Abstract
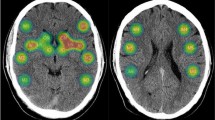
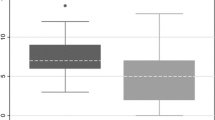
This study investigated the impact of leukoaraiosis (LA) involving the contralateral corticobulbar tract (CBT) on dysphagia in patients with unilateral corona radiata (CR) infarction with CBT involvement. Patients admitted to the Department of Neurology (September 2011–August 2014) were evaluated; those with a first episode of acute unilateral CR infarction involving the CBT and with LA were included. The ‘Case’ group comprised patients with LA involving the contralateral CBT; the ‘Control’ group comprised patients with LA not involving the contralateral CBT. The primary outcome was the feeding method at discharge; secondary outcomes were the feeding method at admission and results of the bedside swallowing test, videofluoroscopic swallowing study (VFSS), videofluoroscopic dysphagia scale, penetration–aspiration scale, American Speech–Language–Hearing Association National Outcome Measurement System Swallowing Scale (ASHA NOMS), oral transit time, and pharyngeal transit time. Infarct size was measured using brain magnetic resonance imaging; LA severity was rated using the Fazekas scale. Eighty-one patients were included (mean age 64.6 ± 11.5 years; 64% male; Case group: 20, 5 underwent VFSS; Control group: 67, 11 underwent VFSS). The Case group was older and had higher total Fazekas scale score than the Control group. The feeding method at discharge and ASHA NOMS score were significantly worse in the Case group than in the Control group. Multivariate analysis revealed that LA involving the contralateral CBT independently predicted the feeding method at discharge and ASHA NOMS score. In conclusion, LA involving the contralateral CBT is associated with dysphagia in patients with unilateral CR infarction involving the CBT.


Similar content being viewed by others
References
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63. https://doi.org/10.1161/01.STR.0000190056.76543.eb.
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;30:744–8. https://doi.org/10.1161/01.STR.30.4.744.
Broadley S, Cheek A, Salonikis S, Whitham E, Chong V, Cardone D, Alexander B, Taylor J, Thompson P. Predicting prolonged dysphagia in acute stroke: the Royal Adelaide Prognostic Index for Dysphagic Stroke (RAPIDS). Dysphagia. 2005;20:303–10. https://doi.org/10.1007/s00455-005-0032-y.
Ovbiagele B, Saver JL. Cerebral white matter hyperintensities on MRI: current concepts and therapeutic implications. Cerebrovasc Dis. 2006;22:83–90. https://doi.org/10.1159/000093235.
Pantoni L, Basile AM, Pracucci G, Asplund K, Bogousslavsky J, Chabriat H, et al. Impact of age-related cerebral white matter changes on the transition to disability—the LADIS study: rationale, design and methodology. Neuroepidemiology. 2005;24:51–62. https://doi.org/10.1159/000081050.
Toscano M, Cecconi E, Capiluppi E, Viganò A, Bertora P, Campiglio L, et al. Neuroanatomical, clinical and cognitive correlates of post-stroke dysphagia. Eur Neurol. 2015;74:171–7. https://doi.org/10.1159/000441056.
Nam KW, Kwon HM, Lim JS, Lee YS. Leukoaraiosis is associated with pneumonia after acute ischemic stroke. BMC Neurol. 2017;17:51. https://doi.org/10.1186/s12883-017-0830-5.
Jang SH, Seo JP. The anatomical location of the corticobulbar tract at the corona radiata in the human brain: diffusion tensor tractography study. Neurosci Lett. 2015;590:80–3. https://doi.org/10.1016/j.neulet.2015.01.072.
Kim DH, Choi KH, Kim HM, Koo JH, Kim BR, Kim TW, et al. Inter-rater reliability of videofluoroscopic dysphagia scale. Ann Rehabil Med. 2012;36:791–6. https://doi.org/10.5535/arm.2012.36.6.791.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration–aspiration scale. Dysphagia. 1996;11:93–8. https://doi.org/10.1007/BF00417897.
Colodny N. Interjudge and intrajudge reliabilities in fiberoptic endoscopic evaluation of swallowing (fees) using the penetration–aspiration scale: a replication study. Dysphagia. 2002;17:308–15. https://doi.org/10.1007/s00455-002-0073-4.
O’Neil KH, Purdy M, Falk J, Gallo L. The dysphagia outcome and severity scale. Dysphagia. 1999;14:139–45. https://doi.org/10.1007/pl00009595.
Wesling M, Brady S, Jensen M, Nickell M, Statkus D, Escobar N. Dysphagia outcomes in patients with brain tumors undergoing inpatient rehabilitation. Dysphagia. 2003;18:203–10. https://doi.org/10.1007/s00455-002-0098-8.
Sims JR, Gharai LR, Schaefer PW, Vangel M, Rosenthal ES, Lev MH, Schwamm LH. ABC/2 for rapid clinical estimate of infarct, perfusion, and mismatch volumes. Neurology. 2009;72:2104–10. https://doi.org/10.1212/WNL.0b013e3181aa5329.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. Am J Roentgenol. 1987;149:351–6. https://doi.org/10.2214/ajr.149.2.351.
Pantoni L, Simoni M, Pracucci G, Schmidt R, Barkhof F, Inzitari D. Visual rating scales for age-related white matter changes (leukoaraiosis): can the heterogeneity be reduced? Stroke. 2002;33:2827–33.
Meyer BC, Hemmen TM, Jackson CM, Lyden PD. Modified National Institutes of Health Stroke Scale for use in stroke clinical trials: prospective reliability and validity. Stroke. 2002;33:1261–6. https://doi.org/10.1161/01.STR.0000015625.87603.A7.
Park J, Kwon Y. Standardization of Korean of the Korean Mini-Mental State Examination (K-MMSE) for use in the elderly: part II, diagnostic validity. J Korean Neuropsychiatr Assoc. 1989;28:508–13.
Fayazi M, Dehkordi SN, Dadgoo M, Salehi M. Test-retest reliability of motricity index strength assessments for lower extremity in post stroke hemiparesis. Med J Islam Repub Iran. 2012;26:27–30.
Kumar S, Doughty C, Doros G, Selim M, Lahoti S, Gokhale S, Schlaug G. Recovery of swallowing after dysphagic stroke: an analysis of prognostic factors. J Stroke Cerebrovasc Dis. 2014;23:56–62. https://doi.org/10.1016/j.jstrokecerebrovasdis.2012.09.005.
Ickenstein GW, Kelly PJ, Furie KL, Ambrosi D, Rallis N, Goldstein R, Horick N, Stein J. Predictors of feeding gastrostomy tube removal in stroke patients with dysphagia. J Stroke Cerebrovasc Dis. 2003;12:169–74. https://doi.org/10.1016/s1052-3057(03)00077-6.
Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, Pedace C, Lenzi L. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009;18:329–35. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.01.009.
Moon HI, Yoon SY, Yi TI, Jeong YJ, Cho TH. Lesions responsible for delayed oral transit time in post-stroke dysphagia. Dysphagia. 2017;33:321–8. https://doi.org/10.1007/s00455-017-9856-5.
Smithard DG, O’Neill PA, Martin DF, England R. Aspiration following stroke: is it related to the side of the stroke? Clin Rehabil. 1997;11:73–6. https://doi.org/10.1177/026921559701100111.
Suntrup S, Kemmling A, Warnecke T, Hamacher C, Oelenberg S, Niederstadt T, Heindel W, Wiendl H, Dziewas R. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 1: dysphagia incidence, severity and aspiration. Eur J Neurol. 2015;22:832–8. https://doi.org/10.1111/ene.12670.
Daniels SK, Pathak S, Mukhi SV, Stach CB, Morgan RO, Anderson JA. The relationship between lesion localization and dysphagia in acute stroke. Dysphagia. 2017;32:777–84. https://doi.org/10.1007/s00455-017-9824-0.
Galovic M, Leisi N, Muller M, Weber J, Abela E, Kägi G, Weder B. Lesion location predicts transient and extended risk of aspiration after supratentorial ischemic stroke. Stroke. 2013;44:2760–7. https://doi.org/10.1161/strokeaha.113.001690.
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010;41:482–6. https://doi.org/10.1161/strokeaha.109.566133.
Lin Q, Huang WQ, Ma QL, Lu CX, Tong SJ, Ye JH, et al. Incidence and risk factors of leukoaraiosis from 4683 hospitalized patients: a cross-sectional study. Medicine. 2017;96:e7682. https://doi.org/10.1097/md.0000000000007682.
Pantoni L, Garcia JH. Pathogenesis of leukoaraiosis: a review. Stroke. 1997;28:652–9. https://doi.org/10.1161/01.STR.28.3.652.
Poggesi A, Gouw A, van der Flier W, Pracucci G, Chabriat H, Erkinjuntti T. Cerebral white matter changes are associated with abnormalities on neurological examination in non-disabled elderly: the LADIS study. J Neurol. 2013;260:1014–21. https://doi.org/10.1007/s00415-012-6748-3.
Viana-Baptista M, Bugalho P, Jordao C, Ribeiro O, Esperanca-Pina JA, Ferro J. Motor dysfunction correlates with frontal white matter ischemic changes in patients with leukoaraiosis. J Aging Res. 2011;2011:950341. https://doi.org/10.4061/2011/950341.
Blahak C, Baezner H, Pantoni L, Poggesi A, Chabriat H, Erkinjuntti T. Deep frontal and periventricular age related white matter changes but not basal ganglia and infratentorial hyperintensities are associated with falls: cross sectional results from the LADIS study. J Neurol Neurosurg Psychiatry. 2009;80:608–13. https://doi.org/10.1136/jnnp.2008.154633.
Levine R, Robbins JA, Maser A. Periventricular white matter changes and oropharyngeal swallowing in normal individuals. Dysphagia. 1992;7:142–7. https://doi.org/10.1007/BF02493446.
Afifi AK, Bergman RA. Functional neuroanatomy: text and atlas, ix. New York: Lange Medical Books/McGraw-Hill; 2005.
Pan C, Peck KK, Young RJ, Holodny AI. Somatotopic organization of motor pathways in the internal capsule: a probabilistic diffusion tractography study. AJNR Am J Neuroradiol. 2012;33:1274–80. https://doi.org/10.3174/ajnr.A2952.
Galovic M, Leisi N, Pastore-Wapp M, Zbinden M, Vos SB, Mueller M, et al. Diverging lesion and connectivity patterns influence early and late swallowing recovery after hemispheric stroke. Hum Brain Mapp. 2017;38:2165–76. https://doi.org/10.1002/hbm.23511.
Kwon HG, Lee J, Jang SH. Injury of the corticobulbar tract in patients with dysarthria following cerebral infarct: diffusion tensor tractography study. Int J Neurosci. 2016;126:361–5. https://doi.org/10.3109/00207454.2015.1020536.
Cho SH, Kim DG, Kim DS, Kim YH, Lee CH, Jang SH. Motor outcome according to the integrity of the corticospinal tract determined by diffusion tensor tractography in the early stage of corona radiata infarct. Neurosci Lett. 2007;426:123–7. https://doi.org/10.1016/j.neulet.2007.08.049.
Koyama T, Marumoto K, Miyake H, Domen K. Relationship between diffusion tensor fractional anisotropy and motor outcome in patients with hemiparesis after corona radiata infarct. J Stroke Cerebrovasc Dis. 2013;22:1355–60. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.02.01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ko, E.J., Choi, K.H. & Kwon, S.U. The Relationship Between Leukoaraiosis Involving Contralateral Corticobulbar Tract and Dysphagia in Patients with Acute Unilateral Corona Radiata Infarction with Corticobulbar Tract Involvement. Dysphagia 34, 654–664 (2019). https://doi.org/10.1007/s00455-018-9963-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9963-y