Abstract
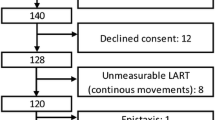
Laryngeal sensitivity is crucial for maintaining safe swallowing, thus avoiding silent aspiration. The sensitivity test, carried out by fiberoptic endoscopic examination of swallowing, plays an important role in the assessment of dysphagic patients. The ventricular folds appear to be more sensitive than the epiglottis during the sensitivity test. Therefore, this study aimed to investigate the mechanical sensitivity of the supraglottic larynx. In seven healthy adults undergoing microlaryngoscopy to remove vocal cord polyps, we excised mucosal samples from the epiglottis and ventricular folds. We measured afferent nerve fiber density by immunoelectron microscopy. All of the subjects underwent an endoscopic sensitivity test based on lightly touching the laryngeal surface of the epiglottis and ventricular folds. The discomfort level was self-rated by the subjects on the visual analog scale. Samples were fixed and stored in cryoprotectant solution at 4 °C. Sections were stained with the protein gene product 9.5, a pan-neuronal selective marker. Nerve fiber density was calculated as the number of fibers per millimeter length of section. The mean nerve fiber density was higher in ventricular samples than in epiglottis samples (2.96 ± 2.05 vs 0.83 ± 0.51; two-sided p = 0.018). The mean visual analog scale scores were significantly higher for touching the ventricular folds than for touching the epiglottis (8.28 ± 1.11 vs 4.14 ± 1.21; two-sided p = 0.017). The higher sensitivity of the ventricular region should be considered for further refining clinical endoscopic evaluation of laryngeal sensitivity.

Similar content being viewed by others
References
Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, Loesche WJ. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998;13:69–81.
Aviv JE, Sacco RL, Thomson J, Tandon R, Diamond B, Martin JH, Close LG. Silent laryngopharyngeal sensory deficits after stroke. Ann Otol Rhinol Laryngol. 1997;106:87–93.
Wakasugi Y, Tohara H, Hattori F, Motohashi Y, Nakane A, Goto S, Ouchi Y, Mikushi S, Takeuchi S, Uematsu H. Screening test for silent aspiration at the bedside. Dysphagia. 2008;23:364–70.
Miles A, Moore S, McFarlane M, Lee F, Allen J, Huckabee ML. Comparison of cough reflex test against instrumental assessment of aspiration. Physiol Behav. 2013;118:25–31.
Miles A, Zeng IS, McLauchlan H, Huckabee ML. Cough reflex testing in dysphagia following stroke: a randomized controlled trial. J Clin Med Res. 2013;5:222–335.
Colodny N. Interjudge and intrajudge reliabilities in fiberoptic endoscopic evaluation of swallowing (FEES) using the penetration-aspiration scale: a replication study. Dysphagia. 2002;17:308–15.
Addington WR, Stephens RE, Gilliland KA. Assessing the laryngeal cough reflex and the risk of developing pneumonia after stroke: an interhospital comparison. Stroke. 1999;30:1203–7.
Stephens RE, Wendel KH, Addington WR. Anatomy of the internal branch of the superior laryngeal nerve. Clin Anat. 1999;12:79–83.
Villaverde R, Pastor LM, Calvo A, Ferrán A, Sprekelsen C. Nerve endings in the epithelium and submucosa of human epiglottis. Acta Otolaryngol. 1994;114:453–7.
Aviv JE. Effects of aging on sensitivity of the pharyngeal and supraglottic areas. Am J Med. 1997;103:74S–6S.
Boushey HA, Richardson PS, Widdicombe JG, Wise JC. The response of laryngeal afferent fibres to mechanical and chemical stimuli. J Physiol. 1974;240:153–75.
Nelson M, Cooper DM, Lawson W. Laryngeal sensory receptors. In: Blitzer A, Brin MF, Ramig OR, editors. Neurologic disorders of the larynx. New York: Thieme; 2009. p. 10–20.
Shin T, Watanabe S, Wada S, Maeyama T. Sensory nerve endings in the mucosa of the epiglottis—morphologic investigations with silver impregnation, immunohistochemistry, and electron microscopy. Otolaryngol Head Neck Surg. 1987;96:55–62.
Domeij S, Dahlqvist A, Forsgren S. Regional differences in the distribution of nerve fibers showing substance P- and calcitonin gene-related peptide-like immunoreactivity in the rat larynx. Anat Embryol. 1991;183:49–56.
Yamamoto Y, Tanaka S, Tsubone H, Atoji Y, Suzuki Y. Age-related changes in sensory and secretomotor nerve endings in the larynx of F344/N rat. Arch Gerontol Geriatr. 2003;36:173–83.
Esaki H, Umezaki T, Takagi S, Shin T. Characteristics of laryngeal receptors analyzed by presynaptic recording from the cat medulla oblongata. Auris Nasus Larynx. 1997;24:73–83.
Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2:216–9.
Aviv JE, Kim T, Thomson JE, Sunshine S, Kaplan S, Close LG. Fiberoptic endoscopic evaluation of swallowing with sensory testing (FEESST) in healthy controls. Dysphagia. 1998;13:87–92.
Aviv JE, Kim T, Sacco RL, Kaplan S, Goodhart K, Diamond B, Close LG. FEESST: a new bedside endoscopic test of the motor and sensory components of swallowing. Ann Otol Rhinol Laryngol. 1998;107:378–87.
Hiss SG, Postma GN. Fiberoptic endoscopic evaluation of swallowing. Laryngoscope. 2003;113:1386–93.
Thompson RJ, Doran JF, Jackson P, Dhillon AP, Rode J. PGP 9.5 a new marker for vertebrate neurons and neuroendocrine cells. Brain Res. 1983;278:224–8.
Gulbenkian S, Wharton J, Polak JM. The visualization of cardiovascular innervation in the guinea pig using an antiserum to protein gene product 9.5 (PGP 9.5). J Auton Nerv Syst. 1987;18:235–47.
Lundberg LM, Alm P, Wharton J, Polak JM. Protein gene product 9.5 (PGP 9.5). A new neuronal marker visualizing the whole uterine innervation and pregnancy-induced and developmental changes in the guinea pig. Histochemistry. 1988;90:9–17.
Setzen M, Cohen M, Mattucci KF, Perlman PW, Ditkoff MK. Laryngopharyngeal sensory deficits as a predictor of aspiration. Otolaryngol Head Neck Surg. 2001;124:622–4.
Aviv JE, Spitzer J, Cohen M, Ma G, Belafsky P, Close LG. Laryngeal adductor reflex and pharyngeal squeeze as predictor of laryngeal penetration and aspiration. Laryngoscope. 2002;112:338–41.
Gøransson LG, Mellgren SI, Lindal S, Omdal R. The effect of age and gender on epidermal nerve fiber density. Neurology. 2004;62:774–7.
Umapathi T, Tan WL, Tan NC, Chan YH. Determinants of epidermal nerve fiber density in normal individuals. Muscle Nerve. 2006;33:742–6.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruoppolo, G., Schettino, I., Biasiotta, A. et al. Afferent Nerve Ending Density in the Human Laryngeal Mucosa: Potential Implications on Endoscopic Evaluation of Laryngeal Sensitivity. Dysphagia 30, 139–144 (2015). https://doi.org/10.1007/s00455-014-9589-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-014-9589-7