Abstract
The pathogenesis and pathophysiological underpinnings of cartilage degradation are not well understood. Either mechanically or enzymatically mediated degeneration at the fibril level can lead to acute focal injuries that will, overtime, cause significant cartilage degradation. Understanding the relationship between external loading and the basic molecular structure of cartilage requires establishing a connection between the fibril-level defects and its aggregate effect on cartilage. In this work, we provide a multiscale constitutive model of cartilage to elucidate the effect of two plausible fibril degradation mechanisms on the aggregate tissue: tropocollagen crosslink failure (β) and a generalized surface degradation (δ). Using our model, the mechanics of aggregate tissue shows differed yield stress and post-yield behavior after crosslink failure and surface degradation compared to intact cartilage, and the tissue-level aggregate behaviors are different from the fibrillar behaviors observed in the molecular dynamics simulations. We also compared the effect of fibrillar defects in terms of crosslink failure and surface degradation in different layers of cartilage within the macroscale tissue construct during a simulated nanoindentation test. Although the mechanical properties of cartilage tissue were largely contingent upon the mechanical properties of the fibril, the macroscale mechanics of cartilage tissue showed ~ 10% variation in yield strain (tissue yield strain: ~ 27 to ~ 37%) compared to fibrillar yield strain (fibrillar yield strain: ~ 16 to ~ 26%) for crosslink failure and ~ 7% difference for the surface degradation (yield strain variations at the tissue: ~ 30 to ~ 37% and fibril: ~ 24 to ~ 26%) at the superficial layer. The yield strain was further delayed in middle layers at least up to 30% irrespective of the failure mechanisms. The cartilage tissue appeared to withstand more strain than the fibrils. The degeneration mechanisms of fibril differentially influenced the aggregate mechanics of cartilage, and the deviation may be attributed to fiber–matrix interplay, depth-dependent fiber orientation and fibrillar defects with different degradation mechanisms. The understanding of the aggregate stress–strain behavior of cartilage tissue, cartilage degradation and its underlying biomechanical factors is important for developing engineering approaches and therapeutic interventions for cartilage pathologies.






Similar content being viewed by others
References
Addi C, Murschel F, De Crescenzo G (2016) Design and use of chimeric proteins containing a collagen-binding domain for wound healing and bone regeneration. Tissue Eng Part B Rev 23:163–182
Adouni M, Dhaher YY (2016) A multi-scale elasto-plastic model of articular cartilage. J Biomech 49:2891–2898
Adouni M, Shirazi-Adl A, Shirazi R (2012) Computational biodynamics of human knee joint in gait: from muscle forces to cartilage stresses. J Biomech 45:2149–2156
Akizuki S, Mow VC, Müller F, Pita JC, Howell DS, Manicourt DH (1986) Tensile properties of human knee joint cartilage: I. Influence of ionic conditions, weight bearing, and fibrillation on the tensile modulus. J Orthop Res 4:379–392
Arbabi V, Pouran B, Weinans H, Zadpoor A (2015) Transport of neutral solute across articular cartilage: the role of zonal diffusivities. J Biomech Eng 137:071001
Asaro RJ, Rice JR (1977) Strain localization in ductile single crystals. J Mech Phys Solids 25:309–338
Ateshian GA (2009) The role of interstitial fluid pressurization in articular cartilage lubrication. J Biomech 42:1163–1176
Atkinson T, Haut R, Altiero N (1998) Impact-induced fissuring of articular cartilage: an investigation of failure criteria. J Biomech Eng 120:181–187
Backus JD et al (2011) Cartilage viability and catabolism in the intact porcine knee following transarticular impact loading with and without articular fracture. J Orthop Res 29:501–510
Bae WC, Lewis CW, Levenston ME, Sah RL (2006) Indentation testing of human articular cartilage: effects of probe tip geometry and indentation depth on intra-tissue strain. J Biomech 39:1039–1047
Bae WC, Schumacher BL, Sah RL (2007) Indentation probing of human articular cartilage: effect on chondrocyte viability. Osteoarthr Cartil 15:9–18
Barrett AJ, Rawlings ND, Woessner JF (2012) Handbook of proteolytic enzymes. Elsevier Science, New York
Bella J, Eaton M, Brodsky B, Berman H (1994) Crystal and molecular structure of a collagen-like peptide at 1.9 A resolution. Science 266:75–81
Bi X, Li G, Doty S, Camacho N (2005) A novel method for determination of collagen orientation in cartilage by Fourier transform infrared imaging spectroscopy (FT-IRIS). Osteoarthr Cartil 13:1050–1058
Bonassar LJ, Jeffries KA, Paguio CG, Grodzinsky AJ (1995) Cartilage degradation and associated changes in biomechanical and electromechanical properties. Acta Orthop Scand 66:38–44
Bozec L, Horton M (2005) Topography and mechanical properties of single molecules of type I collagen using atomic force microscopy. Biophys J 88:4223–4231
Broom ND, Silyn-Roberts H (1989) The three-dimensional ‘knit’ of collagen fibrils in articular cartilage. Connect Tissue Res 23:261–277
Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA (2006) Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma 20:739–744
Buckley MR, Gleghorn JP, Bonassar LJ, Cohen I (2008) Mapping the depth dependence of shear properties in articular cartilage. J Biomech 41:2430–2437
Buehler MJ (2006) Nature designs tough collagen: explaining the nanostructure of collagen fibrils. Proc Natl Acad Sci 103:12285–12290
Buehler MJ (2008) Nanomechanics of collagen fibrils under varying cross-link densities: atomistic and continuum studies. J Mech Behav Biomed Mater 1:59–67
Chan DD, Neu CP, Hull ML (2009) In situ deformation of cartilage in cyclically loaded tibiofemoral joints by displacement-encoded MRI. Osteoarthr Cartil 17:1461–1468
Chan DD, Cai L, Butz KD, Trippel SB, Nauman EA, Neu CP (2016) In vivo articular cartilage deformation: noninvasive quantification of intratissue strain during joint contact in the human knee. Sci Rep 6:19220. https://www.nature.com/articles/srep19220#supplementary-information
Chang S-W, Shefelbine Sandra J, Buehler Markus J (2012) Structural and mechanical differences between collagen homo- and heterotrimers: relevance for the molecular origin of brittle bone disease. Biophys J 102:640–648
Chen JM, Sheldon A, Pincus MR (1995) Three-dimensional energy-minimized model of human Type II “Smith” collagen microfibril. J Biomol Struct Dyn 12:1129–1159
Clarke IC (1971) Articular cartilage: a review and scanning electron microscope study. Bone Joint J 53:732–750
Danso EK, Honkanen JTJ, Saarakkala S, Korhonen RK (2014) Comparison of nonlinear mechanical properties of bovine articular cartilage and meniscus. J Biomech 47:200–206
Depalle B, Qin Z, Shefelbine SJ, Buehler MJ (2016) Large deformation mechanisms, plasticity, and failure of an individual collagen fibril with different mineral content. J Bone Miner Res 31:380–390
Domene C, Jorgensen C, Abbasi SW (2016) A perspective on structural and computational work on collagen. Phys Chem Chem Phys 18:24802–24811
Eleswarapu SV, Responte DJ, Athanasiou KA (2011) Tensile properties, collagen content, and crosslinks in connective tissues of the immature knee joint. PLoS ONE 6:e26178
Eppell SJ, Smith BN, Kahn H, Ballarini R (2006) Nano measurements with micro-devices: mechanical properties of hydrated collagen fibrils. J R Soc Interface 3:117–121
Evans CH (1981) Interactions of tervalent lanthanide ions with bacterial collagenase (clostridiopeptidase A). Biochem J 195:677–684
Franchi M, Trirè A, Quaranta M, Orsini E, Ottani V (2007) Collagen structure of tendon relates to function. Sci World J 7:404–420
Gardiner BS, Woodhouse FG, Besier TF, Grodzinsky AJ, Lloyd DG, Zhang L, Smith DW (2016) Predicting knee osteoarthritis. Ann Biomed Eng 44:222–233
Gasser TC, Holzapfel GA (2002) A rate-independent elastoplastic constitutive model for biological fiber-reinforced composites at finite strains: continuum basis, algorithmic formulation and finite element implementation. Comput Mech 29:340–360
Gautieri A, Vesentini S, Redaelli A, Buehler MJ (2011) Hierarchical structure and nanomechanics of collagen microfibrils from the atomistic scale up. Nano Lett 11:757–766
Graham JS, Vomund AN, Phillips CL, Grandbois M (2004) Structural changes in human type I collagen fibrils investigated by force spectroscopy. Exp Cell Res 299:335–342
Halberg D, Proulx G, Doege K, Yamada Y, Drickamer K (1988) A segment of the cartilage proteoglycan core protein has lectin-like activity. J Biol Chem 263:9486–9490
Haut R, Ide T, De Camp C (1995) Mechanical responses of the rabbit patello-femoral joint to blunt impact. J Biomech Eng 117:402–408
Hayes WC, Keer LM, Herrmann G, Mockros LF (1972) A mathematical analysis for indentation tests of articular cartilage. J Biomech 5:541–551
Hollander AP, Heathfield TF, Webber C, Iwata Y, Bourne R, Rorabeck C, Poole AR (1994) Increased damage to type II collagen in osteoarthritic articular cartilage detected by a new immunoassay. J Clin Investig 93:1722
Holmes DF, Kadler KE (2006) The 10 + 4 microfibril structure of thin cartilage fibrils. Proc Natl Acad Sci 103:17249–17254
Hong J, Evans TM, Mente PL (2015) Study on the damage mechanism of articular cartilage based on the fluid–solid coupled particle model. Adv Mech Eng 7:1687814015581264
Hosseini S, Wilson W, Ito K, Van Donkelaar C (2014) A numerical model to study mechanically induced initiation and progression of damage in articular cartilage. Osteoarthr Cartil 22:95–103
Huebner JL, Williams JM, Deberg M, Henrotin Y, Kraus VB (2010) Collagen fibril disruption occurs early in primary guinea pig knee osteoarthritis osteoarthritis and cartilage/OARS. Osteoarthr Res Soc 18:397–405
Julkunen P, Wilson W, Jurvelin JS, Rieppo J, Qu C-J, Lammi MJ, Korhonen RK (2008) Stress–relaxation of human patellar articular cartilage in unconfined compression: prediction of mechanical response by tissue composition and structure. J Biomech 41:1978–1986
Julkunen P, Wilson W, Isaksson H, Jurvelin JS, Herzog W, Korhonen RK (2013) A review of the combination of experimental measurements and fibril-reinforced modeling for investigation of articular cartilage and chondrocyte response to loading. Comput Math Methods Med 2013:1–23
Kar S, Smith DW, Gardiner BS, Grodzinsky AJ (2016a) Systems based study of the therapeutic potential of small charged molecules for the inhibition of IL-1 mediated cartilage degradation. PLOS ONE 11:e0168047
Kar S, Smith DW, Gardiner BS, Li Y, Wang Y, Grodzinsky AJ (2016b) Modeling IL-1 induced degradation of articular cartilage. Arch Biochem Biophys 594:37–53
Kaukinen A, Laasanen M, Lammentausta E, Halmesmäki E, Helminen H, Jurvelin J, Rieppo J (2005) Destructive testing of articular cartilage in compression-effect of collagen network. In: 51st Annual meeting of the orthopaedic research society
Kempson GE, Freeman MAR, Swanson SAV (1968) Tensile properties of articular cartilage. Nature 220:1127
Kerin AJ, Wisnom MR, Adams MA (1998) The compressive strength of articular cartilage. Proc Inst Mech Eng Part H J Eng Med 212:273–280
Klets O, Mononen ME, Tanska P, Nieminen MT, Korhonen RK, Saarakkala S (2016) Comparison of different material models of articular cartilage in 3D computational modeling of the knee: data from the Osteoarthritis Initiative (OAI). J Biomech 49:3891–3900
Korhonen RK, Tanska P, Kaartinen SM, Fick JM, Mononen ME (2015) New concept to restore normal cell responses in osteoarthritic knee joint cartilage. Exerc Sport Sci Rev 43:143–152
Laasanen M et al (2003) Biomechanical properties of knee articular cartilage. Biorheology 40:133–140
Lee EH (1969) Elastic-plastic deformation at finite strains. J Appl Mech 36:1–6
Li Y, Wang Y, Chubinskaya S, Schoeberl B, Florine E, Kopesky P, Grodzinsky AJ (2015) Effects of insulin-like growth factor-1 and dexamethasone on cytokine-challenged cartilage: relevance to post traumatic osteoarthritis osteoarthritis and cartilage/OARS. Osteoarthr Res Soc 23:266–274
Liu Y, Chan JK, Teoh SH (2015) Review of vascularised bone tissue-engineering strategies with a focus on co-culture systems. J Tissue Eng Regen Med 9:85–105
Lotz M (2001) Cytokines in cartilage injury and repair. Clin Orthop Relat Res 391:S108–S115
Malaspina DC, Szleifer I, Dhaher Y (2017) Mechanical properties of a collagen fibril under simulated degradation. J Mech Behav Biomed Mater 75:549–557
Maroudas A (1976) Balance between swelling pressure and collagen tension in normal and degenerate cartilage. Nature 260:808
Matsushita O, Jung C-M, Minami J, Katayama S, Nishi N, Okabe A (1998) A study of the collagen-binding domain of a 116-kDa Clostridium histolyticum collagenase. J Biol Chem 273:3643–3648
Matsushita O, Koide T, Kobayashi R, Nagata K, Okabe A (2001) Substrate recognition by the collagen-binding domain of Clostridium histolyticum class I collagenase. J Biol Chem 276:8761–8770
Metzmacher I, Radu F, Bause M, Knabner P, Friess W (2007a) A model describing the effect of enzymatic degradation on drug release from collagen minirods. Eur J Pharm Biopharm 67:349–360
Metzmacher I, Ruth P, Abel M, Friess W (2007b) In vitro binding of matrix metalloproteinase-2 (MMP-2), MMP-9, and bacterial collagenase on collagenous wound dressings. Wound Repair Regen 15:549–555
Miyazaki H, Hayashi K (1999) Tensile tests of collagen fibers obtained from the rabbit patellar tendon. Biomed Microdevice 2:151–157
Mononen ME, Tanska P, Isaksson H, Korhonen RK (2016) A novel method to simulate the progression of collagen degeneration of cartilage in the knee: data from the osteoarthritis initiative. Sci Rep 6:21415
Moskowitz RW (2007) Osteoarthritis: diagnosis and medical/surgical management. Lippincott Williams & Wilkins, Philadelphia
Mow VC, Kuei SC, Lai WM, Armstrong CG (1980) Biphasic creep and stress relaxation of articular cartilage in compression: theory and experiments. J Biomech Eng 102:73–84
Muthuri S, McWilliams D, Doherty M, Zhang W (2011) History of knee injuries and knee osteoarthritis: a meta-analysis of observational studies. Osteoarthr Cartil 19:1286–1293
Mwenifumbo S, Shaffer MS, Stevens MM (2007) Exploring cellular behaviour with multi-walled carbon nanotube constructs. J Mater Chem 17:1894–1902
Neu CP, Walton JH (2008) Displacement encoding for the measurement of cartilage deformation. Magn Reson Med 59:149–155
Newberry WN, Mackenzie CD, Haut RC (1998) Blunt impact causes changes in bone and cartilage in a regularly exercised animal model. J Orthop Res 16:348–354
Nötzli H, Clark J (1997) Deformation of loaded articular cartilage prepared for scanning electron microscopy with rapid freezing and freeze-substitution fixation. J Orthop Res 15:76–86
Oyen ML, Shean TA, Strange DG, Galli M (2012) Size effects in indentation of hydrated biological tissues. J Mater Res 27:245–255
Panwar P, Du X, Sharma V, Lamour G, Castro M, Li H, Brömme D (2013) Effects of cysteine proteases on the structural and mechanical properties of collagen fibers. J Biol Chem 288:5940–5950
Panwar P, Lamour G, Mackenzie NCW, Yang H, Ko F, Li H, Brömme D (2015) Changes in structural-mechanical properties and degradability of collagen during aging-associated modifications. J Biol Chem 290:23291–23306
Peters AE, Akhtar R, Comerford EJ, Bates KT (2018) Tissue material properties and computational modelling of the human tibiofemoral joint: a critical review. PeerJ 6:e4298
Piluso S, Lendlein A, Neffe AT (2017) Enzymatic action as switch of bulk to surface degradation of clicked gelatin-based networks. Polym Adv Technol 28:1318–1324
Pratta MA et al (2003) Aggrecan protects cartilage collagen from proteolytic cleavage. J Biol Chem 278:45539–45545
Proctor CS, Schmidt MB, Whipple RR, Kelly MA, Mow VC (1989) Material properties of the normal medial bovine meniscus. J Orthop Res 7:771–782
Repo R, Finlay J (1977) Survival of articular cartilage after controlled impact. J Bone Joint Surg Am 59:1068–1076
Riley KN, Herman IM (2005) Collagenase promotes the cellular responses to injury and wound healing in vivo. J Burns Wounds 4:1–24
Salehghaffari S, Dhaher YY (2015) A phenomenological contact model: understanding the graft–tunnel interaction in anterior cruciate ligament reconstructive surgery. J Biomech 48:1844–1851
Saxena RK, Sahay KB, Guha SK (1991) Morphological changes in the bovine articular cartilage subjected to moderate and high loadings. Cells Tissues Organ 142:152–157
Schinagl RM, Gurskis D, Chen AC, Sah RL (1997) Depth-dependent confined compression modulus of full-thickness bovine articular cartilage. J Orthop Res 15:499–506
Shirazi R, Shirazi-Adl A (2008) Deep vertical collagen fibrils play a significant role in mechanics of articular cartilage. J Orthop Res 26:608–615
Shirazi R, Shirazi-Adl A (2009) Computational biomechanics of articular cartilage of human knee joint: effect of osteochondral defects. J Biomech 42:2458–2465
Shirazi R, Shirazi-Adl A, Hurtig M (2008) Role of cartilage collagen fibrils networks in knee joint biomechanics under compression. J Biomech 41:3340–3348
Shoulders MD, Raines RT (2009) Collagen structure and stability. Annu Rev Biochem 78:929–958
Sigma-Aldrich. Collagenase from Clostridium histolyticum. High purity, purified by chromatography, Type VII, ≥4 FALGPA units/mg solid, lyophilized powder, 1,000-3,000 CDU/mg solid (CDU = collagen digestion units). https://www.sigmaaldrich.com/catalog/product/sigma/c0773?lang=en®ion=US
Silver FH, Siperko LM (2003) Mechanosensing and mechanochemical transduction: how is mechanical energy sensed and converted into chemical energy in an extracellular matrix? Crit Rev Biomed Eng 31:255–331
Spahn G, Kahl E, Klinger Hans M, Mückley T, Günther M, Hofmann Gunther O (2007) Mechanical behavior of intact and low-grade degenerated cartilage/Mechanische Eigenschaften von intaktem und niedriggradig geschädigtem Knorpel 52. Biomed Tech 52:216–222
Stolz M, Raiteri R, Daniels A, VanLandingham MR, Baschong W, Aebi U (2004) Dynamic elastic modulus of porcine articular cartilage determined at two different levels of tissue organization by indentation-type atomic force microscopy. Biophys J 86:3269–3283
Stolz M et al (2009) Early detection of aging cartilage and osteoarthritis in mice and patient samples using atomic force microscopy. Nat Nanotechnol 4:186
Tang H, Buehler MJ, Moran B (2009) A constitutive model of soft tissue: from nanoscale collagen to tissue continuum. Ann Biomed Eng 37:1117–1130
Tang Y, Ballarini R, Buehler MJ, Eppell SJ (2010) Deformation micromechanisms of collagen fibrils under uniaxial tension. J R Soc Interface 7:839–850
Thompson JR, Oegema JT, Lewis J, Wallace L (1991) Osteoarthrotic changes after acute transarticular load. An animal model. J Bone Joint Surg Am 73:990–1001
Thompson RC, Vener MJ, Griffiths HJ, Lewis JL, Oegema TR, Wallace L (1993) Scanning electron-microscopic and magnetic resonance-imaging studies of injuries to the patellofemoral joint after acute transarticular loading. JBJS 75:704–713
Toyoshima T, Matsushita O, Minami J, Nishi N, Okabe A, Itano T (2001) Collagen-binding domain of a Clostridium histolyticum collagenase exhibits a broad substrate spectrum both in vitro and in vivo. Connect Tissue Res 42:281–290
Tzafriri AR, Bercovier M, Parnas H (2002) Reaction diffusion model of the enzymatic erosion of insoluble fibrillar matrices. Biophys J 83:776–793
Verzijl N et al (2002) Crosslinking by advanced glycation end products increases the stiffness of the collagen network in human articular cartilage: a possible mechanism through which age is a risk factor for osteoarthritis. Arthritis Rheumatol 46:114–123
Volokh KY (2007a) Hyperelasticity with softening for modeling materials failure. J Mech Phys Solids 55:2237–2264
Volokh KY (2007b) Softening hyperelasticity for modeling material failure: analysis of cavitation in hydrostatic tension. Int J Solids Struct 44:5043–5055
Watanabe H, Kimata K, Line S, Strong D, L-y Gao, Kozak CA, Yamada Y (1994) Mouse cartilage matrix deficiency (CMD) caused by a 7 bp deletion in the aggrecan gene. Nature Genet 7:154–157
Webb EC (1992) Enzyme nomenclature 1992. Recommendations of the nomenclature committee of the international union of biochemistry and molecular biology on the nomenclature and classification of enzymes, vol 6. Academic Press, Cambridge
Welgus H, Jeffrey J, Stricklin G, Roswit W, Eisen A (1980) Characteristics of the action of human skin fibroblast collagenase on fibrillar collagen. J Biol Chem 255:6806–6813
Williamson AK, Chen AC, Masuda K, Thonar EJMA, Sah RL (2003) Tensile mechanical properties of bovine articular cartilage: variations with growth and relationships to collagen network components. J Orthop Res 21:872–880
Wilson JJ, Matsushita O, Okabe A, Sakon J (2003) A bacterial collagen-binding domain with novel calcium-binding motif controls domain orientation. EMBO J 22:1743–1752
Wilson W, van Donkelaar CC, van Rietbergen B, Ito K, Huiskes R (2004) Stresses in the local collagen network of articular cartilage: a poroviscoelastic fibril-reinforced finite element study. J Biomech 37:357–366
Wilson CJ, Clegg RE, Leavesley DI, Pearcy MJ (2005) Mediation of biomaterial–cell interactions by adsorbed proteins: a review. Tissue Eng 11:1–18
Xu Y et al (2000) Multiple binding sites in collagen type I for the integrins α1β1 and α2β1. J Biol Chem 275:38981–38989
Zderic SA (1995) Muscle, matrix, and bladder function. In: Zderic SA (ed) Advances in experimental medicine and biology, vol 385. Plenum Press, New York. https://nla.gov.au/nla.cat-vn950200
Acknowledgements
The authors would like to thank Bethany Powell (PhD candidate) and David Malaspina (research fellow) in the Szleifer and Dhaher Labs at Northwestern University for the discussion in implementing surface adsorption to estimate surface degradation. The authors greatly appreciate the financial support of the National Institutes of Health for the Grant # U01 EB015410-01A1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
1.1 Multiscale modeling of cartilage strain energy
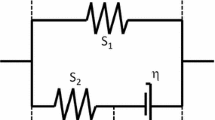
In this study, the evolution of plastic stress in the fibril is triggered by the effective fibril yield stress derived from fibril strain energy (Tang et al. 2009). The yield stress is connected to the fibril yield condition as obtained from MDS (i), the plastic strain rate (ii) and the flow resistance (iii) of the tissues as follows:
These relationships help describe the hierarchical coupling between nanoscale collagen degradation and material properties of fibrils (Fig. 6). The plastic parameters, \(\dot{\gamma } = 0.01/\text{s}\) and p = 0.05, are fixed due to wide agreement in the literature with respect to cartilage’s plastic rate of deformation (Gasser and Holzapfel 2002). A collagen fiber, which is modeled as the fiber-reinforced composite, includes the descriptions of fibril and incompressible neo-Hookean matrix. The elastic strain energy of the fiber can eventually be expressed under extension as
The total elastic strain energy density of the fiber is therefore expressed as
The framework is hierarchically used to model the soft tissue (cartilage) as the fiber-reinforced composite material as well, and the corresponding axial and shear strain energy are written as
The total strain energy of the tissue is defined by
The noticeable feature of the strain energy function is its dependence on both elastic stretch and the total deformation. This is due to the assumption that the plastic deformation occurs only in the fiber while the matrix materials always remain elastic. The total strain energy for the fiber (Wfb) and tissue (Wt) were therefore formulated mathematically combining axial and shear strains for the both, and eventually, the total stress σt was expressed with fibrillar σf and nonfibrillar \(\sigma^{\text{nf}}\) stress tensors as shown in Eq. (4) in the main article. The plastic stress in Eq. (4) becomes dominant when the effective stress, \(\sigma_{y}^{\text{eff}}\), is more than the fibril yield strength, which in this case varies depending on the crosslink failure and surface degradation. The elastic part of the deformation gradient is determined by \({\mathbf{F}}_{e} = {\mathbf{FF}}_{p}^{ - 1}\), where the plastic deformation gradient is \(f\left( {\lambda_{\text{fp}} } \right)\). The stretch, λfp, is unity up to the yield point and only comes into play beyond the fiber yield strength. The plastic stretch depends on the plastic strain rate \(\dot{\gamma }\), which ultimately controls the plastic part of the deformation gradient (Fig. 7).
Appendix B
2.1 Nonlinear optimization of degenerated fibril
The nonlinear optimization function lsqnonlin in MATLAB (The MathWorks Inc., Natick, MA, USA) was employed with the trust region reflective algorithm, which minimized an objective function \(f\left( {\mathbf{x}} \right)\) in a least square sense \(\left( {\sum\nolimits_{n} {\left[ {f\left( {\mathbf{x}} \right)} \right]^{2} } } \right)\). The optimal objective function provides a good compromise between σ MDSfl (represents either \(\left( {\sigma_{{^{fl} }} \left( \beta \right)} \right)\) and \(\left( {\sigma_{{^{fl} }} \left( \delta \right)} \right)\) depending on degradation mechanisms, crosslink failure and generalized surface degradation, respectively) and \(\sigma_{\text{fl}}^{\text{SEF}}\) for the fibril along the fiber direction,
where \({\mathbf{x}}\) is a vector of the unknown fibril parameters \(\left( {\mu_{o} ,I_{o} ,a_{1} ,a_{2} ,a_{3} } \right)\) with each parameter confined by reasonable bounds as provided in earlier studies (Adouni and Dhaher 2016; Tang et al. 2009). To ensure unbiased estimate of the fibril parameters \(\left( {\mu_{o} ,I_{o} ,a_{1} ,a_{2} ,a_{3} } \right)\), multiple sets of the five fibril parameters selected from a plausible range of values were then used (MultiStart MATLAB function) as the initial inputs to the optimization procedure. The multiple outcomes of the optimization process were then averaged to represent the best fit of the fibril parameters used to characterize the fibril continuum model employed in the subsequent FEA simulations.
Figure 8a displays the fibril stress–strain plot of MD data (solid line) and its corresponding fitted curve (dotted line) for the TC crosslink failure (β), varying from native fibril (100% crosslink) to no crosslink. Figure 8b shows the stress–strain curves (MD data and fitted curve) of a fibril at different levels of surface degradation (δ) varying from an intact fibril.
For the fitted data, the goodness-of-fit (GOF) values—coefficient of determination, R2 (presented as mean ± standard error (SE))—were found 0.983 ± 0.04 for the crosslink failure and 0.978 ± 0.02 for the surface degradation. The fitted curves exhibit acceptable fits to the MDS data for the two degeneration mechanisms.
Appendix C
3.1 Estimation of surface degradation
The enzymatic surface degradation can be estimated based on the fraction of surface occupied by the adsorbate (enzyme). The accumulation of the adsorbate on a surface (adsorbent or substrate) is therefore known as adsorption. In the experiment carried out by Laasanen et al. (2003), collagenase type VII (C 0773, Sigma Chemical Co., St. Louis, MO, USA) was applied to degrade the surface of collagen-II in which surface degradation was estimated considering the binding of collagenase molecules on the collagen surface (Fig. 9). The incubation time (in 37 °C, 5% CO2 atmosphere) for collagenase (30 U/ml)-treated samples was 44 h (Laasanen et al. 2003). Because of unavailability of specific parametric values, the surface coverage (degradation) was calculated using Langmuir adsorption isotherm for a range of physical and mechanical properties widely used for collagen and collagenase enzyme. The Langmuir adsorption isotherm provides one of the simplest and most direct methods to quantify the adsorption process. Since the Langmuir isotherm model typically well suited with isotherm data from protein/enzyme adsorption studies, the model is often used to estimate the protein binding affinity (Metzmacher et al. 2007a, b; Wilson et al. 2005).
3.2 Surface coverage
Surface coverage as per Langmuir Isotherm equation is
where θ is the fractional surface coverage, C is the molar concentration of the solution (here collagenase VII), \(k_{\text{a}}\) is the association constant and \(k_{\text{d}}\) is the dissociation or binding constant. \(k_{\text{a}}\) and \(k_{\text{d}}\) are related as \(k_{\text{a}} = \frac{1}{{k_{\text{d}} }}\).
The Collagen Digestion Unit (CDU) of the collagenase varies between 1000 and 3000 CDU/mg, and its molecular weight is between 68 and 125 kDa (Sigma-Aldrich; Webb 1992). For the ranges of CDU and molecular weight, the concentration, C, of collagenase (30 U/ml) was estimated in the range of \(C = 0.08 \times 10^{ - 6} \sim 0.44 \times 10^{ - 6} \,{\text{mol}}/{\text{L}}\).
The binding constant, \(k_{\text{d}}\), between collagenase VII and collagen varies widely (O(10−5) to O(10−7)) whether determined experimentally and computationally (Addi et al. 2016; Bella et al. 1994; Matsushita et al. 1998, 2001; Toyoshima et al. 2001). However, in most of the reported literature, \(k_{\text{d}}\) was estimated to be in the order of O(10−6) (Bella et al. 1994; Evans 1981; Matsushita et al. 1998, 2001; Toyoshima et al. 2001; Wilson et al. 2003) and was used to calculate the surface coverage using Eq. (12). Considering \(k_{\text{d}} = 4.99 \times 10^{ - 6}\) (Wilson et al. 2003), the fraction of binding sites on collagen occupied by collagenase was estimated to \(\theta_{ \hbox{min} } \cong 0.016\) and \(\theta_{\hbox{max} } \cong 0.081\).
3.3 Estimation of collagen fibrils in cartilage
The number of collagen fibril needs to estimate for the cartilage tissue used in the experiment (Laasanen et al. 2003). The following assumptions are rationally considered to calculate the amount of collagen fibrils in cartilage tissue:
-
1.
Superficial layer or zone is typically 15% of articular cartilage tissue height \(\left( {h_{\text{tissue}} } \right)\)(Adouni et al. 2012; Hollander et al. 1994; Shirazi et al. 2008; Shirazi and Shirazi-Adl 2008).
-
2.
Amount of collagen fibers in the superficial layer is approximately 15% (Adouni et al. 2012; Shirazi and Shirazi-Adl 2009; Shirazi et al. 2008).
-
3.
Fibers are idealized as perfect cylinders of tightly packed monomeric fibrils
-
4.
The fiber diameter is larger than the fibril diameter, \(d_{\text{fb}} \gg d_{\text{fl}}\).
-
5.
Diameter of a fiber \(\left( {d_{\text{fb}} } \right)\) in cartilage generally in the range of \(15.2 \pm 8.3 \sim 29.2 \pm 5.4\,{\text{nm}}\) (Halberg et al. 1988; Holmes and Kadler 2006; Moskowitz 2007; Mwenifumbo et al. 2007; Silver and Siperko 2003; Watanabe et al. 1994)
-
6.
Length of the fiber is assumed to 1 µm (Domene et al. 2016; Gautieri et al. 2011; Liu et al. 2015)
An idealized fiber of tightly packed fibrils is shown in Fig. 10. This idealization is valid as long as the fiber diameter, \(d_{\text{fb}}\), is much larger than the diameter of the fibril, \(d_{\text{fl}}\). When the collagen fibrils come in contact with the enzyme solution, the enzyme diffuses into the fibers and binds to specific sites on fibrils located at the surface of the fibers. Due to the size and organization of the fibrils, the enzyme molecules cannot penetrate the tightly packed (crosslinked) fibrils that make up an individual fiber. The fibrils are also assumed to be incompressible and nonoverlapping (small circles in Fig. 10b).
Schematics of a fiber (a) and its cross section (b) perpendicular to the axis of the fiber [based on (Tzafriri et al. 2002)]
Total number of collagen fibers is assumed to be \(n_{\text{fb}}\) that contribute to the total fiber volume. However, the fiber dimeter is variable depending on its young or mature state, and consequently, the diameters of fibers in the superficial layer vary widely (Moskowitz 2007; Mwenifumbo et al. 2007; Silver and Siperko 2003). Taking into account the minimum and maximum mean values of the fiber diameter, the minimum fiber volume, \(V_{\text{fb}}^{\hbox{min} }\), and maximum fiber volume, \(V_{\text{fb}}^{\hbox{max} }\), of a single collagen fiber have been estimated. Thus, based on the \(V_{fb}^{\hbox{min} }\) and \(V_{\text{fb}}^{\hbox{max} }\), the minimum and maximum number of collagen fibers was estimated to \(n_{\text{fb}}^{\hbox{min} } = 5.913 \times 10^{11}\) and \(n_{\text{fb}}^{\hbox{max} } = 2.216 \times 10^{12}\), respectively.
3.4 Estimation of tropocollagen molecules on the surface
During the surface degradation process, enzymes bind and cleave the tropocollagen molecules on the surface (along the circumference of the fibril) and are schematically shown in Fig. 11. The TC molecules were assumed to be arranged tightly around the circumference of the fibrils. The dimensions of each TC molecule are \(d_{\text{TC}} = 1.5\,{\text{nm}}\), \(l_{\text{TC}} = 300\,{\text{nm}}\), with a (D-periodic) gap of \(67\,{\text{nm}}\) between the TC molecules (Chen et al. 1995; Franchi et al. 2007; Graham et al. 2004; Shoulders and Raines 2009).
Considering the minimum and maximum circumference of the fibers, staggered organization of TC molecules with the periodicity of \(67\,{\text{nm}}\) and (collagen type II) fiber length of \(1\,\upmu{\text{m}}\) (Domene et al. 2016; Gautieri et al. 2011; Liu et al. 2015), the minimum and maximum number of TC molecules around the circumferential was estimated to \(n_{{{\text{TC}}_{\text{surf}} }}^{\hbox{min} } = 5.68 \times 10^{13}\) and \(n_{{{\text{TC}}_{\text{surf}} }}^{\hbox{max} } = 3.89 \times 10^{14}\).
3.5 Estimation of surface degradation
The collagenase type VII used in the Laasanen et al. experiments is bacterial collagenase, which acts both as a collagenase and a gelatinase. Collagenases can only cleave at one site on collagen molecules, but gelatinases can cleave the rest of the sites on the collagen once collagenase has made an initial cut. The bacterial collagenase can cut in multiple places on collagen and was accounted here for estimating the number of binding sites (Fig. 12). Thus, in the current estimation, we considered up to three binding sites/TC (Piluso et al. 2017; Riley and Herman 2005; Xu et al. 2000; Zderic 1995). Hence, the total number of collagenases on cartilage surface was estimated in the range of \(n_{\text{Collagenase}}^{\text{surface}} \approx 2.726 \times 10^{12} \sim 9.453 \times 10^{13}\) molecules.
To the best of our knowledge (with extensive literature search), two different rates of collagen cleavage by the bacterial collagenase have been found and considered here in the estimation process. These are: (i) 22 molecules of collagen are degraded per molecule of collagenase per hour (Barrett et al. 2012; Welgus et al. 1980) and (ii) a unit of collagenase activity is defined to produce 10% cleavage of collagen in 2.5 h at 37o C (Zderic 1995).
Considering cleavage rate as per (i), the number of degraded molecules for 44 h of incubation time (Laasanen et al. 2003) was in the range of \(n_{\text{collagen}}^{{{\text{degraded}}\,{\text{mol}}}} \approx 4.67 \times 10^{16} \sim 2.565 \times 10^{17}\) molecules. With this, the minimum and maximum surface degradation was estimated to 0.01% and 0.201%, respectively. According to cleavage rate as per (ii), the number of degraded molecules for the same incubation time (Laasanen et al. 2003) was in the range of \(n_{\text{collagen}}^{{{\text{degraded}}\,{\text{mol}}}} \approx 3.0 \times 10^{15} \sim 2.054 \times 10^{16}\) molecules. With this, the minimum and maximum surface degradation was estimated to be 0.013% and 3.51%, respectively.
Although Langmuir adsorption isotherm is often considered to estimate the protein binding affinity, the Langmuir model does not take into account the interactions between enzymes—especially when the enzymes (considered as voluminous objects) are charged exhibiting enzyme-to-enzyme interactions and, in a context of a joint, exhibiting interactions with other molecules in the synovial fluid. Thus, the Langmuir model neglects any type of chemical interaction with the surroundings except the surface. Moreover, a fixed number of adsorption sites are typically approximated on a static surface under equilibrium conditions as per the Langmuir model. But, experimentally the surface of a collagen fibril is dynamic in nature since the number of adsorption sites changes with time as the degradation progresses, and thus, equilibrium is difficult to achieve. The Langmuir model, however, phenomenologically seems to capture the behavior of surface degradation and the associated adsorption sites that not only give a gross estimation of the amount of surface degradation but provide an insight into the degradation mechanisms as well.
Rights and permissions
About this article
Cite this article
Faisal, T.R., Adouni, M. & Dhaher, Y.Y. The effect of fibrillar degradation on the mechanics of articular cartilage: a computational model. Biomech Model Mechanobiol 18, 733–751 (2019). https://doi.org/10.1007/s10237-018-01112-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-018-01112-2