Abstract
Background
The recurrence of stones after endoscopic minimally invasive cholecystolithotomy (EMIC) remains a hazardous problem in patients with cholelithasis. We sought to evaluate the risk factors for recurrence after cholecystolithotomy and to provide a theoretical basis for the indication for cholecystolithotomy.
Methods
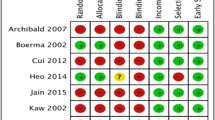
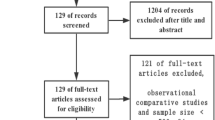
We searched the Cochrane Library, PubMed, EMBASE, WanFang Data, CNKI and VIP Data to identify controlled trials related to cholelithasis that were published between 2007 and 2016. The odds ratios (ORs) were calculated with 95% confidence intervals (CIs). Stata12.0 was used to test the heterogeneity and publication bias.
Results
Eight studies involving 1663 participants were selected. No significant differences were observed in hazardous factors including advanced age, gender and diabetes mellitus compared with the control groups. However, family history of cholelithasis, multiple calculi, gallbladder wall thickening (GBWT) over 3 mm, a preference for greasy food, dysfunction of the gallbladder and not taking oral ursodeoxycholic acid post-EMIC yielded pooled ORs (95% CI) of 3.28 (2.30, 4.66), 4.24 (2.76, 6.50), 18.4 (7.23, 46.83), 1.90 (1.20, 3.01), 26.16 (10.15, 62.34) and 2.90 (1.36, 6.15), respectively.
Conclusions
A family history of cholelithasis, multiple calculi, a GBWT ≥ 3 mm, a preference for greasy food, dysfunction of the gallbladder and not taking oral ursodeoxycholic acid post-EMIC are hazardous factors for stones and sludge after cholecystolithotomy.



Similar content being viewed by others
References
Marschall HU, Einarsson C (2007) Gallstone disease. J Intern Med 261(6):529–542
Traverso LW, Carl (1976) Langenbuch and the first cholecystectomy. Am J Surg 132(1):81–82
Watson RG, Love AH (1987) Intragastric bile acid concentrations are unrelated to symptoms of flatulent dyspepsia in patients with and without gallbladder disease and postcholecystectomy. Gut 28(2):131–136
Fein M et al (2002) Gastric bilirubin monitoring to assess duodenogastric reflux. Dig Dis Sci 47(12):2769–2774
Jaunoo SS, Mohandas S, Almond LM (2010) Postcholecystectomy syndrome (PCS). Int J Surg 8(1):15–17
Thurley PD, Dhingsa R (2008) Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol 191(3):794–801
Morvay K et al (1991) Effects of fecal bile acids on experimental colon carcinogenesis. Zentralbl Chir 116(23):1359–1367
Dowling RH (1988) Medical treatment of gallbladder stones: good news and bad news. In: Paumgartner G, Stiehl A, Gerok W (eds) Trends in bile acid research. Kluwer Academic, Dordrecht, pp 283–305
Kellett MJ, Wickham JE, Russell RC (1988) Percutaneous cholecystolithotomy. Br Med J (Clin Res Ed) 296(6620):453–455
BaoShan Z (2002) Endoscopic minimal invasive cholecystolithotomy in treatment of cholelithasis (Chinese Article). Chin J Endosc 07:7–10
Ye L, Liu J et al (2015) Endoscopic minimal invasive cholecystolithotomy versus laparoscopic cholecystectomy in treatment of cholecystolithiasis in China: a meta-analysis. Int J Surg 13:227–238
The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Jackson D, White IR, Riley RD (2012) Quantifying the impact of between-study heterogeneity in multivariate meta-analyses. Stat Med 31(29):3805–3820
Peters JL et al (2006) Comparison of two methods to detect publication bias in meta-analysis. JAMA 9(6):676–680 295)
Moher D et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012
Li QF, Xu X, Ge X (2015) Gallstone recurrence after minimally-invasive cholecystolithotomy with gallbladder reservation: a follow-up of 720 cases. Eur Rev Med Pharmacol Sci 19(8):1403–1406
Jianping Z (2012) Analysis of the risk factors for stones recurrence after Endoscopiccholecystolithotomy (Chinese Article). Chin Foreign Med Res 27:134
Chao C, Jiaming X, Yihui S, Chunwei G, Haorong W (2015) Analysis of the risk factors for recurrent gallbladder calculi in trauma surgery for calculi removal and gallbladder preservation (Chinese Article). Chin J Endosc Surg 06:426–429
Jianbin G, Guoxin Z, Zhenfu L, Tieying S, Jingcheng Z, Yubin Z, Yunfeng G (2014) recurrence analysis for recurrent gallbladder calculi in endoscopic minimally invasive cholecystolithotomy (Chinese Article). Hebei Med 18:2777–2779
Shuai L, Dong Z, Yuankai H, Weizhi W, Linghai C, Guanbo Z (2015) Analysis of gallstones recurrence factors after mini-invasive surgery of removing gallstones and preserving gallbladder through laparoscope combined with choledochoscope (Chinese Article). J Laparosc Surg 07:535–538
Jian K, Bo Z, Shilong W, Qingcheng M (2011) Analysis of gallstone recurrent rate and risk factors after cholecystolithotomy with gallbladder preserved. China Med 6(3):322–324
Liling S (2016) Analysis of gallstones recurrence factors after mini-invasive surgery of removing gallstones and preserving gallbladder through laparoscope (Chinese Article). Chin J Clin Ration Drug Use 26:110–111
Wei S (2013) Analysis of gallstones recurrence factors after mini-invasive surgery of removing gallstones and preserving gallbladder through laparoscope combined with choledochoscope (Chinese Article). Chin J Integr Tradit West Med Dig 08:429–431
Yufeng Z, Zhiqiang F, Hongyi Z et al (2016) meta-analysis of recurrence rate and its risk factory after cholecystolithotomy. Mil Med J Southeast China 18(3):230–232. https://doi.org/10.3969/j.jssn.1762-271X.2016.03.002
Donald JJ et al (1994) Percutaneous cholecystolithotomy: is gall stone recurrence inevitable? Gut 35(5):692–695
Liu J, Li J, Zhao Q (2009) The analyses of the results of 612 cases with gallbladder stones who underwent fibrocholedocoscope cholecystectomy for removal of caculas and preservation of gallbladder (Chinese Article). Mag Chin Surg 47:279–281
Kosters A, Jirsa M, Groen AK (2003) Genetic background of cholesterol gallstone disease. Biochim Biophys Acta 1637(1):1–19
Trifonova EV, Saifutdinov RG (2012) Factors affecting contractile function of the gallblader in patients with cholelithiasis. Eksp Klin Gastroenterol 4:16–20
Xiachu W, Xiaofu L, Liang L (2009) Research progress on the cause of cholelithiasis (Chinese article). J Reg Anat Oper Surg 01:56–57
Villanova N et al (1989) Gallstone recurrence after successful oral bile acid treatment. A 12-year follow-up study and evaluation of long-term postdissolution treatment. Gastroenterology 97(3):726–731
Dhiman RK, Chawla YK (2006) Is there a link between oestrogen therapy and gallbladder disease? Expert Opin Drug Saf 5(1):117–129
Funding
National Natural Science Foundation of China, No. 81702375. Natural Science Foundation of Guangdong Province, No. 2016A030313200. Science and Technology Project of Guangzhou City, No. 201607010022. Natural Science Foundation of Guangdong Province, No. 2017A030313580. Fundamental Research Funds for the Central Universities (Sun Yat-sen University), No. 17ykp.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Wenchao Li, Pinzhu Huang, Zhicheng Yao, Purun Lei, Hui Luo, Zhiyong Xiong, Bo Liu and Kunpeng Hu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, W., Huang, P., Lei, P. et al. Risk factors for the recurrence of stones after endoscopic minimally invasive cholecystolithotomy in China: a meta-analysis. Surg Endosc 33, 1802–1810 (2019). https://doi.org/10.1007/s00464-018-6455-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6455-y