Abstract
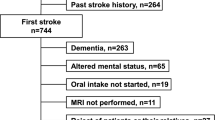
Factors that can facilitate early identification of individuals at risk of dysphagia such as stroke location are potentially of great benefit. The aim of this study was to examine the role of hemisphere and lesion location in assessing dysphagia pattern and airway invasion as identified through the use of validated, standardized interpretation measures for the videofluoroscopic swallowing study. Consecutive patients (N = 80) presenting with stroke symptoms who had a first-time acute ischemic stroke confirmed on diffusion-weighted magnetic resonance imaging (DW-MRI) scan participated. Three swallowing outcome variables were assessed using regression models: modified barium swallow impairment profile (MBSImP) oral impairment (OI) and pharyngeal impairment (PI) scores and penetration aspiration scale (PAS) score. Subjects were primarily male and demonstrated mild stroke and mild to moderate dysphagia. There was a significantly higher likelihood of abnormal PAS scores for infratentorial lesions compared to right hemisphere location (Odds ratio: 3.1, SE: 1.8, p = 0.046) and for Whites compared to African Americans (Odds ratio: 5.5, SE: 2.6, p = <0.001). However, OI scores were higher (worse) in African Americans compared to Whites (Beta = −1.2; SE: 0.56; p = 0.037). PI scores had no significant association with race or lesion location. Using DW-MRI to identify infratentorial stroke can help identify individuals at risk of airway invasion; however, imaging information concerning supratentorial infarct hemisphere and location may not be useful to predict which individuals with mild stroke are at risk for dysphagia and aspiration when admitted with acute stroke symptoms. Future studies should explore the role of race in the development of stroke-related dysphagia.

Similar content being viewed by others
References
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63. doi:10.1161/01STR.0000190056.76543.eb.
Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005;36:1972–6. doi:10.1161/01.STR.0000177529.86868.8d.
Odderson IR, McKenna BS. A model for management of patients with stroke during the acute phase. Outcomes and economic implications. Stroke. 1993;24:1823–7. doi:10.1161/01.STR.24.12.1823.
Martino R, Pron G, Diamont N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidance. Dysphagia. 2000;15:19–30. doi:10.1007/s004559910006.
Daniels SK, Foundas AL. Lesion localization in acute stroke. J Neuroimaging. 1999;9:91–8. doi:10.1111/jon19999291.
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010;41:482–6. doi:10.1161/STROKEAHA.109.566133.
Gonzalez-Fernandez M, Kleinman JT, Ky PKS, Palmer JB, Hillis AE. Supratentorial regions of acute ischemia associated with clinically important swallowing disorders. Stroke. 2008;39:3022–8. doi:10.1161/STROKE.AHA.108.518969.
Galovic M, Leisi N, Muller M, Weber J, Abela E, Kagi G, Weder B. Lesion location predicts transient and extended risk of aspiration after supratentorial ischemic stroke. Stroke. 2013;44:2760–7. doi:10.1161/STROKE.AHA.113.001690.
Suntrup S, Kemmling A, Warnecke T, Hamacher C, Oelenber S, Niederstadt T, Heindel W, Wiendl H, Dziewas R. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 1: dysphagia incidence, severity, and aspiration. Eur J Neurol. 2015;22:832–8. doi:10.1111/ene.12670.
Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, Pedace C, Lenzi L. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009;18:329–35. doi:10.1016/j.jstrokecerebrovasdis.2009.01.009.
Daniels SK, Foundas AL, Iglesia GC, Sullivan MA. Lesion site in unilateral stroke patients with dysphagia. J Stroke Cerebrovasc Dis. 1996;6:30–4. doi:10.1016/S1052-3057(96)80023-1.
Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993;74:1295–300. doi:10.1016/0003-9993(93)90082-L.
Alberts MJ, Horner J, Gray L, Brazer SR. Aspiration after stroke: lesion analysis by brain MRI. Dysphagia. 1992;7:170–3. doi:10.1007/BF02493452.
Jeon WH, Park GW, Lee JH, Jeong HJ, Sim YJ. Association between location of brain lesion and clinical factors and findings of videofluoroscopic swallowing study in subacute stroke patients. Brain Neurorehabil. 2014;7:54–60. doi:10.12786/bn.2014.7.1.54.
Daniels SK, Pathak S, Rosenbek JC, Morgan RO, Anderson JA. Rapid aspiration screening for suspected stroke: part 1: development and validation. Arch Phys Med Rehabil. 2016;97:1440–8. doi:10.1016/j.apmr.2016.03.025.
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J. MBS Measurement tool for swallow impairment-MBSImP: establishing a standard. Dysphagia. 2008;23:392–405. doi:10.1007/s00455-008-9185-9.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8. doi:10.1007/BF00417897.
Vatcheva KP, Lee MJ, Mccormick JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiological studies. Epidemiology (Sunnyvale). 2016;6(2):227. doi:10.4172/2161-1165.1000227.
Vander Weele TJ, Robinson WR. On causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology (Cambridge). 2014;25:473–84. doi:10.1097/EDE.0000000000000105.
Miller AJ. The neuroscientific principles of swallowing and dysphagia. San Diego: Singular; 1999.
Kessler JP, Jean A. Identification of the medullary swallowing regions in rats. Exp Brain Res. 1985;57:256–63. doi:10.1007/BF00236530.
Jean A. Brain control of swallowing: neuronal network and cellular mechanisms. Physiol Rev. 2001;81:929–69.
Flowers HL, Skoretz SA, Streiner DL, Silver FL, Martino R. MRI-based neuroanatomical predictors of dysphagia after acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2011;32:1–10. doi:10.1159/000324940.
Vansant DH, Hamdy S. Cerebral cortical control of deglutition. In: Shaker R, Belafsky PC, Postma GN, Easterling C, editors. Principles of deglutition. New York: Springer; 2013.
Gonzalez-Fernandez M, Kuhlemeier KV, Palmer JB. Racial disparities in the development of dysphagia after stroke: analysis of the California (MIRCal) and New York (SPARCS) inpatient databases. Arch Phys Med Rehabil. 2008;89:1358–65. doi:10.1016/j.apmr.2008.02.016.
Bussell SA, Gonzalez-Fernandez M. Racial disparities in the development of dysphagia after stroke: further evidence from the medicare database. Arch Phys Med Rehabil. 2011;92:737–42. doi:10.1016/j.apmr.2010.12.005.
Acknowledgements
The project described was based on work supported by a Merit Award (1I01RX000121) from the Rehabilitation Research & Development Service of the VA Office of Research and Development. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the University of Texas School of Public Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Stephanie K. Daniels, Shweta Pathak, and Robert Morgan received salary support for a grant from the Department of Veterans Affairs. Shalini V. Mukhi, Carol B. Stach, and Jane A. Anderson report no conflict of interest.
Rights and permissions
About this article
Cite this article
Daniels, S.K., Pathak, S., Mukhi, S.V. et al. The Relationship Between Lesion Localization and Dysphagia in Acute Stroke. Dysphagia 32, 777–784 (2017). https://doi.org/10.1007/s00455-017-9824-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9824-0