Abstract
Background
The purpose of this study was to compare length of stay, as one of the efficacy indicators, and effectiveness, in terms of operative complications and mortality, between laparoscopic (LC) and open cholecystectomy, and to verify the 10-year temporal trends in the application of the LC technique in a large regional population.
Methods
This was a retrospective cohort study based on 73,853 hospital discharge records of cholecystectomies for gallstone disease (GD) in residents of the Veneto from 2001 to 2010, at both public and accredited private hospitals. The data are from a regional administrative database. The main epidemiological rates calculated, and expressed per 100,000 residents, were the cholecystectomy rate (CR) for gallstones by surgical technique (laparoscopic or open surgery), and the in-hospital mortality rate (MR), considered as the in-hospital MR regardless of the specific cause of death.
Results
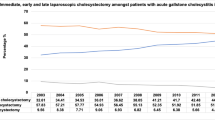
The CR was 139.7 higher in females, with a male-to-female ratio of 1:1.5. LC was performed more frequently in females than in males and in younger than in older patients. From 2001 to 2010, there was a significant linear rising trend in the use of LC, in fact during the period considered, the use of laparoscopic surgery increased significant (χ 2 trend: 316,917; p < 0.05), reaching 93.6 % of surgical procedures for gallstones during the year 2010.
Conclusions
There are still some age- and gender-related disparities in its usage, although LC is an increasingly widely applied, as effective procedure.

Similar content being viewed by others
References
Festi D, Dormi A, Capodicasa S, Staniscia T, Attili AF, Loria P, Pazzi P, Mazzella G, Sama C, Roda E, Colecchia A (2008) Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project). World J Gastroenterol 14(34):5282–5289
Berthou JCh, Dron B, Charbonneau P, Moussalier K, Pellissier L (2007) Evaluation of laparoscopic treatment of common bile duct stones in a prospective series of 505 patients: indications and results. Surg Endosc 21(11):1970–1974
Suuronen S, Koski A, Nordstrom P, Miettinen P, Paajanen H (2010) Laparoscopic and open cholecystectomy in surgical training. Dig Surg 27(5):384–390
Kuwabara K, Matsuda S, Ishikawa KB, Horiguchi H, Fujimori K (2010) Comparative quality of laparoscopic and open cholecystectomy in the elderly using propensity score matching analysis. Gastroenterol Res Pract 2010:490147
Ammori BJ, Vezakis A, Davides D, Martin IG, Larvin M, McMahon MJ (2001) Laparoscopic cholecystectomy in morbidly obese patients. Surg Endosc 15(11):1336–1339
Simopoulos C, Polychronidis A, Botaitis S, Perente S, Pitiakoudis M (2005) Laparoscopic cholecystectomy in obese patients. Obes Surg 15(2):243–246
Farkas DT, Moradi D, Moaddel D, Nagpal K, Cosgrove JM (2012) The impact of body mass index on outcomes after laparoscopic cholecystectomy. Surg Endosc 26(4):964–969
Keus F, Gooszen HG, van Laarhoven CJHM (2010) Open, small-incision, or laparoscopic cholecystectomy for patients with symptomatic cholecystolithiasis. An overview of Cochrane Hepato-Biliary Group reviews. Cochrane Database Syst Rev 20(1):CD008318. doi:10.1002/14651858.CD008318
Matovic E, Hasukic S, Ljuca F, Halilovic H (2012) Quality of life in patients after laparoscopic and open cholecystectomy. Med Arh 66(2):97–100
Epidemiologia e Ricerca Applicata, Atlante ERA (2009). Le procedure a rischio di inappropriatezza. http://www.atlantesanitario.it/index.php?option=com_content&view=article&id=82&Itemid=93. Accessed 1 Sep 2012
Legorreta AP, Silber JH, Costantino GN, Kobylinski RW, Zatz SL (1993) Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy. JAMA 270(12):1429–1432
Pagliarulo M, Fornari F, Fraquelli M, Zoli M, Giangregorio F, Grigolon A, Peracchi M, Conte D (2004) Gallstone disease and related risk factors in a large cohort of diabetic patients. Dig Liver Dis 36(2):130–134
European charter on counteracting obesity, EUR/06/5062700/8 16 November 2006 61995 (Original: English)
ISTAT (2011) Italia in Cifre. www.istat.it/it/files/2011/06/italiaincifre2011.pdf. Accessed 1 Sep 2012
International Diabetes Federation (2012) Diabetes Atlas 2012 update. International Diabetes Federation, Brussels
Csikesz NG, Tseng JF, Shah SA (2008) Trends in surgical management for acute cholecystitis. Surgery 144(2):283–289
Sakpal SV, Bindra SS, Chamberlain RS (2010) Laparoscopic cholecystectomy conversion rates two decades later. JSLS 14(4):476–483
Dubecz A, Langer M, Stadlhuber RJ, Schweigert M, Solymosi N, Feith M, Stein HJ (2012) Cholecystectomy in the very elderly: is 90 the new 70? J Gastrointest Surg 16(2):282–285
Tucker JJ, Yanagawa F, Grim R, Bell T, Ahuja V (2011) Laparoscopic cholecystectomy is safe but underused in the elderly. Am Surg 77(8):1014–1020
Kuwabara K, Matsuda S, Fushimi K, Ishikawa KB, Horiguchi H, Fujimori K (2011) Relationships of age, cholecystectomy approach and timing with the surgical and functional outcomes of elderly patients with cholecystitis. Int J Surg 9(5):392–399
Kuwabara K, Matsuda S, Ishikawa KB, Horiguchi H, Fujimori K (2010) Comparative quality of laparoscopic and open cholecystectomy in the elderly using propensity score matching analysis. Gastroenterol Res Pract 2010:490147
Tagle FM, Lavergne J, Barkin JS, Unger SW (1997) Laparoscopic cholecystectomy in the elderly. Surg Endosc 11(6):636–638
Zacks SL, Sandler RS, Rutledge R, Brown RS Jr (2002) A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol 97(2):334–340
Purkayastha S, Tilney HS, Georgiou P, Athanasiou T, Tekkis PP, Darzi AW (2007) Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: a meta-analysis of randomised control trials. Surg Endosc 21(8):1294–1300
Dipartimento della Programmazione e dell’Ordinamento del Servizio Sanitario Nazionale Dir. Gen. della Programmazione sanitaria Ufficio VI. Rapporto annuale sull’’attività di ricovero ospedaliero. Dati SDO 2010
D Keus F, de Jonge T, Gooszen HG, Buskens E, van Laarhoven CJ (2009) Cost-minimization analysis in a blind randomized trial on small-incision versus laparoscopic cholecystectomy from a societal perspective: sick leave outweighs efforts in hospital savings. Trials 10:80. doi:10.1186/1745-6215-10-80
Secco GB, Cataletti M, Bonfante P, Baldi E, Davini MD, Biasotti B, Ravera G, Ferraris R (2002) Laparoscopic versus mini-cholecystectomy: analysis of hospital costs and social costs in a prospective randomized study. Chir Ital 54(5):685–692
Shea JA, Healey MJ, Berlin JA, Clarke JR, Malet PF, Staroscik RN, Schwartz JS, Williams SV (1996) Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg 224(5):609–620
Richards C, Edwards J, Culver D, Emori TG, Tolson J, Gaynes R, National Nosocomial Infections Surveillance (NNIS) System, Centers for Disease Control and Prevention (2003) Does using a laparoscopic approach to cholecystectomy decrease the risk of surgical site infection? Ann Surg 237(3):3
Hannan EL, Imperato PJ, Nenner RP, Starr H (1999) Laparoscopic and open cholecystectomy in New York State: mortality, complications, and choice of procedure. Surgery 125(2):223–231
Wiseman JT, Sharuk MN, Singla A, Cahan M, Litwin DE, Tseng JF, Shah SA (2010) Surgical management of acute cholecystitis at a tertiary care center in the modern era. Arch Surg 145(5):439–444. doi:10.1001/archsurg.2010.54.58-62
Donabedian A (1998) The quality of care. How can it be assessed? JAMA 260(12):1743–1748
Thomas EJ, Petersen L (2003) Measuring errors and adverse events in health care. J Gen Intern Med 18(1):61–67
Ospedalizzazione e Mobilità in Veneto: le Dimissioni Ospedaliere negli Anni 2000–2010 a cura di: Servizio Epidemiologico Regionale; Servizio Controllo Investimenti Prezzi Acquisti SSR. www.ser-veneto.it
Jurek AM, Greenland S, Maldonado G, Church TR (2005) Proper interpretation of non-differential misclassification effects: expectations vs observations. Int J Epidemiol 34(3):680–687
Disclosures
Mario Saia, Domenico Mantoan, Alessandra Buja, Chiara Bertonecello, Tatjana Baldovin, Giampietro Callegaro, and Vincenzo Baldo have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saia, M., Mantoan, D., Buja, A. et al. Time trend and variability of open versus laparoscopic cholecystectomy in patients with symptomatic gallstone disease. Surg Endosc 27, 3254–3261 (2013). https://doi.org/10.1007/s00464-013-2902-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2902-y