Abstract
Purpose
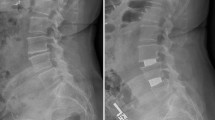
Iatrogenic injuries to paraspinal muscles during the posterior lumbar surgery (PLS) cause a reduction in their cross-sectional areas (CSAs) and contractile densities over time post-surgery. This study aims to quantify such alterations.
Method
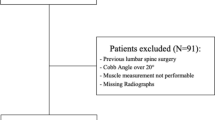
Pre- and postoperative CSAs (~6 months interval) of all paraspinal muscles were measured in six patients undergoing PLS using a 3-T magnetic resonance (MR) scanner to quantify the alterations in geometrical and tissue effective contractile (non-fatty) CSAs of these muscles at all lumbar levels. To examine the presence of any confounding effects on recorded changes within ~7-month period, measurements were also carried out on ten healthy volunteers.
Results
In the healthy population, an important (~22 %) portion of CSA of the erector spinae (ES) was noncontractile at the lower lumbar levels. Negligible variations over time in both the total geometrical (<1.7 % in average) and contractile (<1.2 %) CSAs of muscles were observed in the healthy group (i.e., no confounding effect). Following PLS, significant reductions were observed in the geometrical CSA of only multifidus (MF) muscle by ~14 and 11 % as well as in its contractile CSA by ~26 and 14 % at the L5–S1 and L4–L5 levels, respectively.
Conclusion
The total CSA of ES at lower lumbar levels shows substantial noncontractile contents in both healthy and patient populations. Biomechanical models of the spine should hence account for the noncontractile contents using only the effective contractile muscle CSAs. Postoperative variations in CSAs of paraspinal muscles may have profound effects on patterns of muscle activities, spinal loading, and stability.



Similar content being viewed by others
References
Kawaguchi Y, Matsui H, Tsuji H (1994) Back muscle injury after posterior lumbar spine surgery. Part 2: histologic and histochemical analyses in humans. Spine 19:2598–2602
Kawaguchi Y, Matsui H, Tsuji H (1996) Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine 21:941–944
Gille O, Jolivet E, Dousset V, Degrise C, Obeid I, Vital JM, Skalli W (2007) Erector spinae muscle changes on magnetic resonance imaging following lumbar surgery through a posterior approach. Spine 32:1236–1241
Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H (1999) Serial changes in trunk muscle performance after posterior lumbar surgery. Spine 24:1023–1028
Kim DY, Lee SH, Chung SK, Lee HY (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine 30:123–129
Mayer TG, Vanharanta H, Gatchel RJ, Mooney V, Barnes D, Judge L, Smith S, Terry A (1989) Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine 14:33–36
Airaksinen O, Herno A, Kaukanen E, Saari T, Sihvonen T, Suomalainen O (1996) Density of lumbar muscles 4 years after decompressive spinal surgery. Eur Spine J 5:193–197
Motosuneya T, Asazuma T, Tsuji T, Watanabe H, Nakayama Y, Nemoto K (2006) Postoperative change of the cross-sectional area of back musculature after 5 surgical procedures as assessed by magnetic resonance imaging. J Spinal Disord Tech 19:318–322
Min SH, Kim MH, Seo JB, Lee JY, Lee DH (2009) The quantitative analysis of back muscle degeneration after posterior lumbar fusion: comparison of minimally invasive and conventional open surgery. Asian Spine J. 3:89–95
Bresnahan L, Fessler RG, Natarajan RN (2010) Evaluation of change in muscle activity as a result of posterior lumbar spine surgery using a dynamic modeling system. Spine 35:E761–E767
Gatton ML, Pearcy MJ, Pettet GJ (2011) Computational model of the lumbar spine musculature: implications of spinal surgery. Clin Biomech 26:116–122
Marras WS, Jorgensen MJ, Granata KP, Wiand B (2001) Female and male trunk geometry: size and prediction of the spine loading trunk muscles derived from MRI. Clin Biomech 16:38–46
Anderson DE, D’Agostino JM, Bruno AG, Manoharan RK, Bouxsein ML (2012) Regressions for estimating muscle parameters in the thoracic and lumbar trunk for use in musculoskeletal modeling. J Biomech 45:66–75
Seo A, Lee JH, Kusaka Y (2003) Estimation of trunk muscle parameters for a biomechanical model by age, height and weight. J Occup Health 45:197–201
Hu ZJ, Fang XQ, Zhou ZJ, Wang JY, Zhao FD, Fan SW (2013) Effect and possible mechanism of muscle-splitting approach on multifidus muscle injury and atrophy after posterior lumbar spine surgery. J Bone Joint Surg Am 95(24):e192(1–9)
Holmbäck AM, Askaner K, Holtås S, Downham D, Lexell J (2002) Assessment of contractile and noncontractile components in human skeletal muscle by magnetic resonance imaging. Muscle Nerve 25:251–258
Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R (1998) Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol 85:115–122
Kent-Braun JA, Ng AV, Young K (2000) Skeletal muscle contractile and noncontractile components in young and older women and men. J Appl Physiol 88:662–668
Hu ZJ, He J, Zhao FD, Fang XQ, Zhou LN, Fan SW (2011) An assessment of the intra- and inter-reliability of the lumbar paraspinal muscle parameters using CT scan and magnetic resonance imaging. Spine 36:E868–E874
Arjmand N, Shirazi-Adl A (2006) Model and in vivo studies on human trunk load partitioning and stability in isometric forward flexions. J Biomech 39:510–521
Hajihosseinali M, Arjmand N, Shirazi-Adl A, Farahmand F, Ghiasi MS (2014) A novel stability and kinematics-driven trunk biomechanical model to estimate muscle and spinal forces. Med Eng Phys. doi:10.1016/j.medengphy.2014.07.009
Epstein NE (2011) Lumbar Spine Stenosis. In: Winn HR (ed) Youmans neurological surgery. Saunders, Philadelphia, pp 2932–2933
Käser L, Mannion AF, Rhyner A, Weber E, Dvorak J, Müntener M (2001) Active therapy for chronic low back pain: part 2. Effects on paraspinal muscle cross-sectional area, fiber type size, and distribution. Spine 26:909–919
Belavý DL, Bansmann PM, Böhme G, Frings-Meuthen P, Heer M, Rittweger J, Zange J, Felsenberg D (2011) Changes in intervertebral disc morphology persist 5 mo after 21-day bed rest. J Appl Physiol 111:1304–1314
Ranson CA, Burnett AF, Kerslake R, Batt ME, O’Sullivan PB (2006) An investigation into the use of MR imaging to determine the functional cross sectional area of lumbar paraspinal muscles. Eur Spine J 15:764–773
Keller A, Gunderson R, Reikerås O, Brox JI (2003) Reliability of computed tomography measurements of paraspinal muscle cross-sectional area and density in patients with chronic low back pain. Spine 28:1455–1460
Barker KL, Shamley DR, Jackson D (2004) Changes in the cross-sectional area of multifidus and psoas in patients with unilateral back pain: the relationship to pain and disability. Spine 29:E515–E519
Dangaria TR, Naesh O (1998) Changes in cross-sectional area of psoas major muscle in unilateral sciatica caused by disc herniation. Spine 23:928–931
Acknowledgments
This work was supported by grants from the Iran National Science Foundation (INSF), Sharif University of Technology (Tehran, Iran), Tehran University of Medical Sciences (Tehran, Iran), Institut de recherche Robert-Sauvé en santé et en sécurité du travail, IRSST, (Montréal, Canada), and Natural Sciences and Engineering Research Council of Canada (NSERC). Assistance of Mr. Saman Jamshidnejad is greatly appreciated.
Conflict of interest
The authors have no conflicts of interest concern.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ghiasi, M.S., Arjmand, N., Shirazi-Adl, A. et al. Cross-sectional area of human trunk paraspinal muscles before and after posterior lumbar surgery using magnetic resonance imaging. Eur Spine J 25, 774–782 (2016). https://doi.org/10.1007/s00586-015-4014-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4014-y