Abstract
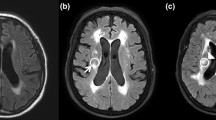
Older patients with stroke have poor functional prognosis compared to younger patients. Patients with stroke who have severe white matter (WM) lesions have been reported to have poor functional prognosis such as cognitive dysfunction, increased propensity for falling, and gait and balance problems. The aim of this study was to determine whether WM lesions exert negative effects on swallowing function in older patients with mild stroke. We conducted a retrospective analysis of 63 patients aged >65 years who had a National Institutes of Health Stroke Scale score ≤5 and who underwent videofluoroscopic swallowing examination after their first stroke. Linear regression analysis showed that oral transit time tended to increase as Fazekas grade increased (p = 0.003). In addition, inadequate mastication was related to the presence of lesions in the left hemisphere (p = 0.039). The presence of penetration could also be predicted by Fazekas grade (p = 0.015). Our findings suggest that WM lesions observed in brain magnetic resonance imaging scans can impact swallowing problems in older patients with mild stroke, regardless of initial stroke severity or other factors associated with lesion location. Accordingly, our data indicate that WM lesions are a predictive factor by which patients can be stratified into favorable or unfavorable outcomes with respect to dysphagia.


Similar content being viewed by others
References
Denti L, Scoditti U, Tonelli C, Saccavini M, Caminiti C, Valcavi R, et al. The poor outcome of ischemic stroke in very old people: a cohort study of its determinants. J Am Geriatr Soc. 2010;58(1):12–7.
Kammersgaard LP, Jorgensen HS, Reith J, Nakayama H, Pedersen PM, Olsen TS, et al. Short- and long-term prognosis for very old stroke patients. The copenhagen stroke study. Age Ageing. 2004;33(2):149–54.
Feigin VL, Barker-Collo S, Parag V, Senior H, Lawes CM, Ratnasabapathy Y, et al. Auckland stroke outcomes study. part 1: gender, stroke types, ethnicity, and functional outcomes 5 years poststroke. Neurology. 2010;75(18):1597–607.
Shi Q, Presutti R, Selchen D, Saposnik G. Delirium in acute stroke: a systematic review and meta-analysis. Stroke. 2012;43(3):645–9.
Forti P, Maioli F, Procaccianti G, Nativio V, Lega MV, Coveri M, et al. Independent predictors of ischemic stroke in the elderly: prospective data from a stroke unit. Neurology. 2013;80(1):29–38.
Liou LM, Chen CF, Guo YC, Cheng HL, Lee HL, Hsu JS, et al. Cerebral white matter hyperintensities predict functional stroke outcome. Cerebrovasc Dis. 2010;29(1):22–7.
Sonohara K, Kozaki K, Akishita M, Nagai K, Hasegawa H, Kuzuya M, et al. White matter lesions as a feature of cognitive impairment, low vitality and other symptoms of geriatric syndrome in the elderly. Geriatr Gerontol Int. 2008;8(2):93–100.
Srikanth V, Beare R, Blizzard L, Phan T, Stapleton J, Chen J, et al. Cerebral white matter lesions, gait, and the risk of incident falls: a prospective population-based study. Stroke. 2009;40(1):175–80.
Inzitari D, Pracucci G, Poggesi A, Carlucci G, Barkhof F, Chabriat H, et al. Changes in white matter as determinant of global functional decline in older independent outpatients: three year follow-up of LADIS (leukoaraiosis and disability) study cohort. BMJ. 2009;339:b2477.
Levine R, Robbins JA, Maser A. Periventricular white matter changes and oropharyngeal swallowing in normal individuals. Dysphagia. 1992;7(3):142–7.
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010;41(3):482–6.
Fandler S, Gattringer T, Eppinger S, Doppelhofer K, Pinter D, Niederkorn K. Frequency and predictors of dysphagia in patients with recent small subcortical infarcts. Stroke. 2016;48(1):213–5.
Shaker R. Principles of deglutition: a multidisciplinary text for swallowing and its disorders. New York: Springer; 2013.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–63.
Leslie P, Drinnan MJ, Ford GA, Wilson JA. Swallow respiratory patterns and aging: presbyphagia or dysphagia? J Gerontol A Biol Sci Med Sci. 2005;60(3):391–5.
Aviv JE. Effects of aging on sensitivity of the pharyngeal and supraglottic areas. Am J Med. 1997;103(5A):74S–6S.
Cook IJ, Weltman MD, Wallace K, Shaw DW, McKay E, Smart RC, et al. Influence of aging on oral-pharyngeal bolus transit and clearance during swallowing: scintigraphic study. Am J Physiol. 1994;266(6 Pt 1):G972–7.
Achem SR, Devault KR. Dysphagia in aging. J Clin Gastroenterol. 2005;39(5):357–71.
Daggett A, Logemann J, Rademaker A, Pauloski B. Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia. 2006;21(4):270–4.
Lee KM, Jang YH, Kim YH, Moon SK, Park JH, Park SW, Yu HJ, Lee SG, Chun MH, Han TR. Reliability and validity of Korean version of national institutes of health stroke scale. J Korean Acad Rehab Med. 2004;28:422–35.
Logemann JA. Swallowing physiology and pathophysiology. Otolaryngol Clin North Am. 1988;21(4):613–23.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Yokoyama M, Mitomi N, Tetsuka K, Tayama N, Niimi S. Role of laryngeal movement and effect of aging on swallowing pressure in the pharynx and upper esophageal sphincter. Laryngoscope. 2000;110(3 Pt 1):434–9.
Rademaker AW, Pauloski BR, Colangelo LA, Logemann JA. Age and volume effects on liquid swallowing function in normal women. J Speech Lang Hear Res. 1998;41(2):275–84.
McKee GJ, Johnston BT, McBride GB, Primrose WJ. Does age or sex affect pharyngeal swallowing? Clin Otolaryngol Allied Sci. 1998;23(2):100–6.
Nilsson H, Ekberg O, Olsson R, Hindfelt B. Quantitative aspects of swallowing in an elderly nondysphagic population. Dysphagia. 1996;11(3):180–4.
Toscano M, Cecconi E, Capiluppi E, Vigano A, Bertora P, Campiglio L, et al. Neuroanatomical, clinical and cognitive correlates of post-stroke dysphagia. Eur Neurol. 2015;74(3–4):171–7.
Murray ME, Vemuri P, Preboske GM, Murphy MC, Schweitzer KJ, Parisi JE, et al. A quantitative postmortem MRI design sensitive to white matter hyperintensity differences and their relationship with underlying pathology. J Neuropathol Exp Neurol. 2012;71(12):1113–22.
Mitchell GF. Effects of central arterial aging on the structure and function of the peripheral vasculature: implications for end-organ damage. J Appl Physiol. 2008;105(5):1652–60.
Bisschops RH, van der Graaf Y, Mali WP, van der Grond J, group Ss. High total cerebral blood flow is associated with a decrease of white matter lesions. J Neurol. 2004;251(12):1481–5.
Nudo RJ. Postinfarct cortical plasticity and behavioral recovery. Stroke. 2007;38(2 Suppl):840–5.
Madden DJ, Bennett IJ, Song AW. Cerebral white matter integrity and cognitive aging: contributions from diffusion tensor imaging. Neuropsychol Rev. 2009;19(4):415–35.
Gunning-Dixon FM, Brickman AM, Cheng JC, Alexopoulos GS. Aging of cerebral white matter: a review of MRI findings. Int J Geriatr Psychiatry. 2009;24(2):109–17.
de Groot M, Ikram MA, Akoudad S, Krestin GP, Hofman A, van der Lugt A, et al. Tract-specific white matter degeneration in aging: the Rotterdam Study. Alzheimers Dement. 2015;11(3):321–30.
Moon HI, Choi SY, Tae WS, Pyun SB. Effects of age on cortical activation during swallowing: an fMRI study. J Korean Dysphagia Soc. 2016;6(1):26–33.
Martin R, Barr A, MacIntosh B, Smith R, Stevens T, Taves D, et al. Cerebral cortical processing of swallowing in older adults. Exp Brain Res. 2007;176(1):12–22.
Humbert IA, Fitzgerald ME, McLaren DG, Johnson S, Porcaro E, Kosmatka K, et al. Neurophysiology of swallowing: effects of age and bolus type. Neuroimage. 2009;44(3):982–91.
van den Heuvel DM, ten Dam VH, de Craen AJ, Admiraal-Behloul F, Olofsen H, Bollen EL, et al. Increase in periventricular white matter hyperintensities parallels decline in mental processing speed in a non-demented elderly population. J Neurol Neurosurg Psychiatry. 2006;77(2):149–53.
Wright CB, Festa JR, Paik MC, Schmiedigen A, Brown TR, Yoshita M, et al. White matter hyperintensities and subclinical infarction: associations with psychomotor speed and cognitive flexibility. Stroke. 2008;39(3):800–5.
Secil Y, Arici S, Incesu TK, Gurgor N, Beckmann Y, Ertekin C. Dysphagia in Alzheimer’s disease. Neurophysiol Clin. 2016;46(3):171–8.
Boccardi V, Ruggiero C, Patriti A, Marano L. Diagnostic assessment and management of dysphagia in patients with Alzheimer’s disease. J Alzheimers Dis. 2016;50(4):947–55.
Rosler A, Pfeil S, Lessmann H, Hoder J, Befahr A, von Renteln-Kruse W. Dysphagia in dementia: influence of dementia severity and food texture on the prevalence of aspiration and latency to swallow in hospitalized geriatric patients. J Am Med Dir Assoc. 2015;16(8):697–701.
Suh MK, Kim H, Na DL. Dysphagia in patients with dementia: alzheimer versus vascular. Alzheimer Dis Assoc Disord. 2009;23(2):178–84.
Lee CK, Kim JA. Pattern of post-stroke swallowing disorder according to the brain lesion. J Korean Acad Rehab Med. 2001;25:193–201.
Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009;40(5):1903–6.
Graff-Radford J, Jones DT, Strand EA, Rabinstein AA, Duffy JR, Josephs KA. The neuroanatomy of pure apraxia of speech in stroke. Brain Lang. 2014;129:43–6.
Wakasugi Y, Tohara H, Hattori F, Motohashi Y, Nakane A, Goto S, et al. Screening test for silent aspiration at the bedside. Dysphagia. 2008;23(4):364–70.
Martino R, Silver F, Teasell R, Bayley M, Nicholson G, Streiner DL, et al. The toronto bedside swallowing screening test (TOR-BSST): development and validation of a dysphagia screening tool for patients with stroke. Stroke. 2009;40(2):555–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no potential conflicts of interest to declare with respect to the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Moon, H.I., Nam, JS., Leem, M.J. et al. Periventricular White Matter Lesions as a Prognostic Factor of Swallowing Function in Older Patients with Mild Stroke. Dysphagia 32, 480–486 (2017). https://doi.org/10.1007/s00455-017-9788-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9788-0