Abstract
Background
Multiport laparoscopic cholecystectomy (MLC) is the gold standard technique for cholecystectomy. In order to reduce postoperative pain and improve cosmetic results, the application of the single-incision laparoscopic cholecystectomy (SILC) technique was introduced, leading surgeons to face important challenges. Robotic technology has been proposed to overcome some of these limitations. The purpose of this review is to assess the safety of single-incision robotic cholecystectomy (SIRC) for benign disease.
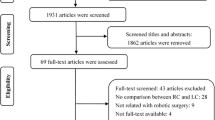
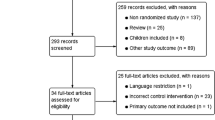
Methods
An Embase and Pubmed literature search was performed in February 2017. Randomized controlled trial and prospective observational studies were selected and assessed using PRISMA recommendations. Primary outcome was overall postoperative complication rate. Secondary outcomes were postoperative bile leak rate, total conversion rate, operative time, wound complication rate, postoperative hospital stay, and port site hernia rate. The outcomes were analyzed in Forest plots based on fixed and random effects model. Heterogeneity was assessed using the I2 statistic.
Results
A total of 13 studies provided data about 1010 patients who underwent to SIRC for benign disease of gallbladder. Overall postoperative complications rate was 11.6% but only 4/1010 (0.4%) patients required further surgery. A postoperative bile leak was reported in 3/950 patients (0.3%). Conversion occurred in 4.2% of patients. Mean operative time was 86.7 min including an average of 42 min should be added as for robotic console time. Wound complications occurred in 3.7% of patients. Median postoperative hospital stay was 1 day. Port site hernia at the latest follow-up available was reported in 5.2% of patients.
Conclusions
The use of the Da Vinci robot in single-port cholecystectomy seems to have similar results in terms of incidence and grade of complications compared to standard laparoscopy. In addition, it seems affected by the same limitations of single-port surgery, consisting of an increased operative time and incidence of port site hernia.

Reproduced with the permission from Moher et al. [61]








Similar content being viewed by others
References
Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I (1997) One-wound laparoscopic cholecystectomy. Br J Surg 84:695
Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK (2011) Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg 202:254–258
Karim MA, Ahmed J, Mansour M, Ali A (2012) Single incision vs. conventional multiport laparoscopic cholecystectomy: a comparison of two approaches. Int J Surg 10:368–372
Pisanu A, Reccia I, Porceddu G, Uccheddu A (2012) Metaanalysis of prospective randomized studies comparing single-incision laparoscopic cholecystectomy (SILC) and conventional multiport laparoscopic cholecystectomy (CMLC). J Gastrointest Surg 16:1790–1801
Arezzo A, Passera R, Bullano A, Mintz Y, Kedar A, Boni L, Cassinotti E, Rosati R, Fumagalli Romario U, Sorrentino M, Brizzolari M, Di Lorenzo N, Gaspari AL, Andreone D, De Stefani E, Navarra G, Lazzara S, Degiuli M, Shishin K, Khatkov I, Kazakov I, Schrittwieser R, Carus T, Corradi A, Sitzman G, Lacy A, Uranues S, Szold A, Morino M (2017) Multi-port versus single-port cholecystectomy: results of a multi-centre, randomised controlled trial (MUSIC trial). Surg Endosc 31:2872–2880
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 254:22–27
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047
Kroh M, El-Hayek K, Rosenblatt S, Chand B, Escobar P, Kaouk J, Chalikonda S (2011) First human surgery with a novel single port robotic system: cholecystectomy using the da Vinci single-site platform. Surg Endosc 25:3566–3573
Wren SM, Curet MJ (2011) Single-port robotic cholecystectomy: results from a first human use clinical study of the new da Vinci single-site surgical platform. Arch Surg 146:1122–1127
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151:65–94
Whiting P, Rutjes AW, Dinnes J, Reitsma J, Bossuyt PM, Kleijnen J (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Methodol 10:3–25
Schwarzer G (2007) Meta: an R package for meta-analysis. R News 7:40–45
Konstantinidis KM, Hirides P, Hirides S, Chrysocheris P, Georgiou M (2012) Cholecystectomy using a novel Single-Site® robotic platform: early experience from 45 consecutive cases. Surg Endosc 26:2687–2694
Buzad FA, Corne LM, Brown TC, Fagin RS, Hebert AE, Kaczmarek CA, Pack AN, Payne TN (2013) Single-site robotic cholecystectomy: efficiency and cost analysis. Int J Med Robot 9:365–370
Ayloo S, Choudhury N (2014) Single-site robotic cholecystectomy. JSLS 18:1–5
Morel P, Buchs NC, Iranmanesh P, Pugin F, Buehler L, Azagury DE, Jung M, Volonte F, Hagen ME (2014) Robotic single-site cholecystectomy. J Hepatobiliary Pancreat Sci 21:18–25
Vidovszky TJ, Carr AD, Farinholt GN, Ho HS, Smith WH, Ali MR (2014) Single-site robotic cholecystectomy in a broadly inclusive patient population: a prospective study. Ann Surg 260:134–141
Bibi S, Rahnemai-Azar AA, Coralic J, Bayoumi M, Khorsand J, Farkas DT, Prasad LM (2015) Single-site robotic cholecystectomy: the timeline progress. World J Surg 39:2386–2391
Gustafson M, Lescouflair T, Kimball R, Daoud I (2016) A comparison of robotic single-incision and traditional laparoscopic cholecystectomy. Surg Endosc 30:2276–2280
Kudsi OY, Castellanos A, Kaza S, McCarty J, Dickens E, Martin D, Tiesenga FM, Konstantinidis K, Hirides P, Mehendale S, Gonzalez A (2017) Cosmesis, patient satisfaction, and quality of life after da Vinci Single-Site cholecystectomy and multiport laparoscopic cholecystectomy: short-term results from a prospective, multicenter, randomized, controlled trial. Surg Endosc 3:3242–3250
Lee H, Lee DH, Kim H, Han Y, Kim SW, Jang JY (2017) Single-incision robotic cholecystectomy: a special emphasis on utilization of transparent gloveports to overcome limitations of single-site port. Int J Med Robot 13:1–6
Pietrabissa A, Pugliese L, Vinci A, Peri A, Tinozzi FP, Cavazzi E, Pellegrino E, Klersy C (2016) Short-term outcomes of single-site robotic cholecystectomy versus four-port laparoscopic cholecystectomy: a prospective, randomized, double-blind trial. Surg Endosc 30:3089–3097
Van der Linden YT, Brenkman HJ, Van der Horst S, Van Grevenstein WM, Van Hillegersberg R, Ruurda JP (2016) Robotic single-port laparoscopic cholecystectomy is safe but faces technical challenges. J Laparoendosc Adv Surg Tech A 26:857–861
Balachandran B, Hufford TA, Mustafa T, Kochar K, Sulo S, Khorsand J (2017) A comparative study of outcomes between single-site robotic and multiport laparoscopic cholecystectomy: an experience from a tertiary center. World J Surg 41:1246–1253
Clavien PA, Sanabria JR, Strasberg SM (1992) Proposed classification of complications with examples in cholecystectomy. Surgery 111:518–526
Dixon E, Vollmer Jr, Charles M, Gary R (2015) Management of benign biliary stenosis and injury: a comprehensive guide. Springer, Cham
Vollmer CM Jr, Callery MP (2007) Biliary injury following laparoscopic cholecystectomy: why still a problem? Gastroenterology 133:1039–1041
Khan MH, Howard TJ, Fogel EL, Sherman S, McHenry L, Watkins JL, Canal DF, Lehman GA (2007) Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP: experience at a large tertiary referral center. Gastrointest Endosc 65:247–252
Visser BC, Parks RW, Garden OJ (2008) Open cholecystectomy in the laparoendoscopic era. Am J Surg 195:108–114
Catarci M, Zaraca F, Scaccia M, Carboni M (1993) Lost intraperitoneal stones after laparoscopic cholecystectomy: harmless sequela or reason for reoperation? Surg Laparosc Endosc 3:318–322
Cervantes J, Rojas GA, Ponte R (1994) Intrahepatic subcapsular biloma. A rare complication of laparoscopic cholecystectomy. Surg Endosc 8:208–210
Stupak D, Cohen S, Kasmin F, Lee Y, Siegel JH (2007) Intra-abdominal actinomycosis 11 years after spilled gallstones at the time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 17:542–544
Roberts DJ, Chun HM (2005) Dropped gallstone as a nidus of intra-abdominal abscess complicated by empyema. Clin Infect Dis 41:e64–e66
Binenbaum SJ, Goldfarb MA (2006) Inadvertent enterotomy in minimally invasive abdominal surgery. JSLS 10:336–340
Strasberg SM (2005) Biliary injury in laparoscopic surgery: Part 1. Processes used in determination of standard of care in misidentification injuries. J Am Coll Surg 201:598–603
Strasberg SM (2005) Biliary injury in laparoscopic surgery: Part 2. Changing the culture of cholecystectomy. J Am Coll Surg 201:604–611
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180:101–125
Thurley PD, Dhingsa R (2008) Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol 191:794–801
Biscione FM, Couto RC, Pedrosa TM, Neto MC (2007) Comparison of the risk of surgical site infection after laparoscopic cholecystectomy and open cholecystectomy. Infect Control Hosp Epidemiol 28:1103–1106
Moore MJ, Bennett CL (1995) The learning curve for laparoscopic cholecystectomy. The Southern Surgeons Club. Am J Surg 170:55–59
Morgenstern L, McGrath MF, Carroll BJ, Paz-Partlow M, Berci G (1995) Continuing hazards of the learning curve in laparoscopic cholecystectomy. Am Surg 61:914–918
Richardson MC, Bell G, Fullarton GM (1996) Incidence and nature of bile duct injuries following laparoscopic cholecystectomy: an audit of 5913 cases. West of Scotland Laparoscopic Cholecystectomy Audit Group. Br J Surg 83:1356–1360
Z’graggen K, Wehrli H, Metzger A, Buehler M, Frei E, Klaiber C (1998) Complications of laparoscopic cholecystectomy in Switzerland. A prospective 3-year study of 10,174 patients. Swiss Association of Laparoscopic and Thoracoscopic Surgery. Surg Endosc 12:1303–1310
Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC (2006) Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg 93:844–853
Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC (1993) Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg 165:9–14
Nuzzo G, Giuliante F, Giovannini I, Ardito F, D’Acapito F, Vellone M, Murazio M, Capelli G (2005) Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg 140:986–992
Arezzo A, Passera R, Forcignanò E, Rapetti L, Cirocchi R, Morino M (2018) Single-Incision laparoscopic cholecystectomy is responsible for increased adverse events: results of a meta-analysis of randomized controlled trials. Surg Endosc. https://doi.org/10.1007/s00464-018-6143-y
Trastulli S, Cirocchi R, Desiderio J, Guarino S, Santoro A, Parisi A, Noia G, Boselli C (2013) Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg 100:191–208
Zacks SL, Sandler RS, Rutledge R, Brown RS Jr (2002) A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol 97:334–340
Zdichavsky M, Bashin YA, Blumenstock G, Zieker D, Meile T, Königsrainer A (2012) Impact of risk factors for prolonged operative time in laparoscopic cholecystectomy. J Gastroenterol Hepatol 24:1033–1038
Spinoglio G, Lenti LM, Maglione V, Lucido FS, Priora F, Bianchi PP, Grosso F, Quarati R (2012) Single-site robotic cholecystectomy (SSRC) versus single-incision laparoscopic cholecystectomy (SILC): comparison of learning curves. First European experience. Surg Endosc 26:1648–1655
Iranmanesh P, Morel P, Buchs NC, Pugin F, Volonte F, Kreaden US, Hagen ME (2013) Docking of the da Vinci Si surgical system with single site technology. Int J Med Robotics Comput Assit Surg 9:12–16
Shamiyeh A, Danis J, Wayand W, Zehetner J (2007) A 14-year analysis of laparoscopic cholecystectomy: conversion—when and why? Surg Laparosc Endosc Percutan Tech 17:271–276
Shaher Z (2007) Port closure techniques. Surg Endosc 21:1264–1274
Duca S, Bãlã O, Al-Hajjar N, Lancu C, Puia IC, Munteanu D, Graur F (2003) Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB (Oxford) 5:152–158
Bedeir K, Mann A, Youssef Y (2016) Robotic single-site versus laparoscopic cholecystectomy: which is cheaper? A cost report and analysis. Surg Endosc 30:267–272
Koshenkov VP, Koru-Sengul T, Franceschi D, Dipasco PJ, Rodgers SE (2013) Predictors of incidental gallbladder cancer in patients undergoing cholecystectomy for benign gallbladder disease. J Surg Oncol 107:118–123
Cavallaro A, Piccolo G, Panebianco V, Lo Menzo E, Berretta M, Zanghì A, Di Vita M, Cappellani A (2012) Incidental gallbladder cancer during laparoscopic cholecystectomy: managing an unexpected finding. World J Gastroenterol 18:4019–4027
Shen BY, Zhan Q, Deng XX, Bo H, Liu Q, Peng CH, Li HW (2012) Radical resection of gallbladder cancer: could it be robotic? Surg Endosc 26:3245–3250
Zeng G, Teo NZ, Goh BKP (2018) Short-term outcomes of minimally invasive surgery for patients presenting with suspected gallbladder cancer: report of 8 cases. J Minim Access Surg 20:1–6
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA GROUP (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097
Funding
The authors declare that no funding support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Marco Migliore, Alberto Arezzo, Simone Arolfo, Roberto Passera, and Mario Morino have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Migliore, M., Arezzo, A., Arolfo, S. et al. Safety of single-incision robotic cholecystectomy for benign gallbladder disease: a systematic review. Surg Endosc 32, 4716–4727 (2018). https://doi.org/10.1007/s00464-018-6300-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6300-3