Abstract
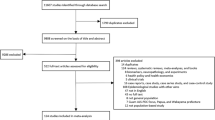
Multidisciplinary care (MDC) has been the most recommended approach for symptom management in amyotrophic lateral sclerosis (ALS) but there is conflicting evidence about its effectiveness on survival and quality of life (QoL) of ALS patients. We conducted a systematic review to determine the effects of multidisciplinary care compared to general neurological care in survival and quality of life of ALS patients. A comprehensive literature search using Scopus, MEDLINE-PubMed, Cochrane, Web of Science, PEDro, and Science Direct was undertaken. Studies related to multidisciplinary care or general neurological care in ALS patients that assessed survival and quality of life and were published in the period up to and including January 2020 were included. A total of 1192 studies were initially identified, but only 6 were included. All studies that investigated survival showed and advantage of MDC over NC, and this benefit was even greater for bulbar onset patients. A meta-analysis was performed and showed a mean difference of 141.67 (CI 95%, 61.48 to 221.86), indicating that patients who received MDC had longer survival than those who underwent NC (p = 0.0005). Concerning QoL, only one study found better mental health scores related to QoL for patients under MDC. Multidisciplinary care is more effective than general neurology care at improving survival of patients with ALS, but only improves mental health outcomes related to quality of life of these patients.


Similar content being viewed by others
Data availability
Not applicable.
References
Hardiman O, Al-Chalabi A, Chio A et al (2017) Amyotrophic lateral sclerosis. Nat Rev Dis Prim 3:1–19. https://doi.org/10.1038/nrdp.2017.71
Wobst HJ, Mack KL, Brown DG, Brandon NJ, Shorter J (2020) The clinical trial landscape in amyotrophic lateral sclerosis—past, present, and future. Med Res Rev 40:1352–1384
Logroscino G, Piccininni M (2019) Neuroepidemiology of aging-review amyotrophic lateral sclerosis descriptive epidemiology: the origin of geographic difference keywords amyotrophic lateral sclerosis Population-based study · cohort · registries · Global Burden of Disease · C9ORF72 · Incidence · Ancestry · Ethnicity · Geographic gradient. https://doi.org/10.1159/000493386
Longinetti E, Fang F (2019) Epidemiology of amyotrophic lateral sclerosis: An update of recent literature. Curr Opin Neurol 32:771–776. https://doi.org/10.1097/WCO.0000000000000730
Dorst J, Chen L, Rosenbohm A, Dreyhaupt J, Hübers A, Schuster J, Weishaupt JH, Kassubek J, Gess B, Meyer T, Weyen U, Hermann A, Winkler J, Grehl T, Hagenacker T, Lingor P, Koch JC, Sperfeld A, Petri S, Großkreutz J, Metelmann M, Wolf J, Winkler AS, Klopstock T, Boentert M, Johannesen S, Storch A, Schrank B, Zeller D, Liu XL, Tang L, Fan DS, Ludolph AC (2019) Prognostic factors in ALS: a comparison between Germany and China. J Neurol 266:1516–1525. https://doi.org/10.1007/s00415-019-09290-4
Jun KY, Park J, Oh KW, Kim EM, Bae JS, Kim I, Kim SH (2019) Epidemiology of ALS in Korea using nationwide big data. J Neurol Neurosurg Psychiatry 90:395–403. https://doi.org/10.1136/jnnp-2018-318974
The WHOQOL group (1995) The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc Sci Med 41:1403–1409. https://doi.org/10.1016/0277-9536(95)00112-K
Simmons Z (2015) Patient-Perceived Outcomes and Quality of Life in ALS. Neurotherapeutics 12:394–402. https://doi.org/10.1007/s13311-014-0322-x
Maessen M, Veldink JH, Onwuteaka-Philipsen BD, de Vries JM, Wokke JHJ, van der Wal G, van den Berg LH (2009) Trends and determinants of end-of-life practices in ALS in the Netherlands. Neurology 73:954–961. https://doi.org/10.1212/WNL.0b013e3181b87983
Craig A, Dzeng E (2018) How should physicians care for dying patients with amyotrophic lateral sclerosis? AMA J Ethics 20:690–698. https://doi.org/10.1001/amajethics.2018.690
Andersen PM, Abrahams S, Borasio GD et al (2012) EFNS guidelines on the Clinical Management of Amyotrophic Lateral Sclerosis (MALS) - revised report of an EFNS task force. Eur J Neurol 19:360–375. https://doi.org/10.1111/j.1468-1331.2011.03501.x
Hogden A, Foley G, Henderson RD, James N, Aoun S (2017) Amyotrophic lateral sclerosis: improving care with a multidisciplinary approach. J Multidiscip Healthc 10:205–215
De Carvalho M, Gooch CL (2017) The yin and yang of gastrostomy in the management of ALS. Neurology 89:1435–1436
Dharmadasa T, Kiernan MC (2018) Riluzole, disease stage and survival in ALS. Lancet Neurol 17:385–386
Dorst J, Ludolph AC (2019) Non-invasive ventilation in amyotrophic lateral sclerosis. Ther Adv Neurol Disord 12:1756286419857040
Chiò A, Bottacchi E, Buffa C, Mutani R, Mora G, PARALS (2006) Positive effects of tertiary centres for amyotrophic lateral sclerosis on outcome and use of hospital facilities. J Neurol Neurosurg Psychiatry 77:948–950. https://doi.org/10.1136/jnnp.2005.083402
Miller RG, Jackson CE, Kasarskis EJ et al (2009) Practice Parameter update: the care of the patient with amyotrophic lateral sclerosis: Multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 73:1227–1233. https://doi.org/10.1212/WNL.0b013e3181bc01a4
Martin S, Trevor-Jones E, Khan S, Shaw K, Marchment D, Kulka A, Ellis CE, Burman R, Turner MR, Carroll L, Mursaleen L, Leigh PN, Shaw CE, Pearce N, Stahl D, al-Chalabi A (2017) The benefit of evolving multidisciplinary care in ALS: a diagnostic cohort survival comparison. Amyotroph Lateral Scler Front Degener 18:569–575. https://doi.org/10.1080/21678421.2017.1349151
Zoccolella S, Beghi E, Palagano G, Fraddosio A, Guerra V, Lepore V, Simone IL, Lamberti P, Serlenga L, Logroscino G (2007) ALS multidisciplinary clinic and survival: Results from a population-based study in Southern Italy. J Neurol 254:1107–1112. https://doi.org/10.1007/s00415-006-0401-y
Ng L, Khan F, Mathers S (2009) Multidisciplinary care for adults with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst Rev (4):CD007425. https://doi.org/10.1002/14651858.CD007425.pub2
Ng L, Khan F, Young CA, Galea M (2017) Symptomatic treatments for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev (1):011776. https://doi.org/10.1002/14651858.CD011776.pub2
Loney PL, Chambers LW, Bennett KJ, Roberts JG, Stratford PW (1998) Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can 19:170–176
Hartling L, Hamm M, Milne A et al (2012) Validity and Inter-Rater Reliability Testing of Quality Assessment Instruments. Agency for Healthcare Research and Quality, Rockville (US)
Higgins JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:343. https://doi.org/10.1136/bmj.d5928
The Nordic Cochrane Centre (2014) Review manager (RevMan). Cochrane Collaboration, Copenhagen
García IJ, Moya NS, Munt MR et al (2015) La opinión del paciente cuenta: experiencia en la atención nutricional en un equipo multidisciplinar de ELA. Nutr Hosp 31:56–66. https://doi.org/10.3305/nh.2015.31.sup5.9132
Paipa AJ, Povedano M, Barcelo A et al (2019) Survival benefit of multidisciplinary care in amyotrophic lateral sclerosis in spain: association with noninvasive mechanical ventilation. J Multidiscip Healthc 12:465–470. https://doi.org/10.2147/JMDH.S205313
Traynor BJ, Alexander M, Corr B, Frost E, Hardiman O (2003) Effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: A population based study, 1996-2000. J Neurol Neurosurg Psychiatry 74:1258–1261. https://doi.org/10.1136/jnnp.74.9.1258
Stephens HE, Felgoise S, Young J, Simmons Z (2015) Multidisciplinary ALS clinics in the USA: a comparison of those who attend and those who do not. Amyotroph Lateral Scler Front Degener 16:196–201. https://doi.org/10.3109/21678421.2014.994530
Van Den Berg JP, Kalmijn S, Lindeman E et al (2005) Multidisciplinary ALS care improves quality of life in patients with ALS. Neurology 65:1264–1267. https://doi.org/10.1212/01.wnl.0000180717.29273.12
Rooney J, Byrne S, Heverin M, Tobin K, Dick A, Donaghy C, Hardiman O (2015) A multidisciplinary clinic approach improves survival in ALS: a comparative study of ALS in Ireland and Northern Ireland. J Neurol Neurosurg Psychiatry 86:496–501
Jenkins TM, Hollinger H, McDermott CJ (2014) The evidence for symptomatic treatments in amyotrophic lateral sclerosis. Curr Opin Neurol 27:524–531
Soriani MH, Desnuelle C (2017) Care management in amyotrophic lateral sclerosis. Rev Neurol (Paris) 173:288–299
Wei Q, Chen X, Zheng Z, Guo X, Huang R, Cao B, Zeng Y, Shang H (2015) The predictors of survival in Chinese amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler Front Degener 16:237–244. https://doi.org/10.3109/21678421.2014.993650
Burkhardt C, Neuwirth C, Sommacal A et al (2017) Is survival improved by the use of NIV and PEG in amyotrophic lateral sclerosis (ALS)? A post-mortem study of 80 ALS patients. PLoS One:12. https://doi.org/10.1371/journal.pone.0177555
Mandrioli J, Malerba SA, Beghi E et al (2018) Riluzole and other prognostic factors in ALS: a population-based registry study in Italy. J Neurol 265:817–827. https://doi.org/10.1007/s00415-018-8778-y
Paganoni S, Nicholson K, Leigh F, Swoboda K, Chad D, Drake K, Haley K, Cudkowicz M, Berry JD (2017) Developing multidisciplinary clinics for neuromuscular care and research. Muscle Nerve 56:848–858. https://doi.org/10.1002/mus.25725
Young CA, Ealing J, McDermott C, Williams T, al-Chalabi A, Majeed T, Burke G, Pinto A, Dick D, Talbot K, Harrower T, Walsh J, Chandran S, Hanemann CO, Mills R, Tennant A (2019) The relationships between symptoms, disability, perceived health and quality of life in amyotrophic lateral sclerosis/motor neuron disease. Amyotroph Lateral Scler Front Degener 20:317–327. https://doi.org/10.1080/21678421.2019.1615951
Hobson EV, McDermott CJ (2016) Supportive and symptomatic management of amyotrophic lateral sclerosis. Nat Rev Neurol 12:526–538
Oskarsson B, Gendron TF, Staff NP (2018) Amyotrophic lateral sclerosis: an update for 2018. Mayo Clin Proc 93:1617–1628
Rooney J, Byrne S, Heverin M, Corr B, Elamin M, Staines A, Goldacre B, Hardiman O (2013) Survival analysis of irish amyotrophic lateral sclerosis patients diagnosed from 1995–2010. PLoS One 8:e74733. https://doi.org/10.1371/journal.pone.0074733
Westeneng H-J, Debray TPA, Visser AE et al (2018) Prognosis for patients with amyotrophic lateral sclerosis: development and validation of a personalised prediction model. Lancet Neurol 17:423–433. https://doi.org/10.1016/S1474-4422(18)30089-9
Ong ML, Tan PF, Holbrook JD (2017) Predicting functional decline and survival in amyotrophic lateral sclerosis. PLoS One 12:e0174925. https://doi.org/10.1371/journal.pone.0174925
Ralli M, Lambiase A, Artico M, de Vincentiis M, Greco A (2019) Amyotrophic lateral sclerosis: autoimmune pathogenic mechanisms, clinical features, and therapeutic perspectives. Isr Med Assoc J 21:438–443
Andrews JA, Jackson CE, Heiman-Patterson TD et al (2020) Real-world evidence of riluzole effectiveness in treating amyotrophic lateral sclerosis. Amyotroph Lateral Scler Front Degener 21:509–518. https://doi.org/10.1080/21678421.2020.1771734
Hesters A, del Amador MM, Debs R et al (2020) Predictive factors for prognosis after gastrostomy placement in routine non-invasive ventilation users ALS patients. Sci Rep 10:1–6. https://doi.org/10.1038/s41598-020-70422-2
Burns TM, Graham CD, Rose MR, Simmons Z (2012) Quality of life and measures of quality of life in patients with neuromuscular disorders. Muscle Nerve 46:9–25
Ilse B, Prell T, Walther M, Hartung V, Penzlin S, Tietz F, Witte OW, Strauss B, Grosskreutz J (2014) Relationships between disease severity, social support and health-related quality of life in patients with amyotrophic lateral sclerosis. Soc Indic Res 120:871–882. https://doi.org/10.1007/s11205-014-0621-y
van Groenestijn AC, Kruitwagen-van Reenen ET, Visser-Meily JMA et al (2016) Associations between psychological factors and health-related quality of life and global quality of life in patients with ALS: a systematic review. Health Qual Life Outcomes 14:14. https://doi.org/10.1186/s12955-016-0507-6
Oh J, Kim JA (2017) Supportive care needs of patients with amyotrophic lateral sclerosis/motor neuron disease and their caregivers: a scoping review. J Clin Nurs 26:4129–4152
Antoniadi AM, Galvin M, Heverin M, Hardiman O, Mooney C (2020) Prediction of caregiver burden in amyotrophic lateral sclerosis: a machine learning approach using random forests applied to a cohort study. BMJ Open 10:10. https://doi.org/10.1136/bmjopen-2019-033109
Creemers H, De Morée S, Veldink JH et al (2016) Factors related to caregiver strain in ALS: a longitudinal study. J Neurol Neurosurg Psychiatry 87:775–781. https://doi.org/10.1136/jnnp-2015-311651
Seeber AA, Pols AJ, Hijdra A, Grupstra HF, Willems DL, de Visser M (2019) Advance care planning in progressive neurological diseases: lessons from ALS. BMC Palliat Care 18:50. https://doi.org/10.1186/s12904-019-0433-6
Hogden A, Greenfield D, Nugus P, Kiernan MC (2012) What influences patient decision-making in amyotrophic lateral sclerosis multidisciplinary care? A study of patient perspectives. Patient Prefer Adherence 6:829. https://doi.org/10.2147/PPA.S37851
Fullam T, Stephens HE, Felgoise SH, Blessinger JK, Walsh S, Simmons Z (2016) Compliance with recommendations made in a multidisciplinary ALS clinic. Amyotroph Lateral Scler Front Degener 17:30–37. https://doi.org/10.3109/21678421.2015.1074703
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Filipe Emanuel Oliveira de Almeida contributed to the study conception and design. Literature search and data analysis were performed by Filipe Emanuel Oliveira de Almeida, Anne Kelly do Carmo Santana, and Fernanda Oliveira de Carvalho. The first draft of the manuscript was written by Filipe Emanuel Oliveira de Almeida and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Almeida, F.E.O., do Carmo Santana, A.K. & de Carvalho, F.O. Multidisciplinary care in Amyotrophic Lateral Sclerosis: a systematic review and meta-analysis. Neurol Sci 42, 911–923 (2021). https://doi.org/10.1007/s10072-020-05011-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-05011-2