Abstract
Background
Postoperative hyperperfusion may lead to severe neurological complications after superficial temporal artery to middle cerebral artery (STA-MCA) anastomosis. However, there are no reliable modalities to predict the occurrence of postoperative hyperperfusion during surgery. The purpose of this study is to evaluate whether a semiquantitative analysis of indocyanine green (ICG) videoangiography could be useful in predicting postoperative hyperperfusion after STA-MCA anastomosis.
Methods
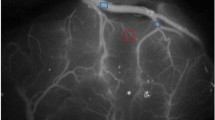
This study included seven patients who underwent STA-MCA anastomosis due to occlusive carotid artery diseases. During surgery, ICG videoangiography was performed before and after bypass procedures, and ICG intensity–time curves were semiquantitatively analyzed to evaluate hemodynamic changes by calculating maximum intensity, time to peak (TTP), and blood flow index (BFI).
Results
Maximum intensity significantly increased from 252.6 ± 132.5 to 351.7 ± 151.9 after bypass (p < 0.001). TTP was significantly shortened from 12.9 ± 4.4 s to 9.8 ± 3.7 s (p < 0.001). Furthermore, BFI significantly increased from 33.9 ± 28.1 to 74.6 ± 88.4 (p < 0.05). Postoperative hyperperfusion was observed in five of seven patients 1 day after surgery. The ratio of BFI before and after bypass procedures was significantly higher in patients with postoperative hyperperfusion than those without, 2.5 ± 1.1 and 1.5 ± 0.4, respectively (p = 0.013).
Conclusions
These findings suggest that semiquantitative analysis of ICG videoangiography is helpful in predicting occurrence of hyperperfusion after STA-MCA anastomosis in patients with occlusive carotid artery diseases.



Similar content being viewed by others
References
Hatazawa J, Fujita H, Kanno I, Satoh T, Iida H, Miura S, Murakami M, Okudera T, Inugami A, Ogawa (1995) Regional cerebral blood flow, blood volume, oxygen extraction fraction, and oxygen utilization rate in normal volunteers measured by the autoradiographic technique and the single breath inhalation method. Ann Nucl Med 9:15–21
Heros RC, Scott RM, Kistler JP, Ackerman RH, Conner ES (1984) Temporary neurological deterioration after extracranial-intracranial bypass. Neurosurgery 15:178–185
Kawamata T, Kawashima A, Yamaguchi K, Hori T, Okada Y (2011) Usefulness of intraoperative laser Doppler flowmetry and thermography to predict a risk of postoperative hyperperfusion after superficial temporal artery-middle cerebral artery bypass for moyamoya disease. Neurosurg Rev 34:355–362, discussion 362
Kawamata T, Okada Y, Kawashima A, Yoneyama T, Yamaguchi K, Ono Y, Hori T (2009) Postcarotid endarterectomy cerebral hyperperfusion can be prevented by minimizing intraoperative cerebral ischemia and strict postoperative blood pressure control under continuous sedation. Neurosurgery 64:447–453, discussion 453–444
Killory BD, Nakaji P, Gonzales LF, Ponce FA, Wait SD, Spetzler RF (2009) Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green angiography during cerebral arteriovenous malformation surgery. Neurosurgery 65:456–462, discussion 462
Kuebler WM, Sckell A, Habler O, Kleen M, Kuhnle GE, Welte M, Messmer K, Goetz AE (1998) Noninvasive measurement of regional cerebral blood flow by near-infrared spectroscopy and indocyanine green. J Cereb Blood Flow Metab 18:445–456
Kuroda S, Houkin K (2012) Bypass surgery for moyamoya disease: concept and essence of surgical techniques. Neurol Med Chir (Tokyo) 52:287–294
Kuroda S, Houkin K, Ishikawa T, Nakayama N, Ikeda J, Ishii N, Kamiyama H, Iwasaki Y (2004) Determinants of intellectual outcome after surgical revascularization in pediatric moyamoya disease: a multivariate analysis. Childs Nerv Syst 20:302–308
Kuroda S, Houkin K, Kamiyama H, Mitsumori K, Iwasaki Y, Abe H (2001) Long-term prognosis of medically treated patients with internal carotid or middle cerebral artery occlusion: can acetazolamide test predict it? Stroke 32:2110–2116
Kuroda S, Kamiyama H, Abe H, Asaoka K, Mitsumori K (1994) Temporary neurological deterioration caused by hyperperfusion after extracranial-intracranial bypass–case report and study of cerebral hemodynamics. Neurol Med Chir (Tokyo) 34:15–19
Kuroda S, Kamiyama H, Abe H, Houkin K, Isobe M, Mitsumori K (1993) Acetazolamide test in detecting reduced cerebral perfusion reserve and predicting long-term prognosis in patients with internal carotid artery occlusion. Neurosurgery 32:912–918, discussion 918–919
Kuroda S, Kamiyama H, Abe H, Yamauchi T, Kohama Y, Houkin K, Mitsumori K (1993) Cerebral blood flow in children with spontaneous occlusion of the circle of Willis (moyamoya disease): comparison with healthy children and evaluation of annual changes. Neurol Med Chir (Tokyo) 33:434–438
Kuroda S, Shiga T, Houkin K, Ishikawa T, Katoh C, Tamaki N, Iwasaki Y (2006) Cerebral oxygen metabolism and neuronal integrity in patients with impaired vasoreactivity attributable to occlusive carotid artery disease. Stroke 37:393–398
Kuroda S, Shiga T, Ishikawa T, Houkin K, Narita T, Katoh C, Tamaki N, Iwasaki Y (2004) Reduced blood flow and preserved vasoreactivity characterize oxygen hypometabolism due to incomplete infarction in occlusive carotid artery diseases. J Nucl Med 45:943–949
Kuroiwa T, Kajimoto Y, Ohta T (2001) Development and clinical application of near-infrared surgical microscope: preliminary report. Minim Invasive Neurosurg 44:240–242
Ogasawara K, Ogawa A (2006) JET study (Japanese EC-IC bypass trial). Nihon Rinsho 64(Suppl 7):524–527
Pena-Tapia PG, Kemmling A, Czabanka M, Vajkoczy P, Schmiedek P (2008) Identification of the optimal cortical target point for extracranial-intracranial bypass surgery in patients with hemodynamic cerebrovascular insufficiency. J Neurosurg 108:655–661
Perbeck L, Lewis DH, Thulin L, Tyden G (1985) Correlation between fluorescein flowmetry, 133Xenon clearance and electromagnetic flow measurement: a study in the intestine of the pig. Clin Physiol 5:293–299
Raabe A, Beck J, Gerlach R, Zimmermann M, Seifert V (2003) Near-infrared indocyanine green video angiography: a new method for intraoperative assessment of vascular flow. Neurosurgery 52:132–139, discussion 139
Raabe A, Nakaji P, Beck J, Kim LJ, Hsu FP, Kamerman JD, Seifert V, Spetzler RF (2005) Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green videoangiography during aneurysm surgery. J Neurosurg 103:982–989
Schuette AJ, Dannenbaum MJ, Cawley CM, Barrow DL (2011) Indocyanine green videoangiography for confirmation of bypass graft patency. J Korean Neurosurg Soc 50:23–29
Terborg C, Groschel K, Petrovitch A, Ringer T, Schnaudigel S, Witte OW, Kastrup A (2009) Noninvasive assessment of cerebral perfusion and oxygenation in acute ischemic stroke by near-infrared spectroscopy. Eur Neurol 62:338–343
van Mook WN, Rennenberg RJ, Schurink GW, van Oostenbrugge RJ, Mess WH, Hofman PA, de Leeuw PW (2005) Cerebral hyperperfusion syndrome. Lancet Neurol 4:877–888
Woitzik J, Horn P, Vajkoczy P, Schmiedek P (2005) Intraoperative control of extracranial-intracranial bypass patency by near-infrared indocyanine green videoangiography. J Neurosurg 102:692–698
Woitzik J, Pena-Tapia PG, Schneider UC, Vajkoczy P, Thome C (2006) Cortical perfusion measurement by indocyanine-green videoangiography in patients undergoing hemicraniectomy for malignant stroke. Stroke 37:1549–1551
Yamaguchi K, Kawamata T, Kawashima A, Hori T, Okada Y (2010) Incidence and predictive factors of cerebral hyperperfusion after extracranial-intracranial bypass for occlusive cerebrovascular diseases. Neurosurgery 67:1548–1554, discussion 1554
Yoshimoto T, Houkin K, Kuroda S, Abe H, Kashiwaba T (1997) Low cerebral blood flow and perfusion reserve induce hyperperfusion after surgical revascularization: case reports and analysis of cerebral hemodynamics. Surg Neurol 48:132–138, discussion 138–139
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
STA-MCA and other bypasses are still needed in selected patients with ischemic occlusive disease, and also often provide enough flow when MCA needs to be sacrificed due to unclippable or uncoilable giant or fusiform aneurysms instead of performing a more complex and riskier high-flow bypass. However, especially in chronically ischemic brain there is the danger of sudden hyperperfusion after such a lower flow bypass, which needs attention and actions when noticed. This nice paper not only shows excellent surgical techniques and results accordingly but also the further development of the almost revolutionary ICG angiography which really has improved patient safety over the last few years, and apparently continues to do so with more advancement. Whether using a double anastomosis instead of only one increases the incidence of hyperperfusion needs to be studied in larger series. However, in the present series, none of the five patients with hyperperfusion developed any neurological sequelae and with strict blood pressure limits it resolved within 1 week. We are waiting for further developments of the ICG angiography to show flow measurement in numbers in the oculars of the operating microscope as a tool for more accurate prediction of hyper- or hypoperfusion in the adjacent brain vasculature after performing a bypass.
Mika Niemelä
Helsinki, Finland
Rights and permissions
About this article
Cite this article
Uchino, H., Nakamura, T., Houkin, K. et al. Semiquantitative analysis of indocyanine green videoangiography for cortical perfusion assessment in superficial temporal artery to middle cerebral artery anastomosis. Acta Neurochir 155, 599–605 (2013). https://doi.org/10.1007/s00701-012-1575-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1575-y