Abstract
Fluorescein is widely used as a fluorescent tracer for many applications. Its capacity to accumulate in cerebral areas where there has been blood–brain barrier damage makes it particularly suitable as a dye for the intraoperative visualization of malignant gliomas (MGs). In this report, we describe the results of a comprehensive review on the use of fluorescein in the surgical treatment of MGs. A comprehensive literature search and review for English-written articles concerning the use of fluorescein in the resection of MGs has been conducted. The search was executed through a PubMed literature search using the following keywords: malignant gliomas, glioblastomas, high-grade gliomas, YELLOW 560, total removal, dedicated filter, neurosurgery, brain tumors, intracranial tumors, and confocal microscopy. The literature search resulted in the retrieval of 412 evidence-based articles. Of these, 17 were found to be strictly related to the resection of MG with the aid of fluorescein. In addition to these 17, we have included 2 articles derived from a personal database of the corresponding author (FA). The analysis of the articles reviewed revealed three major applications of fluorescein during surgery for MGs that was documented: Fluorescein-guided resection of MGs with white-light illumination, fluorescein-guided resection of MGs with a surgical microscope equipped with a dedicated filter for fluorescein, and confocal microscopy for intraoperative histopathological analysis on MGs. The systemic review conducted on the use of fluorescein in MGs explored the applications and the different modalities in which fluorescein has been used. The data we have gathered indicates that fluorescein-guided surgery is a safe, effective, and convenient technique to achieve a high rate of total removal in MGs. Further prospective comparative trials, however, are still necessary to prove the impact of fluorescein-guided surgery on both progression-free survival and overall survival.


Similar content being viewed by others
References
Acerbi F, Broggi M, Eoli M, Anghileri E, Cuppini L, Pollo B, Schiariti M, Visintini S, Orsi C, Franzini A, Broggi G, Ferroli P (2013) Fluorescein-guided surgery for grade IV gliomas with a dedicated filter on the surgical microscope: preliminary results in 12 cases. Acta Neurochir (Wien) 155(7):1277–1286
Belcher EH, Evans HD (1951) The localization of cerebral tumours with radioactive derivatives of fluorescein; physical limitations. Br J Radiol 24(281):272–279
Chen B, Wang H, Ge P, Zhao J, Li W, Gu H, Wang G, Luo Y, Chen D (2012) Gross total resection of glioma with the intraoperative fluorescence-guidance of fluorescein sodium. Int J Med Sci 9(8):708–714
Díez Valle R, Tejada Solis S, Idoate Gastearena MA, García de Eulate R, Domínguez Echávarri P, Aristu Mendiroz J (2011) Surgery guided by 5-aminolevulinic fluorescence in glioblastoma: volumetric analysis of extent of resection in single-center experience. J Neurooncol 102(1):105–113
Dilek O, Ihsan A, Tulay H (2011) Anaphylactic reaction after fluorescein sodium administration during intracranial surgery. J Clin Neurosci 18(3):430–431
Dunbar KB, Canto MI (2010) Confocal laser endomicroscopy in Barrett’s esophagus and endoscopically inapparent Barrett’s neoplasia: a prospective, randomized, double-blind, controlled, crossover trial. Gastrointest Endosc 72(3):668
Eschbacher J, Martirosyan NL, Nakaji P, Sanai N, Preul MC, Smith KA, Coons SW, Spetzler RF (2012) In vivo intraoperative confocal microscopy for real-time histopathological imaging of brain tumors. J Neurosurg 116(4):854–860
Ferroli P, Acerbi F, Albanese E, Tringali G, Broggi M, Franzini A, Broggi G (2011) Application of intraoperative indocyanine green angiography for CNS tumors: results on the first 100 cases. Acta Neurochir Suppl 109:251–257
Ferroli P, Acerbi F, Tringali G, Albanese E, Broggi M, Franzini A, Broggi G (2011) Venous sacrifice in neurosurgery: new insights from venous indocyanine green videoangiography. J Neurosurg 115(1):18–23
Hammoud MA, Ligon BL, ElSouki R, Shi WM, Schomer DF, Sawaya R (1996) Use of intraoperative ultrasound for localizing tumours and determining the extent of resection: a comparative study with magnetic resonance imaging. J Neurosurg 84:737–741
Hurlstone DP, Tiffin N, Brown SR, Baraza W, Thomson M, Cross SS (2008) In vivo confocal laser scanning chromo-endomicroscopy of colorectal neoplasia: changing the technological paradigm. Histopathology 52:417–426
Kabuto M, Kubota T, Kobayashi H, Nakagawa T, Ishii H, Takeuchi H, Kitai R, Kodera T (1997) Experimental and clinical study of detection of glioma at surgery using fluorescent imaging by a surgical microscope after fluorescein administration. Neurol Res 19(1):9–16
Kiesslich R, Gossner L, Goetz M, Dahlmann A, Vieth M, Stolte M, Hoffman A, Jung M, Nafe B, Galle PR, Neurath MF (2006) In vivo histology of Barrett’s esophagus and associated neoplasia by confocal laser endomicroscopy. Clin Gastroenterol Hepatol 4:979–987
Koc K, Anik I, Cabuk B, Ceylan S (2008) Fluorescein sodium-guided surgery in glioblastoma multiforme: a prospective evaluation. Br J Neurosurg 22(1):99–103
Kubben PL, ter Meulen KJ, Schijns OE, ter Laak-Poort MP, van Overbeeke JJ, van Santbrink H (2011) Intraoperative MRI-guided resection of glioblastoma multiforme: a systematic review. Lancet Oncol 12(11):1062–1070
Kuhnt D, Becker A, Ganslandt O, Bauer M, Buchdelferd M, Nimsky C (2011) Correlation of the extent of tumor volume resection and patient survival in surgery of glioblastoma multiforme with high-field intraoperative MRI guidance. Neuro Oncol 13(12):1339–1348
Kuroiwa T, Kajimoto Y, Ohta T (1999) Surgical management for supratentorial astrocytic tumors. Minim Invasive Neurosurg 42(4):182–186
Kuroiwa T, Kajimoto Y, Ohta T (1999) Comparison between operative findings on malignant glioma by a fluorescein surgical microscopy and histological findings. Neurol Res 21(1):130–134
Kuroiwa T, Kajimoto Y, Ohta T (1998) Development of a fluorescein operative microscope for use during malignant glioma surgery: a technical note and preliminary report. Surg Neurol 50(1):41–48
Kwan AS, Barry C, McAllister IL, Constable I (2006) Fluorescein angiography and adverse drug reactions revisited: the Lions Eye experience. Clin Exp Ophthalmol 34(1):33–38
Kwiterovich KA, Maguire MG, Murphy RP, Schachat AP, Bressler NM, Bressler SB, Fine SL (1991) Frequency of adverse systemic reactions after fluorescein angiography. Results of a prospective study. Ophthalmology 98(7):1139–1142
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, Lang FF, McCutcheon IE, Hassenbush SJ, Holland E, Hess K, Michael C, Miller D, Sawaya R (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95(2):190–198
Litofsky NS, Bauer AM, Kasper RS, Sullivan CM, Dabbous OH (2006) Image-guided resection of high-grade glioma: patient selection factors and outcome. Neurosurg Focus 20(3):E16
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (2007) IARC WHO Classification of tumours of the central nervous system International Agency for Research on Cancer. World Health Organization, Lyon
McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, Weingart JD, Brem H, Quinones-Hinojosa AR (2009) Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg 110(1):156–162
Moore GE, Peyton WT, French LA, Walker WW (1948) The clinical use of fluorescein in neurosurgery; the localization of brain tumors. J Neurosurg 5(4):392–398
Moore GE (1947) Fluorescein as an agent in the differentiation of normal and malignant tissues. Science 106(2745):130–131
Murray KJ (1982) Improved surgical resection of human brain tumors: part I. A preliminary study. Surg Neurol 17(5):316–319
Nimsky C, Ganslandt O, Buchfelder M, Fahlbush R (2006) Intraoperative visualization for resection of gliomas: the role of functional neuronavigation and intraoperative 1.5T MRI. Neurol Res 28(5):482–487
Novtny HR, Alvis DL (1961) A method of photographing fluorescence in circulating blood in the human retina. Circulation 24:82–86
Okuda T, Yoshioka H, Kato A (2012) Fluorescence-guided surgery for glioblastoma multiforme using high-dose fluorescein sodium with excitation and barrier filters. J Clin Neurosci 19(12):1719–1722
Sanai N, Eschbacher J, Hattendorf G, Coons SW, Preul MC, Smith KA, Nakaji P, Spetzler RF (2011) Intraoperative confocal microscopy for brain tumors: a feasibility analysis in humans. Neurosurgery 68(2 Suppl Operative):282–290
Sankar T, Delaney PM, Ryan RW, Eschbacher J, Abdelwahab M, Nakaji P, Coons SW, Scheck AC, Smith KA, Spetzler RF, Preul MC (2010) Miniaturized handheld confocal microscopy for neurosurgery: results in an experimental glioblastoma model. Neurosurgery 66(2):410–417
Schebesch KM, Proescholdt M, H√∂hne J, Hohenberger C, Hansen E, Riemenschneider MJ, Ullrich W, Doenitz C, Schlaier J, Lange M, Brawanski A (2013) Sodium fluorescein-guided resection under the YELLOW 560 nm surgical microscope filter in malignant brain tumor surgery-a feasibility study. Acta Neurochir (Wien) 155(4):693–699
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12(11):997–1003
Shinoda J, Yano H, Yoshimura S, Okumura A, Kaku Y, Iwama T, Sakai N (2003) Fluorescence-guided resection of glioblastoma multiforme by using high-dose fluorescein sodium. Technical note. J Neurosurg 99(3):597–603
Stummer W, Meinel T, Ewelt C, Martus P, Jakobs O, Felsber J, Reifenberger G (2012) Prospective cohort study of radiotherapy with concomitant and adjuvant temozolomide chemotherapy for glioblastoma patients with no or minimal residual enhancing tumor load after surgery. J Neurooncol 108(1):89–97
Stummer W, Novotny A, Stepp H, Goetz C, Bise K, Reulen HJ (2000) Fluorescence-guided resection of glioblastoma multiforme by using 5-aminolevulinic acid-induced porphyrins: a prospective study in 52 consecutive patients. J Neurosurg 93(6):1003–1013
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen HJ (2006) Fluorescence-guided surgery with 5- aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol 7(5):392–401
Stummer W, Stocker S, Novotny A, Heimann A, Sauer O, Kempski O, Plesnila N, Wietzorrek J, Reulen HJ (1998) In vitro and in vivo porphyrin accumulation by C6 glioma cells after exposure to 5-aminolevulinic acid. J Photochem Photobiol B 45(2–3):160–169
Stummer W, Stocker S, Wagner S, Stepp H, Fritsch C, Goetz AE, Kiefmann R, Reulen HJ (1998) Intraoperative detection of malignant gliomas by 5-aminolevulinic acid-induced porphyrin fluorescence. Neurosurgery 42(3):518–526
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
Svien HJ, Johnson AB (1951) Fluorescein in the localization of brain tumors. Proc Staff Meet Mayo Clin 26(8):142–150
Tan J, Quinn MA, Pyman JM, Delaney PM, McLaren WJ (2009) Detection of cervical intraepithelial neoplasia in vivo using confocal endomicroscopy. BJOG 116:1663–1670
Tanahashi S, Lida H, Dohi S (2006) An anaphylactoid reaction after administration of fluorescein sodium during neurosurgery. Anesth Analg 103(2):503
Tonn JC, Stummer W (2008) Fluorescence-guided resection of malignant gliomas using 5-aminolevulinic acid: practical use, risks, and pitfalls. Clin Neurosurg 55:20–26
Unsgaard G, Ommedal S, Muller T, Gronningsaeter A, Nagelhus Hernes TA (2002) Neuronavigation by intraoperative three-dimensional ultrasound: initial experience during brain tumor resection. Neurosurgery 50(4):804–812
Wiesner C, Jäger W, Salzer A, Biesterfeld S, Kiesslich R, Hampel C, Thüroff JW, Goetz M (2011) Confocal laser endomicroscopy for the diagnosis of urothelial bladder neoplasia: a technology of the future? BJU Int 107:399–403
Wirtz CR, Albert FK, Schwaderer M, Heuer C, Staubert A, Tronnier VM, Knauth M, Kunze S (2000) The benefit of neuronavigation for neurosurgery analyzed by its impact on glioblastoma surgery. Neurol Res 22(4):354–360
Yannuzzi LA, Rohrer KT, Tindel LJ, Sobel RS, Costanza MA, Shields W, Zang E (1986) Fluorescein angiography complication survey. Ophthalmology 93(5):611–617
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Peter Nakaji, Phoenix, USA
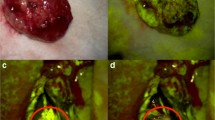
In this review, Acerbi et al. from Paolo Ferroli’s group at the Besta in Milan describe the literature and their personal experience using fluorescein as a fluorophore to guide the resection of malignant gliomas. This technique involves the preoperative injection of intravenous fluorescein and subsequent visualization under a microscope designed to detect fluorescence in the 560 nm range. The brain lights up in yellow under white-light visualization and, generally, the tumor lights up even more, although it varies. This is where things get interesting. Fluorescein is a non-specific fluorophore whose concentration in the tumor relies upon the increased vascular permeability of the tumor compared to normal brain. The advantage of fluorescein compared to metabolized fluorophores such as 5-ALA is that it can be seen while still in the unaugmented visual range, allowing the surgeon to operate and still see the whole surgical field. The tumor generally does appear even brighter yellow. The hope of all of us who are working with fluorescein is that it can be used to guide resection. The underlying premise of cytoreductive surgery is that a lower volume of tumor correlates with better control of the tumor. While there is evidence for this, there is both nuanced debate on this subject and the concern that increased resection in some locations will entail greater risk of deficit, with attendant impact on both survival and functional outcome. These challenges face not only fluorescein-guided resection of malignant gliomas but also all resection guided by intraoperative adjuncts, whether they be visual indicators such as 5-ALA, image guidance, ultrasound, asleep mapping, awake surgery, or endomicroscopes. The principal advantage gained in the use of these agents is if they improve our resection of the marginal tissue whose appearance blends with normal brain. Fluorescein is fairly non-specific, but with experience, there is mounting reason to think that it can help us make this particular distinction. Consideration of the merits of fluorescein immediately invites a deeper comparison with 5-ALA. 5-ALA is a prodrug which is used in the heme synthesis pathway, and in most gliomas, undergoes conversion into protoporphyrin IX, which fluoresces in the 400-nm (ultraviolet) range. It is more specific in the sense that tumor cells preferentially metabolize it, and therefore, it is concentrated in the target tissue. In theory, high specificity of a dye for the tumor is advantageous, but as tumor cells are always found beyond the visible margin, macrofluorescence alone may drive under-resection. At the same time, careful removal of only macrofluorescent tumor also may not be enough to prevent deficits, if the normal tissue is so closely entwined with the tumor that its manipulation alone mandates tampering with eloquent structures. The debate continues on. Perhaps the best role for these agents is in limiting the unintentional leaving of small amounts of residual tumor in non-eloquent areas.
In practical terms, fluorescein has advantages that are considerable for intraoperative use. Fluorescein is a molecule with a long history of safe human administration and a low cost around the world. As the authors recognize, questions about fluorescein remain. The exact dose and timing that is optimal remain to be worked out. The normal brain does fluoresce somewhat; the threshold for distinguishing tumor from brain from necrosis has yet to be firmly established and to be rigorously confirmed through correlative histology.
In the future, surgery may benefit from fluorophores that are highly specific to high-grade glioma—and indeed to any other type of tumor—helping surgeons to identify more accurately what is tumor and what is not, while other technologies tell us whether that tissue can be removed safely. In the meantime, this kind of intermediate technology has advantages that bear continued exploration as the authors and others are doing.
ᅟ
Andreas Raabe, Bern, Switzerland
This interesting article reviews the use of sodium fluorescein as a dye to visualize tumor tissue during surgery of malignant gliomas. These invasive and often poorly delineated tumors may be “gross total resection (GTR)” eligible, or more precisely, “complete resection of enhancing tumor (CRET)” eligible in many cases, but GTR or CRET are achieved in a disappointingly low percentage of patients only. Depending on the selection of patients, this percentage ranges from 20 to 60 % even when neuronavigation or intraoperative ultrasound is used. The only “resection enhancing” technologies that are proven to detect concealed tumor tissue are intraoperative MRI and fluorescence imaging, both of which were shown to increase the CRET rate in eligible glioblastoma patients to 65 to 95 %.
Sodium fluorescein fluorescence is a promising technology for glioblastoma surgery. The integration of a specific yellow light filter into the surgical microscope makes it a straightforward intraoperative technique. The experience and images suggest that this method adds to the surgical artillery that improves the extent of resection. However, as the authors emphasize, hard data are still missing, and a randomized controlled trial comparing white-light and sodium fluorescein is needed to quantify the effect on glioblastoma surgery.
In my view, different methods have different advantages, and the surgeon should have all of them in his or her toolbox to decide what is best for any given situation and patient. When 5-ALA and sodium fluorescein are compared in this review, we should keep in mind that most data about the latter technique are from single-center retrospective studies. Although I agree with the authors that this technology has the potential to increase the extent of resection, the numbers in Table 3 are somewhat biased in favor of the authors’ method and remain to be proven.
How much tumor tissue is included in the sodium fluorescein fluorescence remains unclear. While 5-ALA is metabolized within the tumor cell, sodium fluorescein appearance in the glioma tissue depends on blood–brain-barrier (BBB) leakage. Taking contrast-enhanced MRI as a marker for BBB damage, we expect that this is the volume stained with extracellular sodium fluorescein. In contrast, intracellularly metabolized 5-ALA fluorescence is found beyond the BBB-damaged tumor volume, and the tissue volume resected with 5-ALA is indeed larger than the T1-gadolinium-enhancing tumor [1]. A methodological advantage of sodium fluorescein over 5-ALA is unlikely; however, the low price for this drug may be a deciding factor in many countries.
References
1. Schucht P, Knittel S, Slotboom J, Seidel K, Murek M, Jilch A, Raabe A, Beck J (2014) 5-ALA complete resections go beyond MR contrast enhancement: shift corrected volumetric analysis of the extent of resection in surgery for glioblastoma. Acta Neurochir (Wien) 156(2):305–12
ᅟ
Walter Stummer, Münster, Germany
I gladly grasp the opportunity to write a comment to the review of Dr. Acerbi and co-workers which is being published in Neurosurgical Review on the use of fluorescein sodium for enhancing surgery of malignant gliomas.
Fluorescein sodium has been around a while and was first used by Moore et al. 1948 [1] for finding gliomas when CT and MRI was still science fiction at best. Even in those early reports, the authors were aware of the lack of selectivity of fluorescein for these malignant tumors, noting that a “brilliant yellow-green fluorescence characterizes tumor tissue whereas the normal brain, which retains appreciably less dye, appears white. Edematous tissue surrounding the tumor does fluoresce, but to a lesser degree so that it can be readily separated both from normal brain and the tumor itself.” The senior neurosurgeons reading this comment will remember that after the reports by Moore and his colleagues, fluorescein has not found its way into neurosurgery, but was initially abandoned.
A second round with fluorescein occurred in the late 1990s by Kuoriwa and co-workers from Japan, and three publications can be found by this group, the last in 1999 [2, 3, 4]. This group has also stopped using fluorescein sodium, switching to ALA. To date, they have published a considerable number of articles on malignant gliomas and ALA, the last in 2013 [5, 6, 7, 8, 9, 10, 11, 12].
So why did surgeons not continue using fluorescein sodium for brain tumor surgery? The answer is simple. Fluorescein sodium is hardly specific for tumor because it is a blood-borne dye. Wherever there is blood, there will be fluorescein. Is this a good basis for the surgeon to rely upon for intraoperative tumor identification?
So today, we are seeing a second renaissance of fluorescein sodium, as reflected by the present review. But what is new? It is certainly not the biology of the dye. Fluorescein sodium is still located in the blood and leaks into the tumor through the broken down blood–brain barrier.
What is new is that a novel filter system is available, the Yellow 560 filter, which is now being provided to the community by a microscope company. In contrast to older systems, which visualized yellow fluorescein fluorescence on a black background, this filter system retains background tissue information. What the surgeon sees is (almost) the normal brain and the superimposed fluorescein signal. Please note that this system is superb for vascular surgery, and in this particular context, a real advance. With the new system, the surgeon does not have to rely on the playback on an external video screen with the established indocyanine green (ICG), because ICG fluorescence is invisible to the human eye. As opposed to ICG, fluorescein fluorescence in vessels is clearly visible to the human eye. Thus, the surgeon can directly inspect and manipulate the vessels, which is a real advantage, and extravasated fluorescein is not of importance.
But is fluorescein sodium with this filter also reliable for tumor surgery? As a matter of fact, the image initially appears nice, with the brain being beautifully visible in the background, and the fluorescein fluorescence appearing somewhat selective in the foreground. But be careful; this image is deceptive, since much of the weaker and aberrant fluorescein signal in vessels, edema, and blood in the cavity is now obscured by the additional, bright tissue background information, particularly in the late stages of surgery where discrimination becomes especially important. Normally, with fluorescence, the background is maintained dark to not lose the information that fluorescence conveys. In the context of the YELLOW 560 filter, the surgeon believes he is receiving selective information, where in fact, he is only seeing peak fluorescence. The filter system simply does not change the biology of the dye in the blood. The reader may wish to see an example of the use of fluorescein for glioma surgery in a video posted on abcNEWS and freely available (http://abcnews.go.com/Health/making-brain-tumors-glow-saves-lives/story?id=17076243). Please note the fluorescein, which is in all vessels, is distributed weakly throughout the normal brain and is visible in the dura, the CSF, especially at the resection edge due to tissue injury, and even in the remote brain locations obviously injured during the course of resection.
The reader of the review by Dr. Acerbi and co-workers should give this aspect some thought, as he should critically give thought to the authors’ assertion that fluorescein is so much cheaper than ALA, which is true. However, fluorescein has not been tested in expensive randomized GCP conform clinical studies for safety and efficacy in many hundreds of patients, as was ALA, nor has it been approved for brain tumor surgery, as is ALA. In all studies, so far fluorescein has been used off-label. This in itself bears a number of implications. The authors do not mention this important aspect, and the uncritical user should be well aware of this, especially if his patients experience ill side effects of fluorescein, which have been reported [13].
In the end, the authors themselves acknowledge the necessity of controlled clinical studies to elucidate safety and value of fluorescein in conjunction with novel technology. The community is certainly looking forward to those studies in the ongoing effort to increase the quality of our surgical care while keeping economical restraints in mind.
References
1. Moore GE, Peyton WT, French LA, Walker, WW. The clinical use of fluorescein in neurosurgery; the localization of brain tumors. J Neurosurg. 1948 Jul;5(4):392–8. PubMed PMID: 18872412.
2. Kuroiwa T, Kajimoto Y, Ohta T. Surgical management for supratentorial astrocytic tumors. Minim Invasive Neurosurg. 1999 Dec;42(4):182–6. PubMed PMID: 10667822.
3. Kuroiwa T, Kajimoto Y, Ohta T. Comparison between operative findings on malignant glioma by a fluorescein surgical microscopy and histological findings. Neurol Res. 1999 Jan;21(1):130–4. PubMed PMID: 10048072.
4. Kuroiwa T, Kajimoto Y, Ohta T. Development of a fluorescein operative microscope for use during malignant glioma surgery: a technical note and preliminary report. Surg Neurol. 1998 Jul;50(1):41–8; discussion 48–9. PubMed PMID: 9657492.
5. Kuroiwa T, Kajimoto Y, Furuse M, Miyatake S. A surgical loupe system for observing protoporphyrin IX fluorescence in high-grade gliomas after administering 5-aminolevulinic acid. Photodiagnosis Photodyn Ther. 2013 Dec;10(4):379–81. doi: 10.1016/j.pdpdt.2013.03.004. Epub 2013 May 2. PubMed PMID: 24284089.
6. Masubuchi T, Kajimoto Y, Kawabata S, Nonoguchi N, Fujishiro T, Miyatake S, Kuroiwa T. Experimental study to understand nonspecific protoporphyrin IX fluorescence in brain tissues near tumors after 5-aminolevulinic acid administration. Photomed Laser Surg. 2013 Sep;31(9):428–33. doi: 10.1089/pho.2012.3469. Epub 2013 Jul 20. PubMed PMID: 23869519.
7. Sun W, Kajimoto Y, Inoue H, Miyatake S, Ishikawa T, Kuroiwa T. Gefitinib enhances the efficacy of photodynamic therapy using 5-aminolevulinic acid in malignant brain tumor cells. Photodiagnosis Photodyn Ther. 2013 Feb;10(1):42–50. doi: 10.1016/j.pdpdt.2012.06.003. Epub 2012 Jul 20. PubMed PMID: 23465372.
8. Takahashi K, Ikeda N, Nonoguchi N, Kajimoto Y, Miyatake S, Hagiya Y, Ogura S, Nakagawa H, Ishikawa T, Kuroiwa T. Enhanced expression of coproporphyrinogen oxidase in malignant brain tumors: CPOX expression and 5-ALA-induced fluorescence. Neuro Oncol. 2011 Nov;13(11):1234–43. doi: 10.1093/neuonc/nor116. Epub 2011 Aug 8. Retraction in: Neuro Oncol. 2013 Jul;15(7):969. PubMed PMID: 21824890; PubMed Central PMCID: PMC3199158.
9. Miyatake S, Kajimoto Y, Kuroiwa T. [Intraoperative photo-dynamic diagnosis of brain tumors]. Brain Nerve. 2009 Jul;61(7):835–42. Review. Japanese. PubMed PMID: 19618861.
10. Miyatake S, Kuroiwa T, Kajimoto Y, Miyashita M, Tanaka H, Tsuji M. Fluorescence of non-neoplastic, magnetic resonance imaging-enhancing tissue by 5-aminolevulinic acid: case report. Neurosurgery. 2007 Nov;61(5):E1101-3; discussion E1103-4. PubMed PMID: 18091261.
11. Kajimoto Y, Kuroiwa T, Miyatake S, Ichioka T, Miyashita M, Tanaka H, Tsuji M. Use of 5-aminolevulinic acid in fluorescence-guided resection of meningioma with high risk of recurrence. Case report. J Neurosurg. 2007 Jun;106(6):1070–4. PubMed PMID: 17564181.
12. Tamura Y, Kuroiwa T, Kajimoto Y, Miki Y, Miyatake S, Tsuji M. Endoscopic identification and biopsy sampling of an intraventricular malignant glioma using a 5-aminolevulinic acid-induced protoporphyrin IX fluorescence imaging system. Technical note. J Neurosurg. 2007 Mar;106(3):507–10. PubMed PMID: 17367078.
13. Dilek O, Ihsan A, Tulay H. Anaphylactic reaction after fluorescein sodium administration during intracranial surgery. J Clin Neurosci. 2011 Mar;18(3):430–1. doi: 10.1016/j.jocn.2010.06.012. Epub 2011 Jan 14. PubMed PMID: 21237654.
Rights and permissions
About this article
Cite this article
Acerbi, F., Cavallo, C., Broggi, M. et al. Fluorescein-guided surgery for malignant gliomas: a review. Neurosurg Rev 37, 547–557 (2014). https://doi.org/10.1007/s10143-014-0546-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0546-6