Abstract
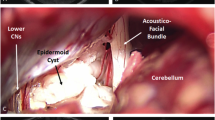
Epidermoid cysts constitute less than 1 % of intracranial tumors with the majority of them involving cerebellopontine angle (CPA). Although several mechanisms for cranial nerve dysfunction due to these tumors have been proposed, no direct evaluation for hyper- or hypoactive dysfunction has been done. In this case series, pathophysiology of cranial nerve dysfunction in CPA epidermoid cysts was evaluated with special attention to a new mechanism of capsule strangulation caused by stratified tumor capsule. Twenty-two cases with epidermoid cysts of CPA micro-neurosurgically treated in our departments since 2005 were reviewed. Clinical status of the patients before the surgery and post-operative functional outcome were recorded. Available data from the English literature were summarized for comparison. Mass reduction of cyst contents in most cases was usually associated with prompt and marked improvement of the symptoms suggesting neuroapraxia caused by compression of the tumor content and/or mild ischemia. Among them, two cases showed strangulation of the affected nerves by the tumor capsule whose preoperative dysfunction did not improve after surgery in spite of meticulous microsurgical removal of the lesion. Involved facial and abducent nerves in these two cases showed distortion of nerve axis and nerve atrophy distal to the strangulation site. We report the first direct evidence of etiology of cranial nerve dysfunction caused by cerebellopontine angle epidermoid tumors. Young age and rapidly progressive neurological deficit might be the characteristics for strangulation of the affected nerves by the cyst capsule. Even though the number of cases might be limited, immediate decompression and release of the strangulating band might be urged in such patients to prevent irreversible deficits.


Similar content being viewed by others
References
Abramson RC, Morawetz RB, Schlitt M (1989) Multiple complications from an intracranial epidermoid cyst: case report and literature review. Neurosurgery 24:574–578
Altschuler EM, Jungreis CA, Sekhar LN, Jannetta PJ, Sheptak PE (1990) Operative treatment of intracranial epidermoid cysts and cholesterol granulomas: report of 21 cases. Neurosurgery 26:606–614
Alvord EC Jr (1977) Growth rates of epidermoid tumors. Ann Neurol 2:367–370
Antoli-Candela F Jr, Stewart TJ (1974) The pathophysiology of otologic facial paralysis. Otolaryngol Clin N Am 7:309–330
Apfelbaum MI (1987) Epidermoid cysts and cholesterol granulomas centered on the posterior fossa: twenty years of diagnosis and management. Neurosurgery 21:805
Bauman CH, Bucy PC (1956) Paratrigeminal epidermoid tumors. J Neurosurg 13:455–468
Berger MS, Wilson CB (1985) Epidermoid cysts of the posterior fossa. J Neurosurg 62:214–219
Committee of Brain Tumor Registry of Japan (2014) Report of brain tumor resistor of Japan (2001–2004). Neurol Med Chir 54(Suppl):9–102
De Souza CE, de Souza R, da Costa S et al (1989) Cerebellopontine angle epidermoid cysts: a report on 30 cases. J Neurol Neurosurg Psychiatry 52:986–990
Gagliardi FM, Vagnozzi R, Caruso R, Delfini R (1980) Epidermoids of the cerebellopontine angle (CPA): usefulness of CT scan. Acta Neurochir (Wien) 54:271–281
Gopalakrishnan CV, Ansari KA, Nair S, Menon G (2014) Long term outcome in surgically treated posterior fossa epidermoids. Clin Neurol Neurosurg 117:93–99
Grant FC, Austin GM (1950) Epidermoids; clinical evaluation and surgical results. J Neurosurg 7(3):190–198
Guidetti B, Gagliardi FM (1977) Epidermoid and dermoid cysts: clinical evaluation and late surgical results. J Neurosurg 47:12–18
Hamel E, Frowein RA, Karimi-Nejad A (1980) Intracranial intradural epidermoids and dermoids. Neurosurg Rev 3:215–219
Hori T, Numata H, Hokama Y, Muraoka K, Tamaki M, Saito Y (1983) Trigeminal pain caused by a parapontine epidermoid cyst. Surg Neurol 19:517–519
Karantanas AH (2001) MR imaging of intracranial epidermoid tumors: specific diagnosis with Turbo-FLAIR pulse sequence. Comput Med Imaging Graph 25:249–255
Kobata H, Kondo A, Iwasaki K, Nishioka T (1998) Combined hyperactive dysfunction syndrome of the cranial nerves: trigeminal neuralgia, hemifacial spasm and glossopharyngeal neuralgia—11-year experience and review. Neurosurgery 43:1351–1362
Kobata H, Kondo A, Iwasaki K (2002) Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: pathogenesis and long-term surgical results in 30 patients. Neurosurgery 50:276–285
Lee SH, Rhee BA, Choi SK, Koh JS, Lim YJ (2010) Cerebellopontine angle tumors causing hemifacial spasm: types, incidence, and mechanism in nine reported cases and literature review. Acta Neurochir (Wien) 152(11):1901–1908
Liu P, Saida Y, Yoshioka H, Itai Y (2003) MR imaging of epidermoids at the cerebellopontine angle. Magn Reson Med Sci 2:109–115
Mallucci CL, Ward V, Carney AS, O’Donoghue GM, Robertson I (1999) Clinical features and outcomes in patients with non-acoustic cerebellopontine angle tumours. J Neurol Neurosurg Psychiatry 66(6):768–771
Mattsson P, Meijer B, Svensson M (1999) Extensive neuronal cell death following intracranial transection of the facial nerve in the adult rat. Brain Res Bull 49:333–341
Mohanty A, Venkatrama SK, Rao BR, Chandramouli BA, Jayakumar PN, Das BS (1997) Experience with cerebellopontine angle epidermoids. Neurosurgery 40(1):24–29
Netsky MG (1988) Epidermoid tumors. Review of literature. Surg Neurol 29:477–483
Obrador S, Lopez-Zafra JJ (1969) Clinical features of the epidermoids of the basal cisterns of the brain. J Neurol Neurosurg Psychiatry 32:450–454
Olivecrona H (1932) On suprasellar cholesteatomas. Brain 55:122–134
Peng Y, Yu L, Li Y, Fan J, Qiu M, Qi S (2014) Pure endoscopic removal of epidermoid tumors of the cerebellopontine angle. Childs Nerv Syst 30(7):1261–1267
Rengachary A, Kishore PRS, Watanabe I (1978) Intradiploic epidermoid cyst of the occipital bone with torcular obstruction. J Neurosurg 48(3):475–478
Rubin G, Scienza R, Pasqualin A, Rosta L, Da Pian R (1989) Craniocerebral epidermoids and dermoids. A review of 44 cases. Acta Neurochir (Wien) 97:1–16
Sabin HI, Bordi LT, Symon L (1987) Epidermoid cysts and cholesterol granulomas centered on the posterior fossa: twenty years of diagnosis and management. Neurosurgery 21:798–805
Safain MG, Dent WC, Heilman CB (2014) An endoscopic assisted retrosigmoid approach to the cerebello-pontine angle for resection of an epidermoid cyst. Neurosurg Focus 36(1 Suppl):1. doi:10.3171/2014
Safavi-Abbasi S, Di Rocco F, Bambakidis N et al (2008) Has management of epidermoid tumors of the cerebellopontine angle improved? A surgical synopsis of the past and present. Skull Base 18(2):85–98
Salazar J, Vaquero J, Saucedo G, Bravo G (1987) Posterior fossa epidermoid cysts. Acta Neurochir 85:34–39
Samii M, Draf W (eds) (1989) Surgery of the skull base. An interdisciplinary approach. Springer-Verlag, Berlin, pp 340–342
Samii M, Tatagiba M, Piquer J, Carvalho GA (1996) Surgical treatment of epidermoid cysts of the cerebellopontine angle. J Neurosurg 84(1):14–19
Schiefer TK, Link MJ (2008) Epidermoids of the cerebellopontine angle: a 20-year experience. Surg Neurol 70(6):584–590
Schroeder HW, Oertel J, Gaab MR (2004) Endoscope-assisted microsurgical resection of epidermoid tumors of the cerebellopontine angle. J Neurosurg 101(2):227–232
Shimamoto Y, Kawase T, Sasaki H, Shiobara R, Yamada F (1999) Anterior transpetrosal approach to the prepontine epidermoids. Skull Base Surg 9(2):75–80
Shulev Y, Trashin A, Gordienko K (2011) Secondary trigeminal neuralgia in cerebellopontine angle tumors. Skull Base 21(5):287–294
Talacchi A, Sala F, Alessandrini F, Turazzi S, Bricolo A (1998) Assessment and surgical management of posterior fossa epidermoid tumors: report of 28 cases. Neurosurgery 42(2):242–251
Tsuruda JS, Chew WM, Moseley ME, Norman D (1990) Diffusion-weighted MR imaging of the brain: value of differentiating between extraaxial cysts and epidermoid tumors. AJR Am J Roentgenol 155:1059–1065
Ulrich J (1964) Intracranial epidermoids. A study on their distribution and spread. J Neurosurg 21:1051–1058
Vinchon M, Pertuzon B, Lejeune JP, Assaker R, Pruvo JP, Christiaens JL (1995) Intradural epidermoid cysts of the cerebellopontine angle: diagnosis and surgery. Neurosurgery 36(1):52–56
Wakabayashi T, Tamaki N, Satoh H, Matsumoto S (1983) Epidermoid tumor presenting as painful tic convulsif. Surg Neurol 19(3):244–246
Yamakawa K, Shitara N, Genka S, Manaka S, Takakura K (1989) Clinical course and surgical prognosis of 33 cases of intracranial epidermoid tumors. Neurosurgery 24:568–573
Yasargil MG, Abernathey CD, Sarioglu AÇ (1989) Microsurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery 24:561–567
Acknowledgments
The authors confirm that no governmental, institutional, or industrial fund or grant was given for the material of this study or to support any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Kazunari Yoshida, Tokyo, Japan
The symptoms of the brain tumor usually occur by compression or destruction of the neural tissue by the tumor mass. Epidermoid cysts in the cerebellopontine angle (CPA) are known to present variable dysfunction of the cranial nerves, including hemifacial spasm, trigeminal neuralgia, and variable cranial nerve palsy. The distinct finding, described in this manuscript, is that the mechanism of the cranial nerve dysfunction in some cases is the nerve degeneration of the distal to the strangulation site by the tumor capsule. Nobody has recognized this type of the mechanism of the cranial nerve dysfunction so far. Dr. Hasegawa and his colleagues have clearly demonstrated this mechanism of the cranial nerve dysfunction in cases of the CPA epidermoid cysts. We should notice this mechanism of the cranial nerve dysfunction and decide the appropriate timing of the management of these tumors.
Henry W. S. Schroeder, Greifswald, Germany
The authors report their experience with the microsurgical treatment of 22 CPA epidermoids. The discussion of the mechanisms of the cranial nerve deficits is interesting. In two of their patients, the authors found a strangulation of the facial and abducent nerve respectively. Although the neurological deficits improved in most of the patients, in the two patients with strangulation of the nerve, there was no satisfying improvement. The authors conclude that in the case of rapidly developing cranial nerve palsy, early surgical intervention is required to increase the chance of recovery of the cranial nerve function. This is an interesting finding that has not frequently been reported in the literature. In our series, the cranial nerve dysfunction was caused by nerve compression and distortion, but we never observed such a strangulation as described by the authors. Early nerve decompression seems to be very reasonable in case of a rapid neurological deficit.
I agree that gross total removal of the epidermoid including the cyst capsule should be the aim of the surgery for epidermoids. I always try a very aggressive resection of the cyst capsule. However, in most patients, I had to leave a small portion of the capsule behind because it was very adherent to the nerves, vessels, or brain stem. Mostly, in virgin cases, that was only a very tiny part (a few square millimeters), sometimes even at only one location in the surgical field. This is referred to as near total resection.
The authors stated that in case of contralateral or supratentorial tumor extension, the tumor would be resected through the ipsilateral corridor as much as possible and the contralateral remnant would be followed for any symptomatic or radiological growth. In epidermoid resections, I almost always use endoscope assistance to increase the rate of total removal of the cyst contents. With 30° or 45° endoscopes, one may look around the tentorium or the brain stem to the contralateral side and remove the residual tumor under endoscopic visualization in a safe way. Additionally, I found the endoscope very helpful to remove extensions of the epidermoid located in Meckel’s cave.
Thomas Kretschmer, Oldenburg, Germany
The paper’s emphasis is on a considerable case series of CP-angle epidermoids with evaluation of functional outcome and correlation to intraoperative findings. This is compared to the pertinent literature. As such, the reader finds condensed information on clinical findings, functional deficits and expectable outcomes from microsurgery. An additional mechanism for cranial nerve deficit other than neurapraxia is identified and introduced: namely “strangulation” of CN. The proposed mechanism is detailed by two cases. As the functional results in these cases were that CNs were unfavorable and distinct from other cases, the authors drew the following conclusion: A rapidly progressive CN deficit in a young patient with CP-angle epidermoid is suggestive of a strangulation mechanism. In such cases early surgery is recommended.
This is an interesting observation in a large case series, which was nicely worked-up for outcome and compared to existing series. The paper adds to our knowledge about cp-angle epidermoid, congratulation.
Rights and permissions
About this article
Cite this article
Hasegawa, M., Nouri, M., Nagahisa, S. et al. Cerebellopontine angle epidermoid cysts: clinical presentations and surgical outcome. Neurosurg Rev 39, 259–267 (2016). https://doi.org/10.1007/s10143-015-0684-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0684-5