Abstract
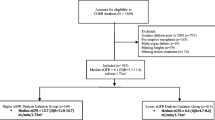
The purpose of this communication is to study the clinical patterns and level of residual renal function at the initiation of dialysis in children in the United States of America (US). Data were reviewed for 7,039 children under the age of 20 years and 647,600 adults extracted from the patient incidence report, obtained from the United States Renal Data Systems (USRDS), who were initiated on dialysis between January 1995 and September 2002. Based on pre-defined exclusion criteria, only 4,808 of the 7,093 (67.8%) pediatric entries were included in the analysis. About 6.9% of the entries were not used because of missing data only, 23.3% because of out of range data only, and 2.0% because of both missing and out of range data, a total of 32.2% exclusions. For adults, 570,808 (88.1%) had acceptable data. The percentage of the 4,808 children who were initiated on dialysis with an estimated GFR greater than 10 mL min−1 per 1.73 m2 (early start) was 49.6%. Using logistic regression, the factors affecting the probability of an early start were sex, race, type of insurance, region of the country, age at initiation of dialysis, and the year dialysis was initiated. The highest chance of starting dialysis early (0.77) was for a white male, aged 15–19 years, with insurance and residing in the Northwest part of the US The percentage of 4,808 children who initiated dialysis with an estimated GFR less than 5 mL min−1 per 1.73 m2 (late start) was 7.3%. The factors affecting the probability of a late start were sex, race, type of insurance, and the year dialysis was initiated. The greatest chance for a late start of dialysis was for black female patients without insurance (0.21). Mean estimated GFR at the start of dialysis was higher for children than for adults (10.7±4.6 vs 8.2±4.1 mL min−1 per 1.73 m2, respectively, P<0.0001). It was concluded that patterns of management of children with ESRD are not uniform among US children.



Similar content being viewed by others
Abbreviations
- US:
-
United States of America
- CKD:
-
Chronic kidney disease
- ESRD:
-
End stage renal disease
- HD:
-
Hemodialysis
- PD:
-
Peritoneal dialysis
- GFR:
-
Glomerular filtration rate
- USRDS:
-
United States Renal Data System
- BMI:
-
Body mass index
- HCFA:
-
Health Care Financing Agency
- RR:
-
Relative risk
References
National Institute of Diabetes and Digestive and Kidney Disease: Healthy People 2110: Chronic Renal Disease, Bethesda, MD, National Institute of Health, National Institute of diabetes and Digestive and Kidney Disease, 2000
Obrador GT, Pereira BJG (1998). Early referral to nephrologist and timely initiation of renal replacement therapy: a paradigm shift in the management of patients with chronic renal failure. Am J Kidney Dis 31:398–417
Scribner BH, Buri R, Caner JEZ, HegStrom R, Burnell JM (1960) The treatment of chronic uremia by means of intermittent dialysis: A preliminary report. Trans Am Soc Artif Organs 6:114–119
Popovich RP, Moncirif JW, Decherd JF, Bomar JB, Pyle WK (1976) The definition of a novel portable/wearable equilibrium dialysis technique (Abstract). Trans Am Soc Artif Intern Organs 5:64
Obrador GT, Arora P, Kausz AT, Ruthazer R, Pereira BJG, Levey A (1999) Level of renal function at the initiation of dialysis in the US end stage renal disease population. Kidney Int 56:2227–2235
United States growth charts. National center for health statistics, Center for disease control.http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/datafiles.htm
Seikaly MG, Loleh S, Rosenblum A, Browne R (2004) Validation of the Center for Medicare and Medicaid Services algorithm for eligibility for dialysis. Pediatr Nephrol 19:893–897
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A Simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Guruprasad M, Sarnak MJ, Levey AS (2001) Prediction equations to estimate glomerular filtration rate: update. Curr Opinion Nephrol Hyper 10:785–792
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 130:461–470
Seikaly MG, Browne R, Bajaj G, Arant BS (1996) Limitations to body length/plasma creatinine ratio as an estimate of glomerular filtration in children. Pediatr Nephrol 10:709–711
Eknoyan G, Levin NW (2002) K/DOQI Guidelines. Am J Kidney Dis. 39:S14–S214
Bach PB, Hoanginai H, Schrag D, Tate RC, Hargaves JL (2004) Primary care physicians who treat Black and White. N Engl J Med 351:575–584
Acknowledgments
We are indebted to Sharon Blend for secretarial support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government. The authors assume full responsibility for the accuracy and completeness of the ideas presented. This article is a direct result of the Health Care Quality Improvement Program initiated by the Centers for Medicare and Medicaid Services, which has encouraged identification of quality improvement projects derived from analysis of patterns of care, and therefore required no special funding on the part of this contractor. Ideas and contributions to the author concerning experience in engaging with issues presented are welcomed.
Rights and permissions
About this article
Cite this article
Seikaly, M.G., Salhab, N. & Browne, R. Patterns and time of initiation of dialysis in US children. Pediatr Nephrol 20, 982–988 (2005). https://doi.org/10.1007/s00467-004-1803-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-004-1803-7