Abstract
In the past few decades, the so-feared botulinum toxin has conversely acquired the role of a ever more versatile therapeutic substance, used in an increasing number of pathological situations, including chronic headache and more precisely in the prophylaxis of chronic migraine. The medical use of botulinum toxin allowed to better understand its multiple mechanisms of action. Investigations about the pathophysiology of primary and secondary headaches has shown a series of common biological elements that frequently are also targets of the action of botulinum toxin. These increasing evidences allowed to identify some biochemical, neurophysiological and radiological markers that may be useful in the individuation of patients which probably will respond to the treatment with Onabotulinum toxin-A among chronic migraineurs. These predictors include CGRP plasmatic levels, specific laser-evoked potential responses, peculiar brain MRI and fMRI and characteristic clinical manifestations. Unfortunately, at now, these predictors are still not available for the clinical practice. Furthermore, the better knowledge about biology of headaches and regarding botulinum toxin activities may also help in directing investigations on the possible use of Onabotulinum toxin-A in other headaches different from migraine. This review tries to show in detail these biological mechanisms and their implication in selecting patients eligible for the treatment with Onabotulinum toxin-A.
Similar content being viewed by others
References
Welch MJ, Purkiss JR, Foster KA (2000) Sensitivity of embryonic rat dorsal root ganglia neurons to Clostridium botulinum neurotoxins. Toxicon 38(2):245–258 (PMID: 10665805)
Waseem Z, Boulias C, Gordon A, Ismail F, Sheean G, Furlan AD (2011) Botulinum toxin injections for low-back pain and sciatica. Cochrane Database Syst Rev CD1:008257. doi:10.1002/14651858.CD008257.pub2 (Review, PMID: 21249702)
Silberstein SD. (2016) The use of botulinum toxin in the management of headache disorders. Semin Neurol. Thieme Medical Publishers, 333 Seventh Avenue, New York, NY 10001, USA (PMID 26866501)
Aurora SK, Dodick DW et al (2010) PREEMPT 1 Chronic Migraine Study Group. Onabotulinum toxin A for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia 30(7):793–803. doi:10.1177/0333102410364676 (Epub 2010 Mar 17)
Diener HC, Dodick DW, Aurora SK, Turkel CC, DeGryse RE, Lipton RB, Silberstein SD, Brin MF (2010) PREEMPT 2 Chronic Migraine Study Group. Onabotulinum toxin A for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia 30(7):804–814. doi:10.1177/0333102410364677 (Epub 2010 Mar 17)
McCoy ES, Taylor-Blake B, Zylka MJ (2012) CGRPα-expressing sensory neurons respond to stimuli that evoke sensations of pain and itch. PLoS One 7(5):e36355. doi:10.1371/journal.pone.0036355 (PMID: 22563493)
Hou Q et al (2011) Keratinocyte expression of calcitonin gene-related peptide β: implications for neuropathic and inflammatory pain mechanisms. Pain 152(9):2036–2051. doi:10.1016/j.pain.2011.04.033 (PMID: 21641113)
Malon JT, Cao L (2016) Calcitonin gene-related peptide contributes to peripheral nerve injury-induced mechanical hypersensitivity through CCL5 and p38 pathways. J Neuroimmunol 15(297):68–75. doi:10.1016/j.jneuroim.2016.05.003 (PMID: 27397078)
Vega AV, et al. (2010) CGRP, a vasodilator neuropeptide that stimulates neuromuscular transmission and EC coupling. Curr Vasc Pharmacol 8(3):394–403
Goadsby PJ (2005) Calcitonin gene-related peptide antagonists as treatments of migraine and other primary headaches. Drugs 65(18):2557–2567
Tfelt-Hansen P et al (2009) Calcitonin gene-related peptide in blood: is it increased in the external jugular vein during migraine and cluster headache? A review. J Headache Pain 10(3):137–143. doi:10.1007/s10194-009-0112-8
Arulmani U et al (2004) Calcitonin gene-related peptide and its role in migraine pathophysiology. Eur J Pharmacol 500(1–3):315–330
Durham P (2006) Calcitonin gene-related peptide (CGRP) and migraine. Headache 48(Suppl 1):S3–S8. doi:10.1111/j.1526-4610.2006.00483.x (PMC 3134175, freely accessible, PMID 16927957)
Cernuda-Morollón E (2013) Interictal increase of CGRP levels in peripheral blood as a biomarker for chronic migraine. Neurology 81(14):1191–1196. doi:10.1212/WNL.0b013e3182a6cb72
Wang Y et al. (2016) Induction of calcitonin gene-related peptide expression in rats by cortical spreading depression. Cephalalgia. doi:10.1177/0333102416678388
Ashina H et al. (2016) CGRP in human models of primary headaches. Cephalalgia. doi:10.1177/0333102416684344
Edvinsson L et al. (2005) Neurobiology in primary headaches. Brain Res Brain Res Rev 48(3):438–456
Leone M et al. (2017) Advances in the understanding of cluster headache. Expert Rev Neurother 17(2):165–172. doi:10.1080/14737175.2016.1216796
Neeb L et al. (2016) Methylprednisolone blocks interleukin 1 beta induced calcitonin gene related peptide release in trigeminal ganglia cells. J Headache Pain 17:19. doi:10.1186/s10194-016-0609-x
Frese A et al. (2005) Calcitonin gene-related peptide in cervicogenic headache. Cephalalgia 25(9):700–703
Cernuda-Morollón E et al. (2015) Onabotulinum toxin A decreases interictal CGRP plasma levels in patients with chronic migraine. Pain 156(5):820–824. doi:10.1097/j.pain.0000000000000119
Lacković Z et al. (2016) Activity of botulinum toxin type A in cranial dura: implications for treatment of migraine and other headaches. Br J Pharmacol 173(2):279–291. doi:10.1111/bph.13366
Antonucci F et al (2016) SNAP-25, a known presynaptic protein with emerging postsynaptic functions. Front Synaptic Neurosci 24(8):7. doi:10.3389/fnsyn.2016.00007 (review, PMID: 27047369)
Garrity P (2010) Analysis of Drosophila TRPA1 reveals an ancient origin for human chemical nociception. Nature 464:25. doi:10.1038/nature08848597 (Macmillan Publishers Limited, all rights reserved © 2010)
Clapham DE (2003) TRP channels as cellular sensors. Nature 426(6966):517–524 (review, PMID: 14654832)
Starowicz K, Nigam S, Di Marzo V (2007) Biochemistry and pharmacology of endovanilloids. Pharmacol Ther 114(1):13–33
Blair NT et al (2015) Transient receptor potential channels. Last modified on 21 May 2015. IUPHAR/BPS guide to pharmacology
Story GM et al (2003) ANKTM1, a TRP-like channel expressed in nociceptive neurons, is activated by cold temperatures. Cell 112(6):819–829 (PMID: 12654248)
Geppetti P, Holzer P (1996) Neurogenic inflammation. CRC Press, Boca Raton
Caterina MJ, Schumacher MA et al (1997) The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389:816–824
Gibson HE, Edwards JG et al (2008) TRPV1 channels mediate long-term depression at synapses on hippocampal interneurons. Neuron 57(5):746–759. doi:10.1016/j.neuron.2007.12.027
Huang D, Li S, Dhaka A et al (2012) Expression of the transient receptor potential channels TRPV1, TRPA1 and TRPM8 in mouse trigeminal primary afferent neurons innervating the dura. Mol Pain 8:66. doi:10.1186/1744-8069-8-66
Diamond S, Freitag F, Phillips SB et al (2000) Intranasal civamide for the acute treatment of migraine headache. Cephalalgia 20(6):597–602
Fusco BM, Barzoi G, Agro F (2003) Repeated intranasal capsaicin applications to treat chronic migraine. Br J Anaesth 90(6):812
Nassini R, Materazzi S, Vriens J et al (2012) The ‘headache tree’ via umbellulone and TRPA1 activates the trigeminovascular system. Brain 135:376–390
Edelmayer RM, Le LN, Yan J et al (2012) Activation of TRPA1 on dural afferents: a potential mechanism of headache pain. Pain 153:1949–1958
Materazzi S, Benemei S, Fusi C et al (2013) Parthenolide inhibits nociception and neurogenic vasodilatation in the trigeminovascular system by targeting the TRPA1 channel. Pain 154:2750–2758
Zhong J, Minassi A, Prenen J et al (2011) Umbellulone modulates TRP channels. Pflugers Arch 2011(462):861–870
O’Neill J, Brock C, Olesen AE et al (2012) Unravelling the mystery of capsaicin: a tool to understand and treat pain. Pharmacol Rev 64:939–971
Burstein R, Zhang X et al (2014) Selective inhibition of meningeal nociceptors by botulinum neurotoxin type A: therapeutic implications for migraine and other pains. Cephalalgia 34(11):853–869. doi:10.1177/0333102414527648 (Epub 2014 Apr 2)
Amaya F, Oh-hashi K et al (2003) Local inflammation increases vanilloid receptor 1 expression within distinct subgroups of DRG neurons. Brain Res 963:190–196
Schueler M, Messlinger K et al (2013) Extracranial projections of meningeal afferents and their impact on meningeal nociception and headache. Pain 154:1622–1631
Zhang X, Strassman AM, Novack V (2016) Extracranial injections of botulinum neurotoxin type A inhibit intracranial meningeal nociceptors’ responses to stimulation of TRPV1 and TRPA1 channels: are we getting closer to solving this puzzle? Cephalalgia 36(9):875–886. doi:10.1177/0333102416636843 (Epub 2016 Mar 16 PMID: 26984967)
Denner AC et al. (2016) Role of transient receptor potential ankyrin 1 receptors in rodent models of meningeal nociception—experiments in vitro. Eur J Pain. doi:10.1002/ejp.986
Devesa I, Ferrándiz-Huertas C et al (2014) αCGRP is essential for algesic exocytotic mobilization of TRPV1 channels in peptidergic nociceptors. Proc Natl Acad Sci USA 111(51):18345–18350. doi:10.1073/pnas.1420252111 (Epub 2014 Dec 8)
Valeriani M et al. (2003) Reduced habituation to experimental pain in migraine patients: a CO(2) laser evoked potential study. Pain 105(1–2):57–64
de Tommaso M et al. (2016) Effects of OnabotulintoxinA on Habituation of Laser Evoked Responses in Chronic Migraine. Toxins (Basel) 8(6). doi:10.3390/toxins8060163
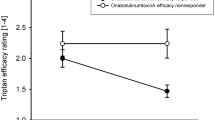
Hubbard CS, Becerra L, Smith JH et al (2016) Brain changes in responders vs. non-responders in chronic migraine: markers of disease reversal. Front Hum Neurosci 10:497 (eCollection 2016, PMID: 27766076)
Finkel AG (2015) Botulinum toxin and the treatment of headache: a clinical review. Toxicon 107(Pt A):114–119. doi:10.1016/j.toxicon.2015.09.008
Miller S, Correia F, Lagrata S, Matharu MS (2015) Onabotulinum toxin A for Hemicrania continua: open label experience in 9 patients. J Headache Pain 16:19. doi:10.1186/s10194-015-0502-z
Khalil M et al. (2013) Hemicrania continua responsive to botulinum toxin type a: a case report. Headache 53(5):831–833, doi:10.1111/head.12086
Rozen D et al. (2006) Treatment of tension-type headache with botox: a review of the literature. Mt Sinai J Med 73(1):493–498
Mathew NT et al. (2008) Predictors of response to botulinum toxin type A (BoNTA) in chronic daily headache. Headache 48(2):194–200
Bratbak DF et al (2016) Pilot study of sphenopalatine injection of onabotulinum toxin A for the treatment of intractable chronic cluster headache. Cephalalgia 36(6):503–509. doi:10.1177/0333102415597891 (PMID: 26232105)
Cernuda-Morollón E et al (2014) CGRP and VIP levels as predictors of efficacy of onabotulinum toxin type A in chronic migraine. Headache 54(6):987–995. doi:10.1111/head.12372 (Epub 2014 May 6)
Kim CC et al (2010) Predicting migraine responsiveness to botulinum toxin type A injections. Arch Dermatol 146(2):159–163. doi:10.1001/archdermatol.2009.356
Pagola I et al. (2014) Predictive factors of the response to treatment with onabotulinum toxin A in refractory migraine. Rev Neurol 58(6):241–246
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I certify that there is no actual or potential conflict of interest in relation to this article.
Rights and permissions
About this article
Cite this article
Lovati, C., Giani, L. Action mechanisms of Onabotulinum toxin-A: hints for selection of eligible patients. Neurol Sci 38 (Suppl 1), 131–140 (2017). https://doi.org/10.1007/s10072-017-2884-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-2884-y