Qualitative Health Research,29(5), 731–738.
O’Byrne, P. (2019b). HIV PEP and nursing scholarship: A review of critical theory and social justice. Witness: The Canadian Journal of Critical Nursing Discourse,1(1), 28–38.
O’Byrne, P., & Gagnon, M. (2012). HIV criminalization and nursing practice. Aporia,4(2), 5–34.
O’Byrne, P., & Haines, M. (in press). A qualitative exploratory study of consensual non-monogamy: Sexual scripts, stratifications, and charmed circles. Social Theory & Health. https://doi.org/10.1057/s41285-019-00120-1.
O’Byrne, P., & Holmes, D. (2008). Researching marginalized populations: Ethical concerns about ethnography. Canadian Journal of Nursing Research,40(3), 144–159.
O’Byrne, P., & MacPherson, P. A. (2016). HIV treatment as prevention in men who have sex with men: Examining the evidence. Canadian Medical Association Journal,188(3), 198–203.
O’Byrne, P., & MacPherson, P. A. (2019). Syphilis. British Medical Journal,365, I4159. https://doi.org/10.1136/bmj.l4159.
O’Byrne, P., MacPherson, P. A., Ember, A., Grayson, M. O., & Bourgault, A. (2014). Overview of a gay men’s STI/HIV testing clinic in Ottawa: Clinical operations and outcomes. Canadian Journal of Public Health,105(5), e389–e394.
O’Byrne, P., & Watts, J. (2011). Exploring sexual networks: A pilot study of swingers’ sexual behaviour and health-care-seeking practices. Canadian Journal of Nursing Research,43(1), 80–97.
O’Byrne, P., & Woodyatt, C. (2012). Sexual health nursing assessments: Examining the violence of intimate exposures. In T. Rudge & D. Holmes (Eds.), Re(thinking) violence in health care settings (pp. 189–199). Surrey, England: Ashgate.
Parsons, J. T., Schrimshaw, E. W., Wolitski, R. J., Halkitis, P. N., Pucell, D. W., Hoff, C. C., & Gomez, C. A. (2005). Sexual harm reduction practices of HIV-seropositive gay and bisexual men: Serosorting, strategic positioning, and withdrawal before ejaculation. AIDS,19(suppl. 1), S13–S25.
Perron, A., Fluet, C., & Holmes, D. (2005). Agents of care and agents of the state: Bio-power and nursing practice. Journal of Advanced Nursing,50(5), 536–544.
Pharmaceuticals Research and Manufacturers of America. (PHRMA). (2014). Twenty-five years of progress against hepatitis C: Setbacks and stepping stones. http://phrma-docs.phrma.org/sites/default/files/pdf/Hep-C-Report-2014-Stepping-Stones.pdf.
Pisani, E. (2009). The wisdom of whores: Bureaucrats, brothels, and the business of AIDS. London: W.W. Norton & Co.
Public Health Agency of Canada (PHAC). (2013). Management and treatment of specific syndromes. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-19.html#table-1.
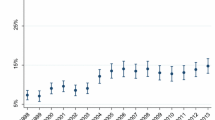
Public Health Agency of Canada (PHAC). (2017). Canadian sexually transmitted infection cases. https://www.datawrapper.de/_/rU7ta/.
Public Health Agency of Canada (PHAC). (2019). Canadian guidelines on sexually transmitted infections. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections.html.
Rubin, G. (1984). Thinking sex: Notes for a radical theory of the politics of sexuality. In C. Vance (Ed.), Pleasure and danger (pp. 143–178). London: Routledge.
Schachter, J., & Stephens, R. S. (2008). Biology of Chlamydia trachomatis. In K. K. Holmes, P. Sparling, W. Stamm, P. Piot, J. Wasserheit, L. Corey, & M. Cohen (Eds.), Sexually transmitted diseases (4th ed., pp. 555–574). New York: McGraw Hill.
Scott-Sheldon, L. A. J., & Chan, P. A. (2020). Increasing sexually transmitted infections in the U.S.: A call for action for research, clinical, and public health practice [Guest Editorial]. Archives of Sexual Behavior, 49, 13–17.
Shah, C. P. (2003). Public health and preventive medicine in Canada (5th ed.). Toronto: Elsevier.
Sparling, P. F. (2008). Biology of Neisseria gonorrhoeae. In K. K. Holmes, P. Sparling, W. Stamm, P. Piot, J. Wasserheit, L. Corey, & M. Cohen (Eds.), Sexually transmitted diseases (4th ed., pp. 607–626). New York: McGraw Hill.
Tan, D. H. S., Hull, M., Yoong, D., Tremblay, C., O’Byrne, P., Thomas, R., et al. (2017). Canadian guideline on HIV pre-exposure prophylaxis and nonoccupational postexposure prophylaxis. Canadian Medical Association Journal,189, 1448–1458.
Taylor, M. M., Rotblatt, H., Brooks, J. T., Montoya, J., Aynalem, G., Smith, L., et al. (2004). Epidemiologic investigation of a cluster of workplace HIV infections in the adult film industry: Los Angeles, California, 2004. Clinical Infectious Diseases,44(2), 301–305.
UNAIDS. (2017). Confronting discrimination: Overcoming HIV-related stigma and discrimination in health-care settings and beyond. https://www.unaids.org/sites/default/files/media_asset/confronting-discrimination_en.pdf.
Unemo, M., & Jensen, J. J. (2017). Antimicrobial-resistant sexually transmitted infections: Gonorrhoea and Mycoplasma genetalium. Nature Reviews,14, 139–152.
van Liere, G. A., Hoebe, C. J., Niekamp, A. M., Koedijk, F. D., & Dukers-Muijeres, N. H. (2013). Standard symptom- and sexual history-based testing misses anorectal Chlamydia trachomatis and Neisseria gonorrhoeae infections in swingers and men who have sex with men. Sexually Transmitted Diseases,40(4), 285–289.
Ward, H., & Ronn, M. (2010). The contribution of STIs to the sexual transmission of HIV. Current Opinion in HIV/AIDS,5(4), 305–310.
Watts, J., & O’Byrne, P. (2019). ‘I don’t care if you think I’m gay … that won’t make me either promiscuous or HIV-positive’: HIV, stigma, and the paradox of the gay men’s sexual health clinic—An exploratory study. Applied Nursing Research,47, 1–3.
Wawer, M. J., Gray, R. H., Sewankambo, N. K., Serwaddo, D., Li, X., Laeyendecker, O., et al. (2005). Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. Journal of Infectious Diseases,191(9), 1403–1409.
Whitehead, J., Shaver, J., & Stephenson, R. (2016). Outness, stigma, and primary health care utilization among rural LGBT populations. PLoS ONE,11(1), e0146139. https://doi.org/10.1371/journal.pone.0146139
Wong, T., Singh, A., Mann, J., Hansen, L., & McMahon, S. (2004). Gender differences in bacterial STIs in Canada. BMC Women’s Health,4(Suppl 1), S26. https://doi.org/10.1186/1472-6874-4-S1-S26
World Health Organization (WHO). (2019a). Sexually transmitted infections (STIs)—Fact sheet. https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis).
World Health Organization (WHO). (2019b). Types of surveillance. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/en/.
Zablotska, I. B., Grulich, A. E., De Wit, J., & Prestage, G. (2011). Casual sexual encounters among gay men: Familiarity, trust, and unprotected anal intercourse. AIDS and Behavior,15(3), 607–612.
Acknowledgements
Patrick O’Byrne holds a research chair in public health and HIV prevention from the Ontario HIV Treatment Network.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest.
Informed Consent
No participants were involved in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
O’Byrne, P. Considerations for Research on Sexually Transmitted Infections (STIs): Reflections of an STI Clinician–Researcher. Arch Sex Behav 49, 1863–1873 (2020). https://doi.org/10.1007/s10508-020-01726-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-020-01726-7